|
 |
- Search
| Asian Spine J > Volume 7(4); 2013 > Article |
Abstract
Study Design
A nation-wide, outpatient-based, cross-sectional survey with the use of questionnaires.
Purpose
To evaluate the pain, disability and satisfaction of patients with osteoporotic vertebral compression fractures (OVCFs).
Overview of Literature
There are no nation-wide data in Korea on the degree of pain, disability and satisfaction with treatment in patients with OVCFs.
Methods
We performed a cross-sectional survey of 573 patients with OVCFs. After excluding incomplete questionnaires (missing more than 30% of the variables), 430 patient-physician-matched data sets were collected for this survey.
Results
Patients with OVCFs were managed with conservative treatment in 63% and with a vertebroplasty in 37%. The means of the latest visual analogue scale (VAS, 5.2) and Oswestry Disability Index (ODI, 47.7) scores checked at the time of survey were significantly higher than those VAS and ODI scores prior to OVCFs (the prefracture VAS and ODI scores, 3.6 and 26.3, respectively; p<0.001 for both comparisons). However, the means of the latest VAS and ODI scores were insignificantly different between the conservative and vertebroplasty groups, irrespective of the duration from the fractures. Overall, 75% of patients were satisfied with their clinical outcomes. However, the percentages of patient's satisfaction were not significantly different between the conservative and vertebroplasty groups. Eighty-eight percent of patients felt some or marked deterioration of their general health condition following OVCFs.
Osteoporotic vertebral compression fractures (OVCFs) are the most common complication of osteoporosis. Although previous studies have shown that OVCFs may be a minor problem in some patients, they may significantly impair the physical function and quality of life in other patients [1-6]. In some of the latter patients for whom conservative management fails, minimal invasive interventions, such as vertebroplasty and kyphoplasty, may provide early improvement of their pain and function [7-10].
With increasing life expectancy, osteoporosis is currently one of the major medical conditions affecting the aged population in Korea [11]. Accordingly, the number of patients with OVCFs is believed to have steeply increased during the last decade [12]. In addition, the unofficial market research in Korea has found that there appears to be an exponential increase in the use of vertebroplasty for the management of OVCFs as an alternative to conservative treatment [9,13]. However, we do not yet have our own nation-wide data on the degree of pain, disability and satisfaction with treatment in patients with OVCFs. Thus, the academic committee of the Korean Society of Spine Surgery (KSSS) with collaboration with the Korea Yasen Pharmacy decided to conduct a nation-wide, outpatient-based survey to evaluate the pain, disability and satisfaction of patients with OVCFs.
We performed a cross-sectional survey of 573 patients with OVCFs, who were being managed by the members of the KSSS at secondary or tertiary hospitals located in each of the nine provinces in our country. Patients were diagnosed as having OVCFs if they had OVCFs with at least two of the following criteria: a) at least one of the T-scores of lumbar spinal bone mineral densities (BMDs) on a dual-energy X-ray absorptiometry was less than -2.5; b) patients were older than 65 years; and c) there was a loss of transverse trabecula in the vertebral body on the lateral plain radiograph. The exclusion criteria were as follow: 1) patients who had neurological deficits related to OVCFs, 2) patients who underwent instrumented stabilization surgery for OVCFs, 3) the patients who had received joint replacement arthroplasty in the lower extremities prior to OVCFs, and 4) patients who had had a gait disturbance for any reasons prior to OVCFs.
At the time of the latest visit to the outpatient clinics, patients and treating surgeons filled out the OVCF questionnaires (Table 1). Volunteers, who were unaware of the purpose of this survey, assisted all patients in filling out the questionnaires. The surgeon's questionnaires consisted of the following; 1) patient information: age, gender and body mass index (BMI=weight [kg]/height2 [m]; underweight <18.5, normal=18.5-22.9, and overweight ≥23); 2) the lowest lumbar spinal BMD value; 3) the history of anti-osteoporosis medication prior to fractures; 4) the fracture location (thoracic [T1-T10], thoracolumbar [T11-L2], lumbar [L3-L5]). When a patient had VCFs in more than two locations or more than two vertebrae in a location, the most severely compressed or kyphotic vertebra was chosen for this survey; 5) the management methods (conservative treatment or vertebroplasty). 6) the percentage of vertebral height loss (Fig. 1A); and finally, 7) the wedge angle (Fig. 1B). Patient's questionnaires consisted of 1) the residence area (urban or rural); 2) the work state (employed or unemployed); 3) the presence or absence of definite traumatic events at the time of VCF (fall from height, fall by slipping, traffic accident, etc.); 4) the visual analogue scale (VAS) for pain prior to fracture (prefracture VAS) and at the time of survey (the latest VAS), respectively (for the prefracture VAS scores, only the patients who were able to precisely remember their pain status prior to fracture recorded these scores.); 5) the Oswestry Disability Index (ODI) scores prior to fracture (prefracture ODI) and at the time of the survey (the latest ODI), (for the prefracture ODI, only the patients who were able to precisely remember their disability status prior to fracture recorded these scores); 6) the duration from the OVCF to the time of survey (≤4 months, 5-8 months, 9-12 months or >12 months); 7) patient's subjective satisfaction or dissatisfaction with their clinical outcomes; and 8) patient's subjective feeling on their general health conditions, following OVCFs: (no/somewhat/marked) deterioration compared with the prefracture status.
The variables were analyzed 1) to compare the prefracture VAS and ODI scores with the latest VAS and ODI scores (paired t-test), 2) to compare the latest VAS and ODI scores between the conservative and vertebroplasty groups at each duration from the OVCF to the time of survey (independent samples t-test), 3) to compare the number of patients who were satisfied or dissatisfied with their clinical outcomes between the conservative and vertebroplasty groups (chi-square test), and 4) to determine which of the variables significantly affected the patient's satisfaction (multiple logistic regression analysis with variable selection using a backward elimination method); the variables included in this analysis were gender, residence (urban or rural), work state (employed or unemployed), BMD, BMI (underweight, normal or overweight), trauma history (yes or no), location of OVCFs (thoracic, thoracolumbar or lumbar), duration from OVCFs to the time of survey (≤4 months, 5-8 months, 9-12 months or >12 months), anti-osteoporosis medications prior to OVCFs (yes or no), treatment method (conservative or vertebroplasty), latest VAS and ODI scores, percentages of vertebral height loss (%) and wedge angle (degrees).
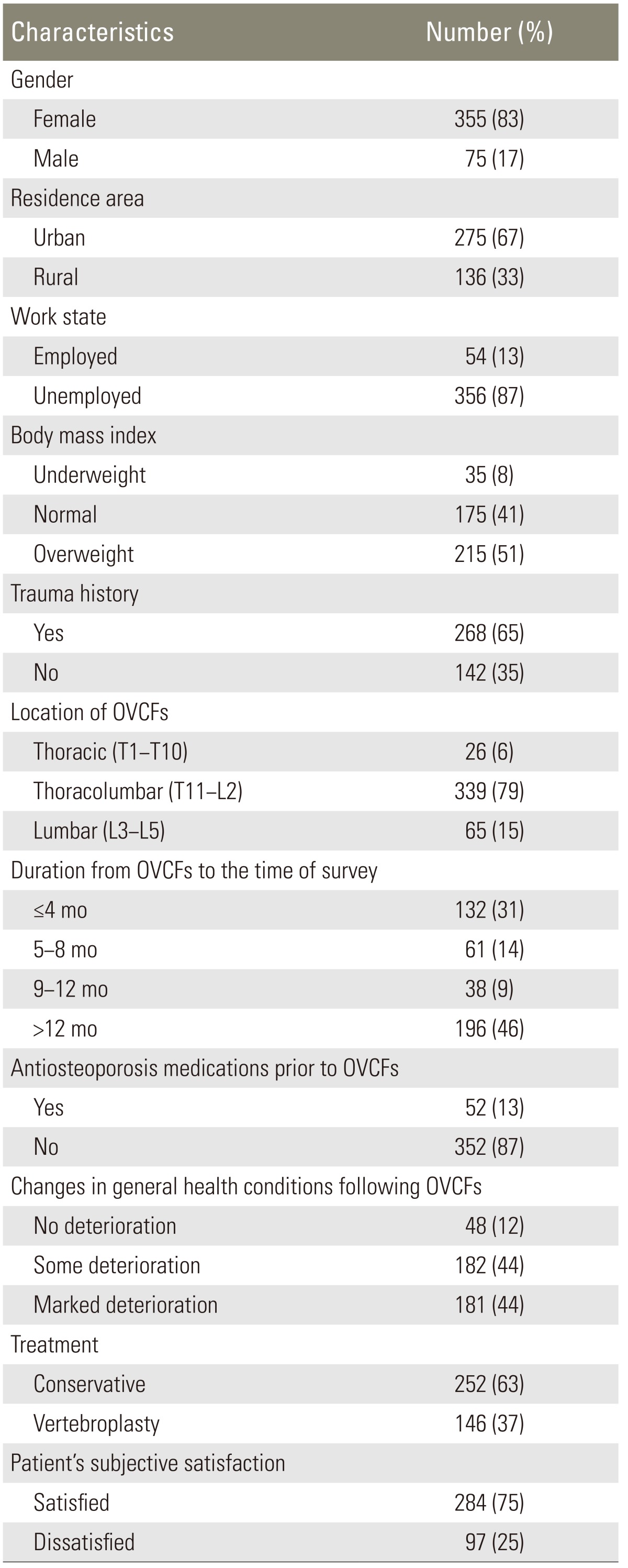
Five hundred seventy-three sets of patient-physician-matched data were compiled. After excluding the questionnaires with incomplete data (missing more than 30% of the variables), a total of 430 sets of data were used for this survey. The summary of results of the questionnaires is listed in Table 1. Of the 430 patients, there were 355 females (83%) and 75 males (17%), with a mean age of 70 years (standard deviation [SD], ±8.6 years). Of the 411 patients, 275 (67%) patients resided in urban areas and 136 (33%) resided in rural areas. Of the 410 patients, 54 (13%) patients were employed and 356 (87%) were unemployed. According to the BMI, 215 of 425 (51%) patients were overweight, 175 (41%) patients were normal, and 35 (8%) patients were underweight. Of the 410 patients, 268 (65%) patients had a definite trauma history, but 142 (35%) patients did not. According to the duration from OVCFs, the fractures (427 patients) occurred four or less months ago (≤4 months) in 132 (31%) patients, and 61 (14%) patients got fractures between five and eight months (5-8 months) ago. In addition, in 38 (9%) patients, factures occurred between 9 and 12 months (9-12 months) ago and more than 12 months (>12 months) ago in 196 (46%) patients. The location of OVCFs (430 patients) was thoracic in twenty-six (6%) patients, thoracolumbar in 339 (79%) patients and lumbar in sixty-five (15%) patients. Three hundred fifty-four of the 404 (87%) patients had not taken any anti-osteoporosis medications prior to OVCFS. Of the 398 patients, 252 (63%) were managed with conservative treatment and 146 (37%) were treated with vertebroplasty. The means of the vertebral height loss and wedge angle at the time of this survey were 33.2% (SD, ±16.5%) and 17.6° (SD, ±7.9°), respectively.
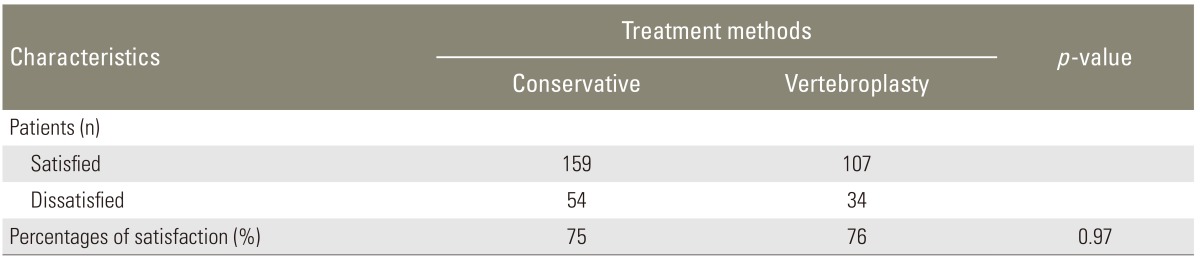
Overall, the latest VAS (5.2) and ODI (47.7) scores were significantly higher than the prefracture VAS (3.6) and ODI (26.3) scores (p<0.001 for both comparisons) (Table 2). The latest VAS and ODI scores were not significantly different between the conservative and vertebroplasty groups, irrespective of the duration from OVCFs (p>0.05 for all comparisons) (Tables 3, 4). Further, 75% (284 of 381) of the patients were satisfied with their clinical outcomes (Table 1). However, a chi-square test showed no significant difference in the number of patients who were satisfied or dissatisfied with their clinical outcomes between the conservative (159 of 213 patients, 75%) and vertebroplasty (107 of 141 patients, 76%) groups (p=0.79) (Table 5). Three hundred sixty-three of the 411 (88%) patients subjectively felt some or marked deterioration of their general health conditions following OVCFs. Multiple logistic regression analysis with variable selection, using a backward elimination method, showed that female gender, patients with lower latest VAS scores, or patients with lesser wedge angle had a tendency to be satisfied with their clinical outcomes (Table 6).
The present survey included patients with OVCFs, who were being managed by members of the KSSS. Our data showed that OVCFs commonly occurred in women and in the thoracolumbar region. Surprisingly, OVCFs developed without definite traumatic events in approximately one third of the patients. The means of the vertebral height loss and wedge angle at the time of survey were 33.2% (SD, ±16.5%) and 17.6° (SD, ±7.9°), respectively.
Conservative treatment, such as a short-term bed rest and early ambulation with a brace, has long been the gold standard for the management of OVCFs in Korea. However, vertebroplasty as an alternative to conservative treatment is assumed to have increased exponentially during the last decade in our country. The academic committee of the KSSS raised a hot issue concerning the exponential increase of vertebroplasty, and they decided to conduct a nation-wide survey to evaluate the current real state of OVCFs that are managed by the members of the KSSS. Our survey showed that approximately two thirds of patients were managed with conservative treatment and the rest were managed with vertebroplasty. The percentages using vertebroplasty were much higher than the committee had expected before this survey. This result indicates that although conservative treatment is still a preferred method, as performed by the members of the KSSS, there is a big change in the management of OVCFs from conservative treatment to vertebroplasty in Korea.
Several studies published in the last decade have advocated vertebroplasty for the management of OVCFs, based on the results from immediate improvement in the functional outcomes of patients with OVCFs following vertebroplasty [7-9,14]. However, two recent randomized multicenter studies showed that the improvements in pain and pain-related disability associated with OVCFs in patients treated with vertebroplasty were similar to the improvements in the control group [15,16]. They found no beneficial effect of vertebroplasty as compared with a sham procedure [15]. In the present survey, we found similar results to those of the two recent studies: the latest VAS and ODI scores were not significantly different between the conservative and vertebroplasty groups. In addition, patients' satisfaction with their clinical outcomes was insignificantly different between the two groups. Thus, this survey failed to find any evidence of superiority for using vertebroplasty compared to conservative treatment for the management of OVCFs in terms of pain, disability and the patient's satisfaction. However, there may be particular situations in which vertebroplasty is more effective than conservative treatment. For example, in very elderly patients suffering from both OVCFs in the thoracic spines and chronic lung diseases, vertebroplasty compared with conservative treatment immediately improved the pulmonary function, which is very critical for such patients [17]. The result of this survey does not unconditionally oppose the use of vertebroplasty; however, it should be reestablished which particular cases with OVCFs are better suited for this procedure.
Overall, 75% (284 of 381) of patients were satisfied with their clinical outcomes. Multiple logistic regression analysis showed that the female gender, patients with lower latest VAS scores or patients with lesser wedge angles had a tendency to be satisfied with their clinical outcomes. A female patient compared with a male patient may have less physical activities, which may induce less back pain. Back muscle fatigue or pain may be more severe in patients with greater wedge angles than those with smaller wedge angles. Because the wedge angle is the only physician-dependent factor, a treating physician should pay close attention to prevent kyphosis, rather than focusing on the loss of vertebral height during fracture management.
Despite relatively favorable value (75% of the patients) of patient's satisfaction on their clinical outcomes, 88% of the patients subjectively felt some or marked deterioration of their general health condition following OVCFs. In addition, the latest VAS (5.3) and ODI (47.7) scores were significantly higher than the the prefracture VAS (3.6) and ODI (26.3) scores. These results indicate that although most patients were satisfied with their clinical outcomes, their subjective general health conditions, as well as their pain and disability, did not recover to the prefracture state. Thus, from the patient's point of view, OVCFs should not be regarded as a minor problem. Furthermore, the results that 87% of patients had not taken any anti-osteoporosis medications prior to fractures and that OVCFs occurred without any traumatic events in 35% of the patients strongly emphasize that more consideration should be paid to preventing OVCFs.
Although most patients with OVCFs were satisfied with their clinical outcome, their subjective general health conditions, as well as their pain and disability, did not recover to the prefracture state. Thus, from the patient's point of view, OVCFs should not be regarded as a minor problem and thus, more consideration must be paid to prevent OVCFs.
Acknowledgments
This study was supported by the Korea Yansen Pharmacy. The authors express thanks to all the patients and the members of the Korean Society of Spine Surgery who took the time to participate in this survey. The results of this survey were presented at the annual meeting of the International Society for the Study of the Lumbar Spine, Geneva, Switzerland, 2008.
References
1. Adachi JD, Ioannidis G, Olszynski WP, et al. The impact of incident vertebral and non-vertebral fractures on health related quality of life in postmenopausal women. BMC Musculoskelet Disord 2002;3:11PMID: 11967146.



2. Adachi JD, Loannidis G, Berger C, et al. The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int 2001;12:903–908. PMID: 11804016.


3. Cockerill W, Ismail AA, Cooper C, et al. European Vertebral Osteoporosis Study (EVOS) Group. Does location of vertebral deformity within the spine influence back pain and disability? Ann Rheum Dis 2000;59:368–371. PMID: 10784519.



4. Cockerill W, Lunt M, Silman AJ, et al. Health-related quality of life and radiographic vertebral fracture. Osteoporos Int 2004;15:113–119. PMID: 14618303.


5. Oleksik A, Lips P, Dawson A, et al. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res 2000;15:1384–1392. PMID: 10893688.


6. Oleksik AM, Ewing S, Shen W, van Schoor NM, Lips P. Impact of incident vertebral fractures on health related quality of life (HRQOL) in postmenopausal women with prevalent vertebral fractures. Osteoporos Int 2005;16:861–870. PMID: 15558238.


7. Alvarez L, Alcaraz M, Perez-Higueras A, et al. Percutaneous vertebroplasty: functional improvement in patients with osteoporotic compression fractures. Spine (Phila Pa 1976) 2006;31:1113–1118. PMID: 16648745.


8. Garfin SR, Buckley RA, Ledlie J. Balloon Kyphoplasty Outcomes Group. Balloon kyphoplasty for symptomatic vertebral body compression fractures results in rapid, significant, and sustained improvements in back pain, function, and quality of life for elderly patients. Spine (Phila Pa 1976) 2006;31:2213–2220. PMID: 16946656.


9. Ha KY, Lee JS, Kim KW, Chon JS. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. J Bone Joint Surg Br 2006;88:629–633. PMID: 16645109.


10. Prather H, Van Dillen L, Metzler JP, Riew KD, Gilula LA. Prospective measurement of function and pain in patients with non-neoplastic compression fractures treated with vertebroplasty. J Bone Joint Surg Am 2006;88:334–341. PMID: 16452745.


11. Rowe SM, Jung ST, Lee JY. Epidemiology of osteoporosis in Korea. Osteoporos Int 1997;7(Suppl 3): S88–S90. PMID: 9536310.


12. Kung AW. Epidemiology and diagnostic approaches to vertebral fractures in Asia. J Bone Miner Metab 2004;22:170–175. PMID: 15108057.


13. Yeom JS, Kim WJ, Choy WS, Lee CK, Chang BS, Kang JW. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg Br 2003;85:83–89. PMID: 12585583.


14. Alvarez L, Perez-Higueras A, Granizo JJ, de Miguel I, Quinones D, Rossi RE. Predictors of outcomes of percutaneous vertebroplasty for osteoporotic vertebral fractures. Spine (Phila Pa 1976) 2005;30:87–92. PMID: 15626987.


15. Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009;361:557–568. PMID: 19657121.


16. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009;361:569–579. PMID: 19657122.



17. Lee JS, Kim KW, Ha KY. The effect of vertebroplasty on pulmonary function in patients with osteoporotic compression fractures of the thoracic spine. J Spinal Disord Tech 2011;24:E11–E15. PMID: 20625321.


Fig. 1
Measurement methods: (A) the percentage of vertebral height loss and (B) the wedge angle. The percentage of vertebral height loss is calculated by the formula: {1-B/[(A+C)/2]}×100%. The wedge angle is defined as the angle A formed between the two lines drawn parallel to the superior and inferior endplates of the fractured vertebra.
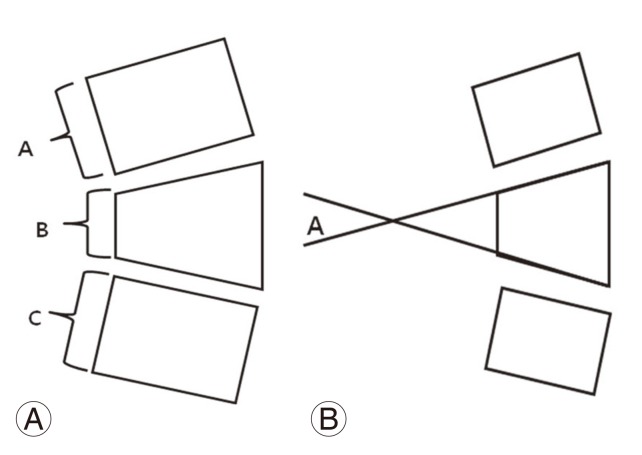
Table 2
Comparisons of the visual analog scale and Oswestry Disability Index scores between the prefracture status and latest status
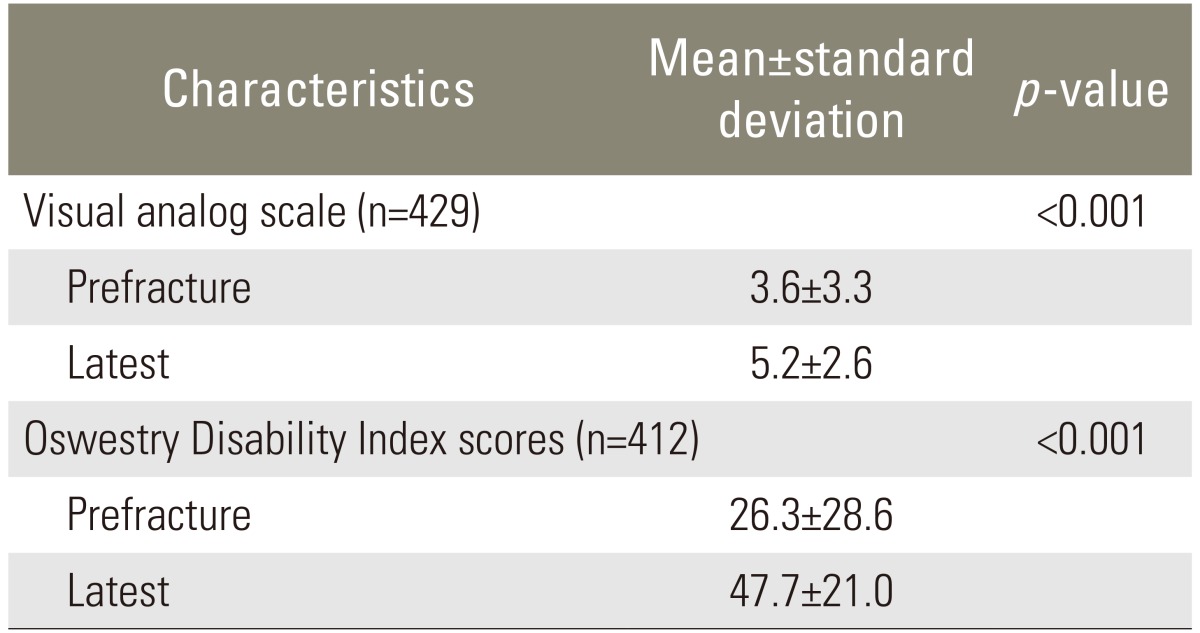
Table 3
Comparisons of the latest VAS scores between the conservative and vertebroplasty groups with regard to the duration from OVCFs

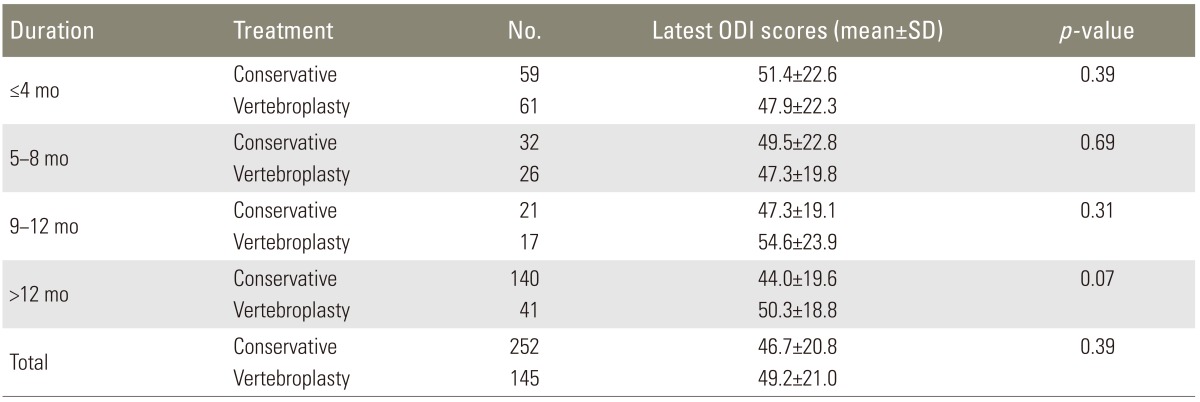
Table 4
Comparisons of the latest ODI scores between the conservative and vertebroplasty groups with regard to the duration from OVCFs