 |
 |
- Search
| Asian Spine J > Volume 16(6); 2022 > Article |
|
Abstract
Conflict of Interest
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Notes
Author Contributions
Each author has significantly contributed to the study. HAP and NSC are involved in study, design, data collection and manuscript preparation. VP contributed in data analysis and manuscript preparation. AWB and AS contributed by expert opinion and in manuscript preparation.
Acknowledgments
Fig. 1

Fig. 2
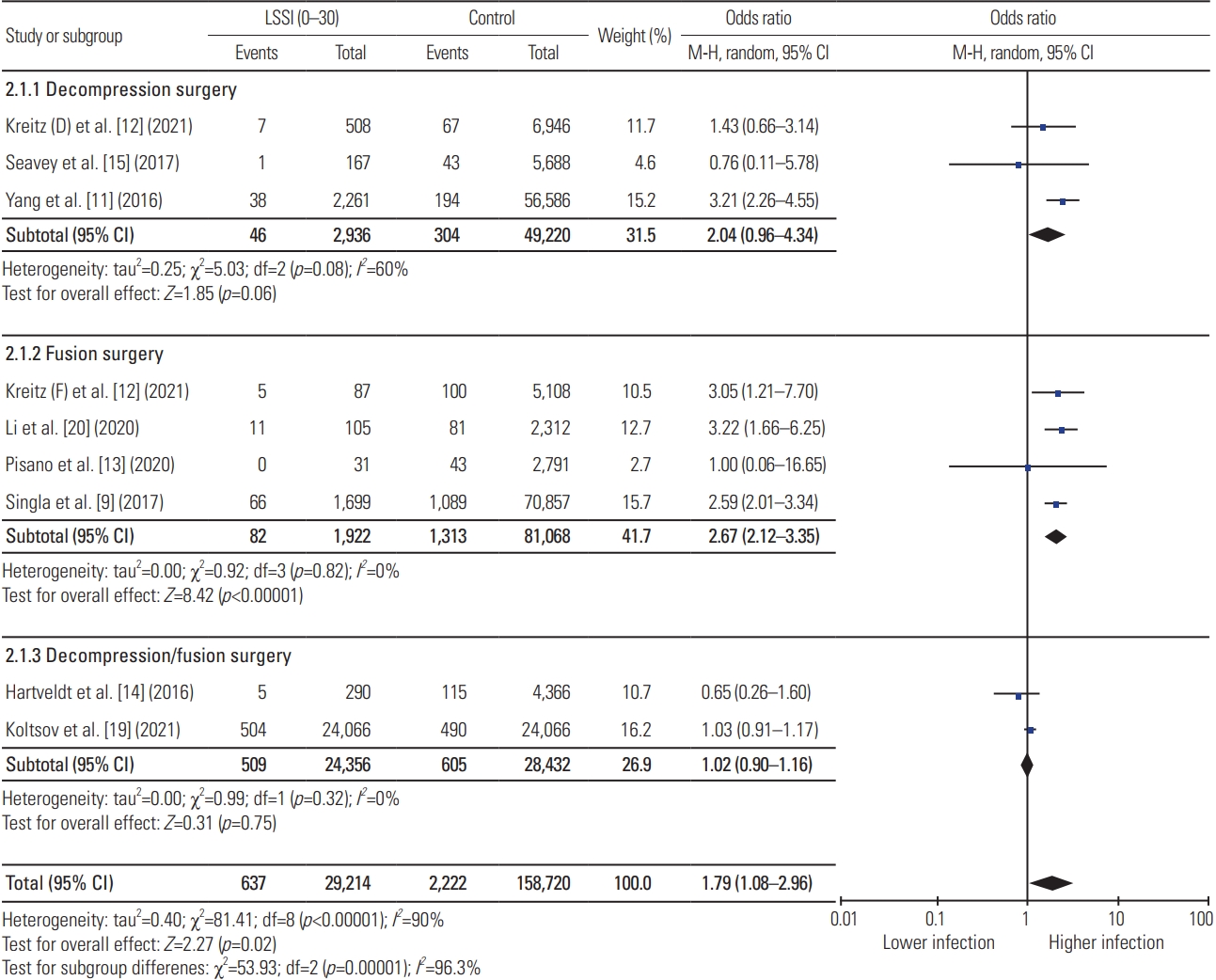
Fig. 3
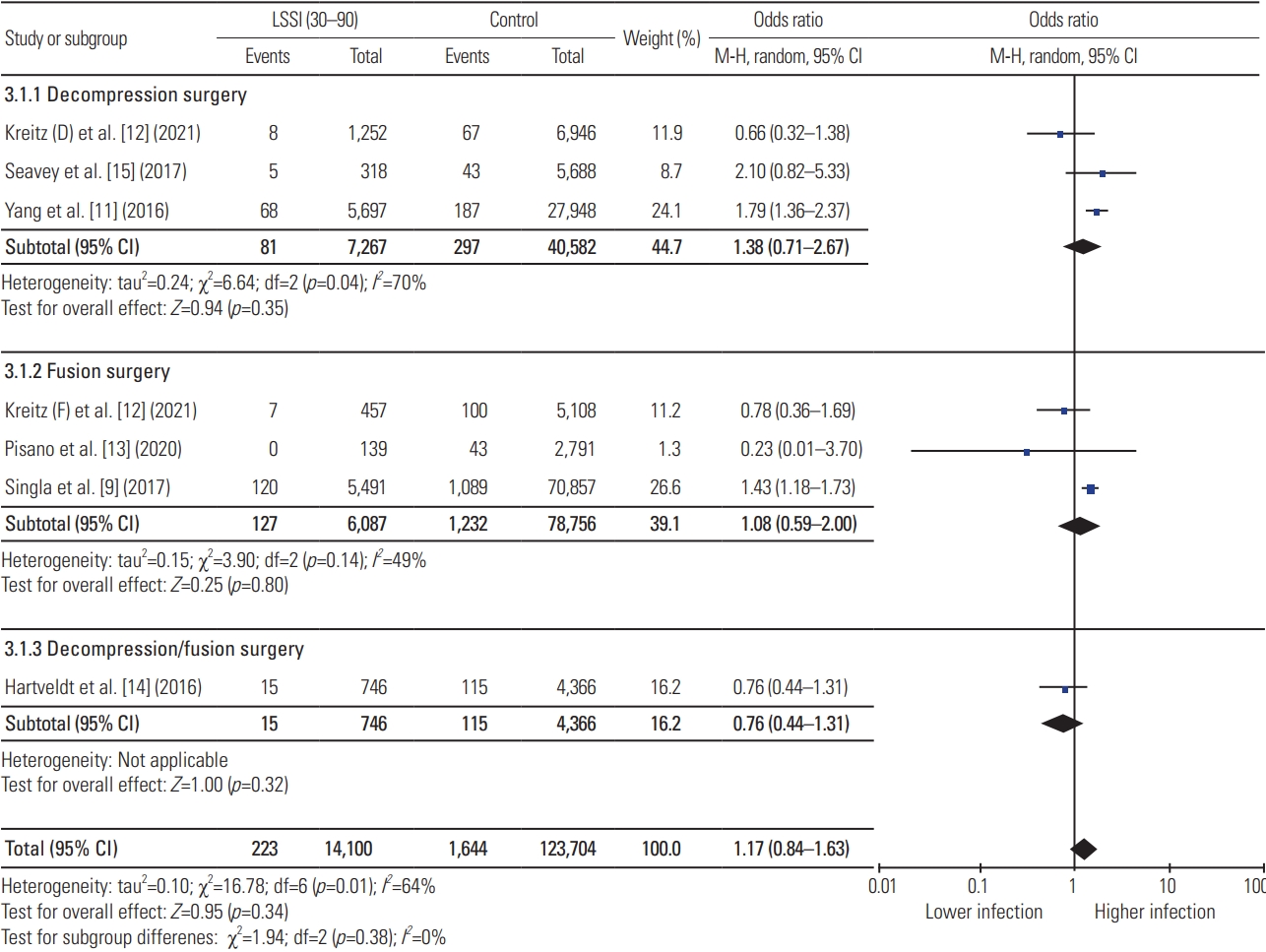
Fig. 4
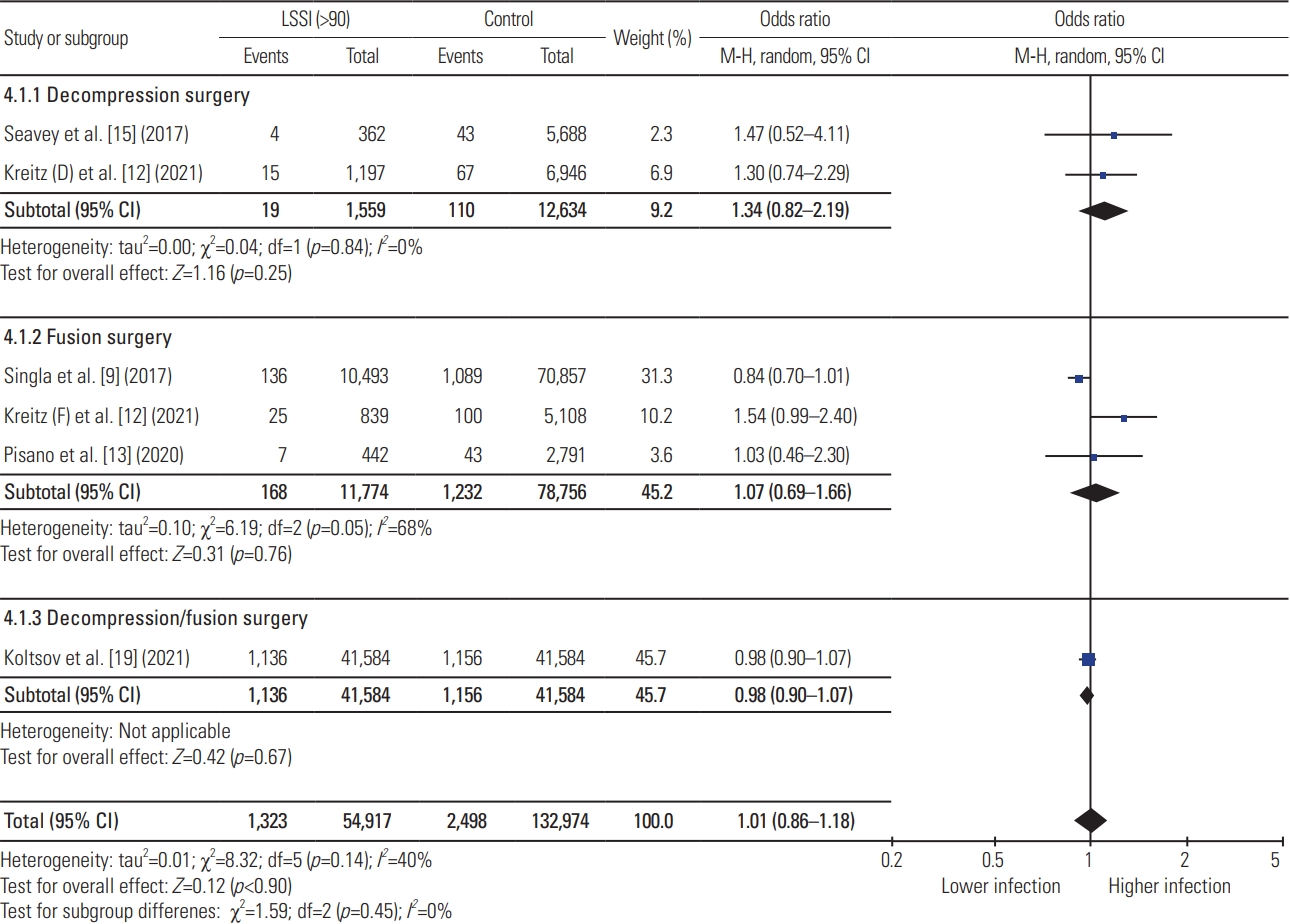
Table 1
| Author | Journal | Study type | Type of surgery | Type of LSSI | Study cohorts | Age (yr) | Definition of infection | Study and control group difference |
|---|---|---|---|---|---|---|---|---|
| Hartveldt et al. [14] (2016) | Spine | Retrospective comparative cohort study: two tertiary care center | Single or multilevel lumbar decompression and fusion surgery | Translaminar or transforaminal LESI | (1) LSSI <30; (2) LSSI 30–90; (3) LSSI <90; (4) control (non-LSSI) | LSSI: 56±16; control: 58±16 | SSI defined as symptoms clinically consistent requiring an I&D intervention performed in the operating room. | Modified CCI is higher in LSSI group compared to control. No difference in tobacco use, obesity, and chronic diabetes. |
| Yang et al. [11] (2016) | The Spine Journal | Retrospective database study (Medicare patients from PearlDriver database) 2005–2012 | Single level lumbar decompression surgery | LESI using CPT code: 64483, 62311 | (1) LSSI <30 vs. control; (2) LSSI 30–90 vs. control; (3) LSSI 90–180 vs. control; (4) LSSI 180–365 vs. control | NR | ICD-9 codes: 998.5, 998.51, 998.59; CPT code: 20005, 22015 | Matched for age, gender, smoking status, obesity, and diabetes. |
| Seavey et al. [15] (2017) | The Spine Journal | Retrospective database study (MHS) 2009–2014 | Single level decompression surgery | LESI using CPT code: 0230T, 64483, 64484 | (1) LSSI <30; (2) LSSI 30–90; (3) LSSI 90–180; (4) LSSI 180–365; (5) LSSI >365; (6) control | LSSI: 38.61±12.56; control: 40.82±14.68 | ICD-9 codes: 998.51, 998.59 | No reporting of medical comorbidities comparison. |
| Singla et al. [9] (2017) | Journal of Neurosurgery Spine | Retrospective database study (Medicare patients from PearlDriver database) 2005–2012 | 1 and 2 level posterior lumbar fusion surgery | LESI using CPT code: 64483, 62311 | (1) LSSI <30; (2) LSSI 30–90; (3) LSSI 90–180; (4) control | NR | ICD-9 codes: 998.5, 998.51, 998.59, 996.67; CPT code: 20005, 22015 | Matched for age, gender, smoking status, obesity, and diabetes. |
| Donnally et al. [8] (2018) | Journal of Spine Surgery | Retrospective database study (Medicare patients from PearlDriver database) 2005–2014 | Primary lumbar decompression surgery | LESI using CPT code: 64483, 62311 | (1) LSSI <30; (2) LSSI 30–90; (3) LSSI 90–180; (4) control | NR | ICD-9 codes: 998.5, 998.51, 998.59, 996.67; CPT code: 20005, 22015 | Strict 1 to 1 matching for age, gender, sex, obesity, diabetes, CCI, and multiple comorbidities. |
| Koltsov et al. [19] (2021) | European Spine Journal | Retrospective database study (IBM Marketscan) 2007–2015 | Lumbar decompression and fusion surgery | LESI using CPT code: 64483, 64484, 62311 | (1) LSSI <30 vs. control; (2) LSSI 30–60 vs. control; (3) LSSI 60–90 vs. control; (4) LSSI 90–365 vs. control | NR | ICD-9 codes | Strict 1 to 1 matching for age, sex, comorbidities, surgery type, and other surgical parameters. |
| Kreitz et al. [12]a) (2021) | Spine | Retrospective comparative cohort study (single institution) 2000–2017 | Separate data analysis for lumbar decompression surgery: Kreitz (D) and lumbar fusion surgery: Kreitz (F) | LESI using CPT code: 64475, 64483, 64493, 62311 | (1) LSSI <30; (2) LSSI 30–90; (3) LSSI >90; (4) control | NR | ICD code: 996.67, 998.12, 998.31, 998.32, 998.59, T81.31XA, T81.32XA, T84.7XXA | No reporting of medical comorbidities comparison. |
| Pisano et al. [13] (2020) | Journal of Clinical Neuroscience | Retrospective database study (MHS) 2009–2014 | Anterior/lateral and posterior lumbar fusion surgery | LESI using CPT code: 0230T, 64483, 64484; lumbar facet steroid injection identified using CPT code: 0216T, 0217T, 64475, 64476, 64493 | (1) LSSI <30; (2) LSSI 30–90; (3) LSSI 90–180; (4) LSSI 180–365; (5) LSSI >365; (6) control | LSSI: 41.14±12.00; control: 43.35±14.49 | ICD-9 codes: 998.51, 998.59 | No reporting of medical comorbidities comparison. |
| Li et al. [20] (2020) | Journal of Pain Research | Prospective comparative cohort study (single institution) | Posterior lumbar fusion surgery | LESI | (1) LSSI <30; (2) LSSI >30; (3) control | LSSI <30: 60.4±5.9; LSSI >30: 60.6±5.8; control: 59.4±6.8 | Infection defined as SSI related to the operation; no clear definition | No difference in age, sex, BMI, diabetes, and smoking status |
LSSI, lumbar spinal steroid injection; LESI, lumbar epidural steroid injection; SSI, surgical site infection; I&D, irrigation and debridement; CCI, Charlson comorbidity index; CPT, current procedural terminology; NR, not reported; ICD, International Classification of Diseases; MHS, military health system; BMI, basal metabolic index.
a) Kreitz et al. [12] has presented separate data analysis for decompression and fusion surgery, which was used separately as Kreitz (D) and Kreitz (F), respectively in this study.
Table 2
| Author | Study group infection rate | Control group infection rate | Final study conclusion |
|---|---|---|---|
| Hartveldt et al. [14] | (1) LSSI <30: 5/290 (1.72%); (2) LSSI 30–90: 15/746 (2.01%); (3) LSSI <90: 19/945 (2.01%) | Control: 115/4,366 (2.63%) | No association—exposure or dose-response relationship—between preoperative LSSI and postoperative infection for lumbar spine surgery. |
| Yang et al. [11] | (1) LSSI <30: 38/2261 (1.7%); (2) LSSI 30–90: 68/5,697 (1.2%); (3) LSSI 90–180: 58/7,017 (0.8%); (4) LSSI 180–365: 32/3,956 (0.81%) | (1) Control <30: 194/36,586 (0.53%); (2) control 30–90: 187/27,948 (0.67%); (3) control 90–180: 148/23,236 (0.64%); (4) control 180–365: 117/18,775 (0.62%) | Preoperative LSSI with in 90 days before surgery found to be associated with significantly higher infection after lumbar decompression than matched control group. |
| Seavey et al. [15] | (1) LSSI <30: 1/167 (0.60%); (2) LSSI 30–90: 5/318 (1.57%); (3) LSSI 90–180: 3/202 (1.49%); (4) LSSI 180–365: 1/89 (1.12%); (5) LSSI >365: 0/71 (0%) | Control: 43/5,688 (0.76%) | Preoperative LSSI do not significantly increase the risk of postoperative infection after single level lumbar decompression with in MHS. |
| Singla et al. [9] | (1) LSSI <30: 66/1,699 (3.9%); (2) LSSI 30–90: 120/5,491 (2.2%); (3) LSSI 90–180: 10,493 (1.3%) | Control: 1,089/70,857 (1.5%) | Lumbar spinal fusion performed within 3 months after LSSI may be associated with an increased rate of postoperative infection. |
| Donnally et al. [8] | (1) LSSI <30: 1.98%; (2) LSSI 30–90: 1.59%; (3) LSSI 90–180: 1.40% | NA (presented odds ratio comparing study group with control group infection rate) | Preoperative LSSI with in 30–180 days may predispose patients to higher infection rates following lumbar decompressions without fusion. |
| Koltsov et al. [19] | (1) LSSI <30: 504/24,066 (2.1%); (2) LSSI 30–60: 622/26,092 (2.4%); (3) LSSI 60–90: 451/18,268 (2.5%); (4) LSSI 90–365: 1,136/41,584 (2.7%) | (1) Control <30: 490/24,066 (2.0%); (2) control 30–60: 601/26,092 (2.3%); (3) control 60–90: 471/18,268 (2.6%); (4) control 90–365: 1,156/41,584 (2.8%) | Preoperative LSSI has no association with increased infection rate after lumbar spine surgery compared to control group. |
| Kreitz (D) et al. [12] | (1) LSSI <30: 7/508 (1.37%); (2) LSSI 30–90: 8/1,252 (0.63%); (3) LSSI >90: 15/1,197 (1.3%) | Control: 67/6,946 (0.96%) | Preoperative LSSI has no association with postoperative infection for lumbar decompression surgery. |
| Kreitz (F) et al. [12] | (1) LSSI <30: 5/87 (5.74%); (2) LSSI 30–90: 7/457 (1.53%); (3) LSSI >90: 25/839 (2.9%) | Control: 100/5,108 (1.95%) | Preoperative LSSI is associated with significantly higher infection rate compared to the control group. |
| Pisano et al. [13] | (1) LSSI <30: 0/31 (0%); (2) LSSI 30–90: 0/139 (0%); (3) LSSI 90–180: 2/158 (1.27%); (4) LSSI 180–365: 3/162 (1.85%); (5) LSSI >365: 2/122 (1.64%) | Control: 43/2,791 (1.54%) | Postoperative infection rate is not significantly increased in patients receiving LSSI prior to lumbar arthrodesis. |
| Li et al. [20] | (1) LSSI <30: 11/105 (10.48%); (2) LSSI >30: 8/140 (5.71%) | Control: 81/2,312 (3.51%) | Preoperative LSSI within 30 days is associated with significantly higher infection rate after lumbar fusion surgery. |
Table 3
| Criteria | Hartveldt et al. [14] | Yang et al. [11] | Seavey et al. [15] | Singla et al. [9] | Donnally et al. [8] | Koltsov et al. [19] | Kreitz et al. [12] | Pisano et al. [13] | Li et al. [20] |
|---|---|---|---|---|---|---|---|---|---|
| A clearly stated aim | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Inclusion of consecutive patients | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Prospective collection of data | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Endpoints appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Unbiased assessment of the study endpoint | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Follow-up period appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Loss to follow up less than 5% | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Prospective calculation of the study size | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| An adequate control group | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Contemporary groups | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Baseline equivalence of groups | 1 | 2 | 0 | 2 | 2 | 0 | 0 | 0 | 2 |
| Adequate statistical analyses | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 |
| Total | 16 | 18 | 16 | 18 | 18 | 15 | 16 | 16 | 20 |
References
- TOOLS
-
METRICS

- Related articles in ASJ
-
Endoscopic Anterior Lumbar Interbody Fusion: Systematic Review and Meta-Analysis2023 December;17(6)





