Preoperative and Postoperative Pulmonary Function in Elderly Patients with Thoracolumbar Kyphoscoliosis
- Tatsuya Yasuda, Tomohiko Hasegawa, Yu Yamato, Sho Kobayashi, Daisuke Togawa, Yukihiro Matsuyama
- Received February 16, 2015 Revised March 10, 2015 Accepted March 22, 2015
- ABSTRACT
-
- Study Design
- Case series.
- Purpose
- The objective of this study was to investigate the change in pulmonary function in adult patients with a spinal deformity who underwent spinal corrective surgery.
- Overview of Literature
- Degenerative lumbar and/or thoraco-lumbar deformities are is often prominent in adult spinal deformity cases, whereas a thoracic deformity involving the chest wall is inconspicuous. A lumbar spine deformity could affect the pulmonary function; however, few reports have investigated pulmonary function in adult patients with a spinal deformity.
- Methods
- This study included 14 adult patients with a spinal deformity who underwent posterior corrective fusion (3 males, 11 females; mean age, 67.4 years). We measured percent vital capacity (%VC) and percent forced expiratory volume in 1 second (%FEV1) before surgery and six months after surgery. We investigated the change in pulmonary function after corrective surgery and the correlation between radiographic parameters and pulmonary function.
- Results
- Mean preoperative %VC and %FEV1 values were 99.9% and 79.3%, respectively. Two cases were diagnosed with restrictive impairment, and two cases were diagnosed with obstructive impairment before surgery. %VC improved in the restrictive impairment cases six months after surgery. However, %FEV1 did not improve significantly after surgery in the obstructive impairment cases.
- Conclusions
- Restrictive impairment was improved in adult patients with a spinal deformity by corrective spinal surgery. However, spinal surgery did not improve obstructive impairment.
- Introduction
- Introduction
Curvature of the chest cage is almost a three-dimensional distortion in adolescent cases of idiopathic scoliosis. Therefore, patients with progressive scoliosis have an increased risk for developing respiratory failure [1,2,3].Spinal deformities are becoming increasingly prevalent in the elderly population, and decrease quality of life. In particular, sagittal imbalance is strongly correlated with health related quality score [4,5,6,7].The main deformities in these cases are lumbar or thoraco-lumbar, whereas a chest wall deformity is rare. A deformity of the lumbar spine may affect pulmonary function; however, few reports are available about pulmonary function in adult patients with a spinal deformity.The purpose of this study was to investigate the change in pulmonary function in adult patients with a spinal deformity who underwent spinal corrective surgery.
- Materials and Methods
- Materials and Methods
- 1. Patients
- 1. Patients
This study included 14 adult patients with a spinal deformity (3 males, 11 females; mean age, 67.4 years; range, 45-78 years) who underwent posterior corrective fusion. Based on the scoliosis apex, the number of patients at each level were: two at L1, seven at L2, four at L3, and one at L4.- 2. Surgical procedure
- 2. Surgical procedure
All cases underwent a Ponte osteotomy with a rod rotation maneuver, laminectomy, and posterior interbody fusion using a cage with a L2/3 to L5/S1 autograft to correct kyphoscoliosis. The upper fusion level was lower thoracic (T8-T10), and the lower fusion level was L5 or S1.- 3. Radiography
- 3. Radiography
A radiographic evaluation was performed according to an established positioning protocol for anteroposterior and lateral 36-inch standing radiographs. Radiographic parameters, including coronal Cobb angle, sagittal vertical axis (SVA), T5-T12 thoracic kyphosis (TK) and T12-S1 lumbar lordosis (LL) were analyzed before surgery, just after surgery, and six months after surgery.- 4. Pulmonary function
- 4. Pulmonary function
Pulmonary function tests were carried out in all patients before surgery and six months after the surgery. We measured percent vital capacity (%VC) and percent forced expiratory volume in 1 second (%FEV1). These two paramparameters are required to diagnose obstructive and restrictive impairment. Obstructive impairment was diagnosed, if %FEV1 was <70%, and restrictive impairment was diagnosed if %VC was <80%. Merged cases were diagnosed as mixed impairment.We investigated the change in pulmonary function before and after spinal corrective surgery. Furthermore, we analyzed the correlation between the radiographic parameters and pulmonary function parameters using Pearson correlation coefficient analysis and the Wilcoxon signed rank test.
- Results
- Results
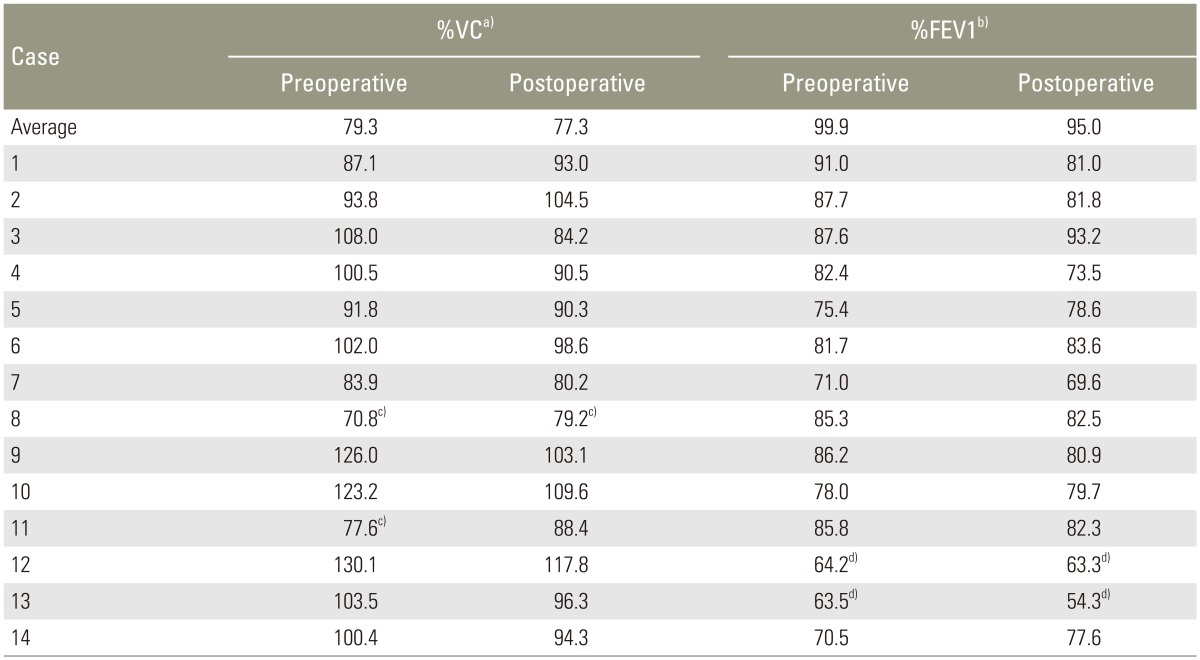
- 1. Radiography
- 1. Radiography
The coronal Cobb angle improved from 45.5° to 13.4° just after surgery (correction rate, 70.5%) and was 12.5° six months after surgery. SVA improved from 73.9 mm just after surgery to 77.2 mm six months after surgery. TK and LL changed from 29.6° and 10.9° to 34.4° and 31.2° just after surgery, respectively, and were 32.1° and 31.0° six months after surgery (Table 1).- 2. Pulmonary function
- 2. Pulmonary function
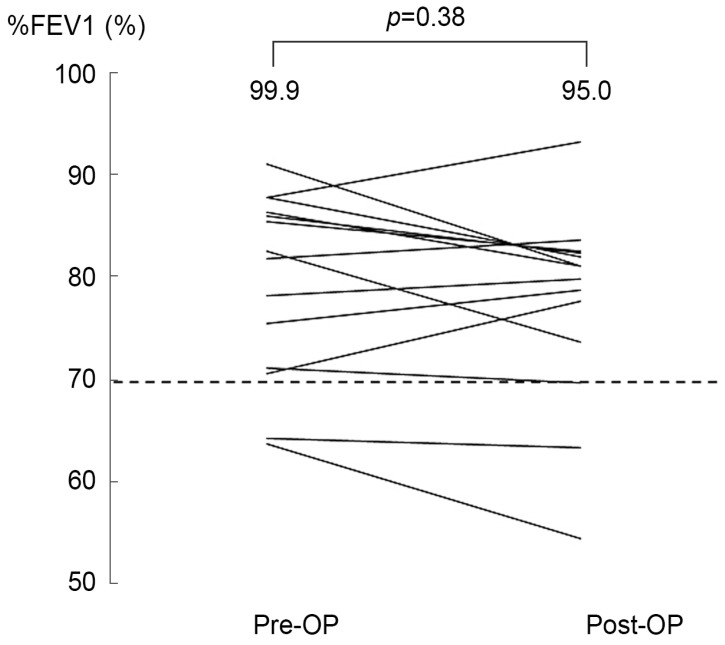
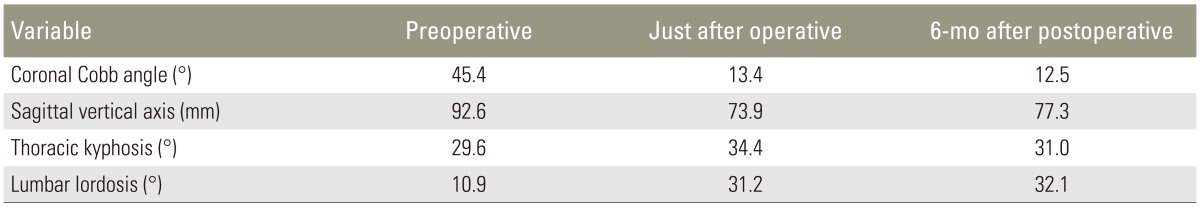
Mean %VC and %FEV1 values were 99.9% and 79.3% preoperatively and 95.0% and 77.3% six months after surgery. %VC and %FEV1 did not change significantly six months after surgery (%VC, p=0.49; %FEV1, p=0.38). Two cases were preoperatively diagnosed with restrictive impairment. In both cases, %VC improved from 70.8% and 77.6% to 79.2% and 88.4%, respectively six months after surgery. Two cases were preoperatively diagnosed with obstructive impairment. %FEV1 did not improve in either case (64.2% and 63.5% to 63.3% and 54.3%, respectively) six months after surgery (Table 2, Figs. 1, 2, 3).
- Discussion
- Discussion
A scoliosis deformity decreases pulmonary function due to stiffness of the chest wall and a decrease in respiratory muscle force. New pulmonary alveoli are added until 5-8 years of age [8] and development continues until 20 years of age [9]. Therefore, improved pulmonary function in adolescent patients with idiopathic scoliosis is expected after surgically correcting the chest cage deformity [10,11,12,13].The main deformity occurs in the lumbar or thoracolumbar area in adults with a spinal deformity. In this series, the scoliosis apex level was L1-L4 in all cases and most cases, maintained pulmonary function (%VC and %FEV1), suggesting that the lumbar and thoraco-lumbar curve affects pulmonary function.%VC improved postoperatively in the two cases of restrictive impairment. Decreased mobility of the diaphragm and chest wall may have been improved by correcting the lumbar spine deformity. Restrictive impairment can be improved by corrective surgery in adult patients with a spinal deformity. Therefore, we should consider corrective surgery to improve restrictive impairment if adult patients with a spinal deformity have decreased %VC.%FEV1 did not improve postoperatively in two cases of obstructive impairment. Obstructive impairment can occur in elderly patients due to problems with the respiratory tract. The prevalence of chronic obstructive pulmonary disease (COPD) is 10.9% in Japan [14]. If adult patients with a spinal deformity have obstructive impairment it is necessary to check for lung diseases, such as COPD.Some limitations of this study should be mentioned. The first limitation is that the sample size was small; thus, further studies should have an increased number of cases. The second limitation is the timing of the pulmonary function evaluation, as more time may be need for pulmonary function to improve. Therefore, further long-term evaluations should be conducted. Furthermore, elderly patients may have subclinical respiratory disease, which is difficult to distinguish.
- Conclusions
- Conclusions
Our results suggest that restrictive impairment can be improved by corrective spinal surgery in adult patients with a spinal deformity. However, obstructively impaired adult patients with a spinal deformity should be checked for lung disease such as COPD.
- Conflict of Interest
- Conflict of Interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- REFERENCES
- REFERENCES
- 1. Giordano A, Fuso L, Galli M, et al. Evaluation of pulmonary ventilation and diaphragmatic movement in idiopathic scoliosis using radioaerosol ventilation scintigraphy. Nucl Med Commun 1997;18:105–111. PMID: 9076764.
[Article] [PubMed]2. Leong JC, Lu WW, Luk KD, Karlberg EM. Kinematics of the chest cage and spine during breathing in healthy individuals and in patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24:1310–1315. PMID: 10404572.
[Article] [PubMed]3. Leaver JM, Alvik A, Warren MD. Prescriptive screening for adolescent idiopathic scoliosis: a review of the evidence. Int J Epidemiol 1982;11:101–111. PMID: 7047422.
[Article] [PubMed]4. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682–688. PMID: 15770185.
[Article] [PubMed]5. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024–2029. PMID: 16166889.
[Article] [PubMed]6. Lafage V, Schwab F, Skalli W, et al. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine (Phila Pa 1976) 2008;33:1572–1578. PMID: 18552673.
[Article] [PubMed]7. Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine (Phila Pa 1976) 2010;35:E1193–E1198. PMID: 20959772.
[Article] [PubMed]8. Thurlbeck WM. Postnatal human lung growth. Thorax 1982;37:564–571. PMID: 7179184.
[Article] [PubMed] [PMC]9. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med 1999;159:179–187. PMID: 9872837.
[Article] [PubMed]10. Gagnon S, Jodoin A, Martin R. Pulmonary function test study and after spinal fusion in young idiopathic scoliosis. Spine (Phila Pa 1976) 1989;14:486–490. PMID: 2727795.
[Article] [PubMed]11. Kumano K, Tsuyama N. Pulmonary function before and after surgical correction of scoliosis. J Bone Joint Surg Am 1982;64:242–248. PMID: 7056779.
[Article] [PubMed]12. Pehrsson K, Danielsson A, Nachemson A. Pulmonary function in adolescent idiopathic scoliosis: a 25 year follow up after surgery or start of brace treatment. Thorax 2001;56:388–393. PMID: 11312408.
[Article] [PubMed] [PMC]
Fig. 1
Scatter plot of the pulmonary function test results. Two cases of restrictive impairment and two cases of obstructive impairment were identified. %VC, percent vital capacity; %FEV1, percent forced expiratory volume in 1 second.
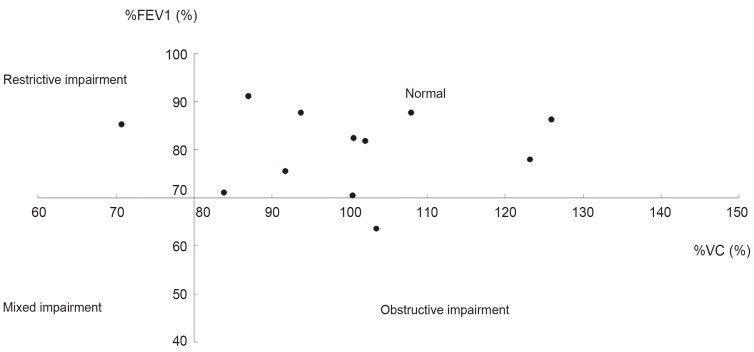
Fig. 2
Postoperative changes in percent forced expiratory volume in 1 second (%FEV1). The two obstructively impaired cases had not improved 6 months after surgery. Dotted line means normal reference value. Pre-OP, preoperative; Post-OP, postoperative.