APSS-ASJ Best Clinical Research Award: Predictability of Curve Progression in Adolescent Idiopathic Scoliosis Using the Distal Radius and Ulna Classification
Article information
Abstract
Study Design
Prospective study.
Purpose
To determine the risk of clinically significant curve progression in adolescent idiopathic scoliosis (AIS) based on the initial Cobb angle and to test the utility of the distal radius and ulna (DRU) classification in predicting these outcomes.
Overview of Literature
Determining the remaining growth potential in AIS patients is necessary for predicting prognosis and initiating treatment. Limiting the maturity Cobb angle to <40° and <50° reduces the risk of adulthood progression and need for surgery, respectively. The risk of curve progression is the greatest with skeletally immature patients and thus warrants close monitoring or early intervention. Many parameters exist for measuring the skeletal maturity status in AIS patients, but the DRU classification has been shown to be superior in predicting peak growth and growth cessation. However, its predictive capabilities for curve progression are unknown.
Methods
Totally, 513 AIS patients who presented with Risser 0–3 were followed until either skeletal maturity or the need for surgery, with a minimum 2-year follow-up period. Outcomes of 40° and 50° were used for probability analysis based on the cut-offs of adulthood progression risk and surgical threshold, respectively.
Results
At the R6/U5 grade, most curves (probability of ≥48.1%–55.5%) beyond a Cobb angle of 25° progressed to the 40° threshold. For curves of ≥35°, there was a high risk of unfavorable outcomes, regardless of skeletal maturity. Most patients with the R9 grade did not progress, regardless of the initial curve magnitude (probability of 0% to reach the 50° threshold for an initial Cobb angle of ≥35°).
Conclusions
This large-scale study illustrates the utility of the DRU classification for predicting curve progression and how it may effectively guide the timing of surgery. Bracing may be indicated for skeletally immature patients at an initial Cobb angle of 25°, and those with a scoliosis ≥35° are at an increased risk of an unfavorable outcome, despite being near skeletal maturity.
Introduction
Determining a child's remaining skeletal growth is crucial for the management of adolescent idiopathic scoliosis (AIS) [123]. This is particularly important for brace treatment because the prompt initiation of this management approach can reduce the number of AIS patients undergoing surgery [456]. Generally, the goal of a bracing treatment is to prevent a patient from reaching the commonly described surgical threshold of >50°. However, the prevention of virtually any Cobb angle progression by bracing is also beneficial. According to natural history studies, a smaller Cobb angle at skeletal maturity is more cosmetically acceptable and preventing the 40° threshold can reduce the risk of adulthood deterioration and need for surgery [37]. Adulthood progression as reported in these studies can be at least 1° per year for curvatures of ≥40° at skeletal maturity.
Good brace compliance with more than 20 hours of daily use has been shown to be effective in reducing curve progression [8]. In a multicenter study, Weinstein et al. [6] demonstrated that in patients with high-risk curves, bracing significantly decreased curve progression based on a dose-effect response and, in turn, the need for surgery. Identification of peak height velocity (PHV) is thus essential for good outcomes as it indicates the period where the risk of deformity progression is the greatest. It is equally important to identify patients who have passed their growth spurt as brace effectiveness is limited in these cases and complications may arise from prolonged use [8910]. Extensive and indiscriminate use of bracing in children has been shown to reduce spinal mobility, lead to poor body image and loss of self-esteem, and reduce the quality of life [111213]. Maintaining good health and quality of life parameters is crucial to the success of AIS treatment [141516]
It is the clinician's responsibility to gauge the risk of reaching the previously discussed thresholds and the potential benefits of prescribing brace treatment. Having an accurate skeletal maturity assessment tool is thus necessary to predict a patient's remaining growth potential to facilitate this decision-making process. To this end, prediction models can be very useful as they generate an algorithm based on large datasets [17]. However, a standardized parameter must be used for accurate testing. The distal radius and ulna (DRU) classification incorporates the whole range of growth phases with 11 radius grades (R1–R11) and 9 ulna grades (U1–U9). This classification has been shown to be easily reproducible, with excellent intra- and inter-rater reliability, and a simplified version has been developed for clinical use [1819]. Due to being solely based on the morphology of two physeal plates, it is more user-friendly than measuring the entire hand. Large-scale thorough analyses of the relationship between the DRU classification and the Risser sign, age at menarche, and metacarpal/phalangeal physeal capping and fusion have been performed [1220], and it has been shown that the DRU classification is superior to conventional methods in determining peak growth (Fig. 1) and growth cessation (Fig. 2). Nevertheless, its utility in predicting curve progression and curve magnitude at skeletal maturity has not yet been determined. Therefore, this study aimed to investigate the capacity of the DRU classification, using the presenting Cobb angle, to predict whether the clinically relevant 40° and 50° outcome thresholds would be reached at skeletal maturity.

Wrist radiograph showing a distal radius and ulna classification grade of R6 and U5, which indicates peak height velocity.
Materials and Methods
1. Clinical data
This study was based on prospectively collected data from a tertiary scoliosis specialty clinic. From April 1998 to June 2014, all AIS patients who initially presented with Risser 0–3 and were less than 2 years post menarche were followed until skeletal maturity at Risser 5 or until surgical intervention was needed, which was offered for those with Cobb angles of >50°. All non-idiopathic scoliosis patients and AIS patients who first presented with a Cobb angle of ≥40° were excluded. This study was approved by a local ethics review board.
At initial presentation, age, body height (BH), arm span (AS), coronal Cobb angle magnitude, Lenke classification, Risser sign, and DRU classification grades were recorded. Age at menarche was listed for females. All patient data were recorded as per the standard protocol in our clinic. BH was measured with a patient standing on a stadiometer without shoes and socks. The heels were kept together, and the recorder measured only BH after the patient was asked to stand upright with the chin up. AS was measured with the patient's arms apart in the maximally outstretched position from the ends of the middle fingers. All Cobb angles were measured for all curves on a standing posteroanterior whole spine plain radiograph. The same radiograph was used for grading the Risser sign. The DRU classification was measured using left wrist radiographs routinely obtained for skeletal maturity grading [19]. Radiographs were generally obtained every 6 months, particularly during the peak growth spurt periods. It was also recorded whether bracing was prescribed for patients. Our protocol for bracing follows that of the SRS criteria, which includes patients aged 10 or older, with Risser 0–2, with a primary curve angle of 25°–40°, and who were premenarchal or <1 year post menarche (females). However, due to the lack of objective compliance monitoring data and possible inaccuracies with self-reported compliance, this parameter was not used in the study.
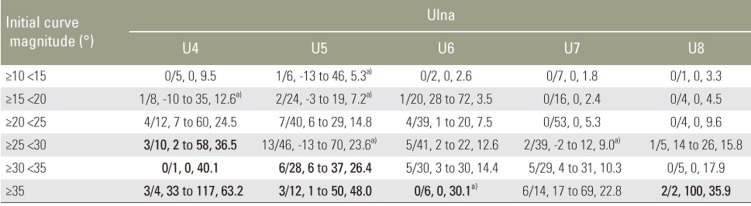
The risk of curve progression was tested based on each patient's initial curve magnitude and DRU classification grade. The initial curve magnitudes were grouped as ≥10° to <15°, ≥15° to <20°, ≥20° to <25°, ≥25° to <30°, ≥30° to <35°, and ≥35°. The major curve Cobb angle was used for progression analysis in this study. The final Cobb angle at either skeletal maturity or at surgical intervention was used as the outcome measure. Curve progression was identified as any curve progression beyond 5° of the initial curve magnitude. Curve progression to two “poor” outcomes was used for analysis. This included the 40° threshold for increased risk of adulthood deterioration and the 50° threshold for the need for surgery.
2. Statistical analysis
Descriptive data are presented as mean±standard deviation, and statistical analyses were performed using one-way analysis of variance to explore intergroup differences. For bracing patents, the chi-square test was utilized to determine the relationship between various parameters (i.e., bracing) and curve progression. Following univariate analyses, covariates were chosen for regression modelling if they had a p-value of <0.200. Multivariate stepwise logistic regression was used to determine the probabilities of curve progression to the outcomes of 40° and 50° thresholds. Two sets of analyses were undertaken by dichotomizing the presence or absence of progression to one of the thresholds based on the initial Cobb angle and DRU classification grade. The predicted percentage change generated from the regression model was used to represent the risk of progression. The forecasted probability was divided into quartiles: <25%, 25% to <50%, 50% to <75%, and ≥75%; a probability of 25% to <50% was considered moderate, while that of ≥50% was considered high risk. All p-values of <0.05 were regarded as statistically significant, and 95% confidence intervals were reported.
Results
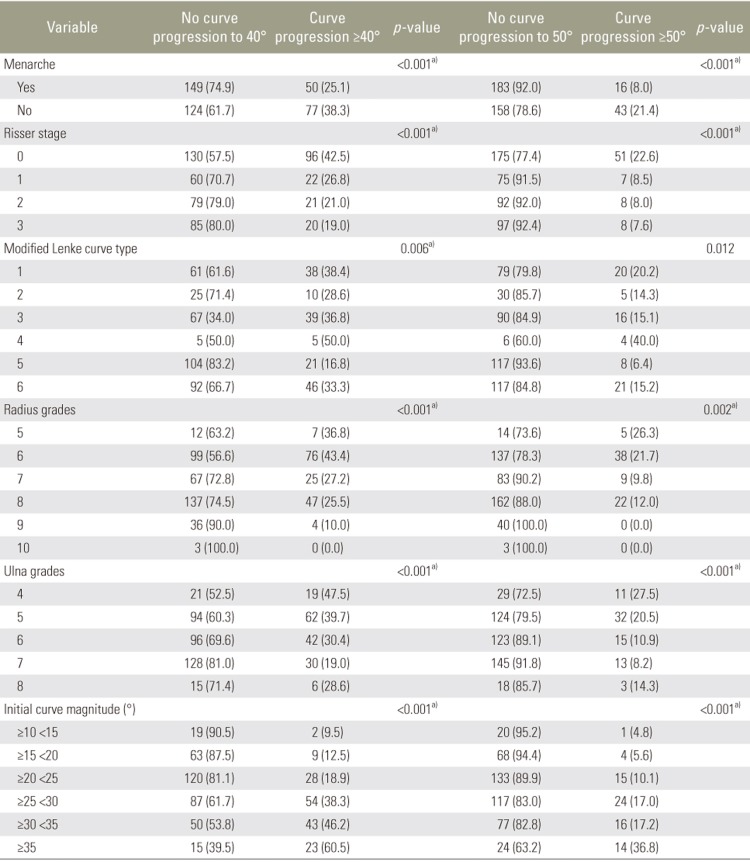
Totally, 513 AIS patients (n=400 females) were studied. The mean age at initial presentation was 12.5±1.3 years, and the mean follow-up duration was 4.7±2.5 years until skeletal maturity or when surgery was needed. At initial presentation, 50.2% of the patients were premenarchal. Those who were postmenarchal presented an average of 8.1±6.1 months after menarche. Baseline data are presented in Table 1. The spread of data was similar between females and males, and the two groups were combined for the general representation of the study population. Up to 316 patients (61.6%) received bracing, and 32 of them eventually required surgery, despite bracing. A total of 226 patients (44.1%) were at Risser 0, while 175 (34.1%) were graded as R6 and 156 (30.4%) as U5 at initial presentation. According to published data [12], an R6U5 grade indicates the peak growth period. Regarding curve types, patients with major thoracolumbar or lumbar curves had lesser risk of progression than those with major thoracic and double thoracic curves. Those with Lenke 5 curves rarely (6.4%) progressed to the surgical threshold.
Specifically regarding the 226 patients with Risser 0 at baseline, 182 (80.5%) received bracing treatment, and of these, 20 (11.0%) subsequently underwent surgery. The outcomes from bracing are listed in Table 2. Up to 56.3% of the patients with an initial Cobb angle of ≥35° reached both 40° and 50° thresholds, despite most of them being braced. Differences in the spread of parameters were observed between those who did not have curve progression at all or did not reach clinically significant outcome thresholds and those who reached the 40° or 50° threshold; these data are presented in Table 3. Of all patients at Risser 0, only 58 (25.7%) did not experience curve progression; of them, 38 (65.5%) were braced. A classification of Risser 0 was a significant predictor of later reaching the surgical threshold, but a classification of up to Risser 3 can still have significant risk for adulthood progression. A statistically significant prediction model could not be constructed for the Risser sign. Although 168 patients (74.3%) had significant curve progression, 72 (42.9%) did not progress beyond the 40° threshold, regardless of the initial Cobb angle. A total of 96 patients (57.1%) reached the 40° threshold and 51 (30.4%) reached the 50° threshold.
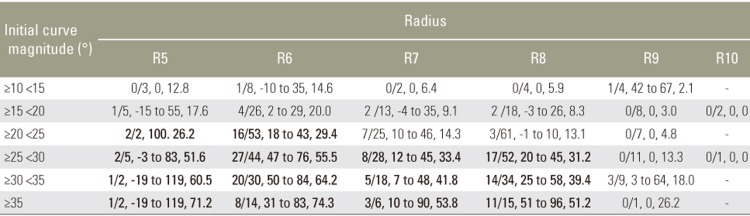
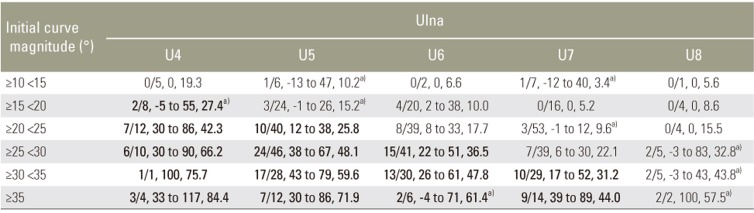
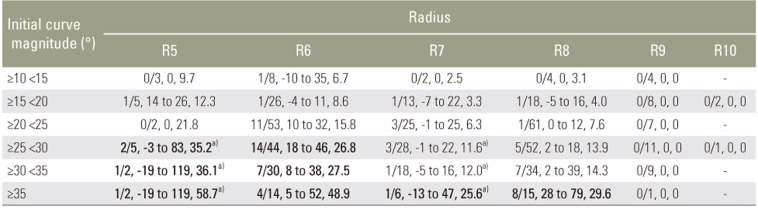
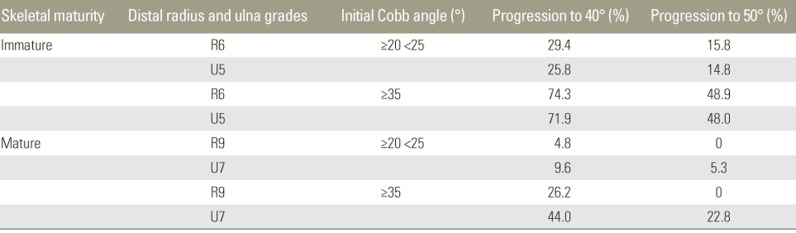
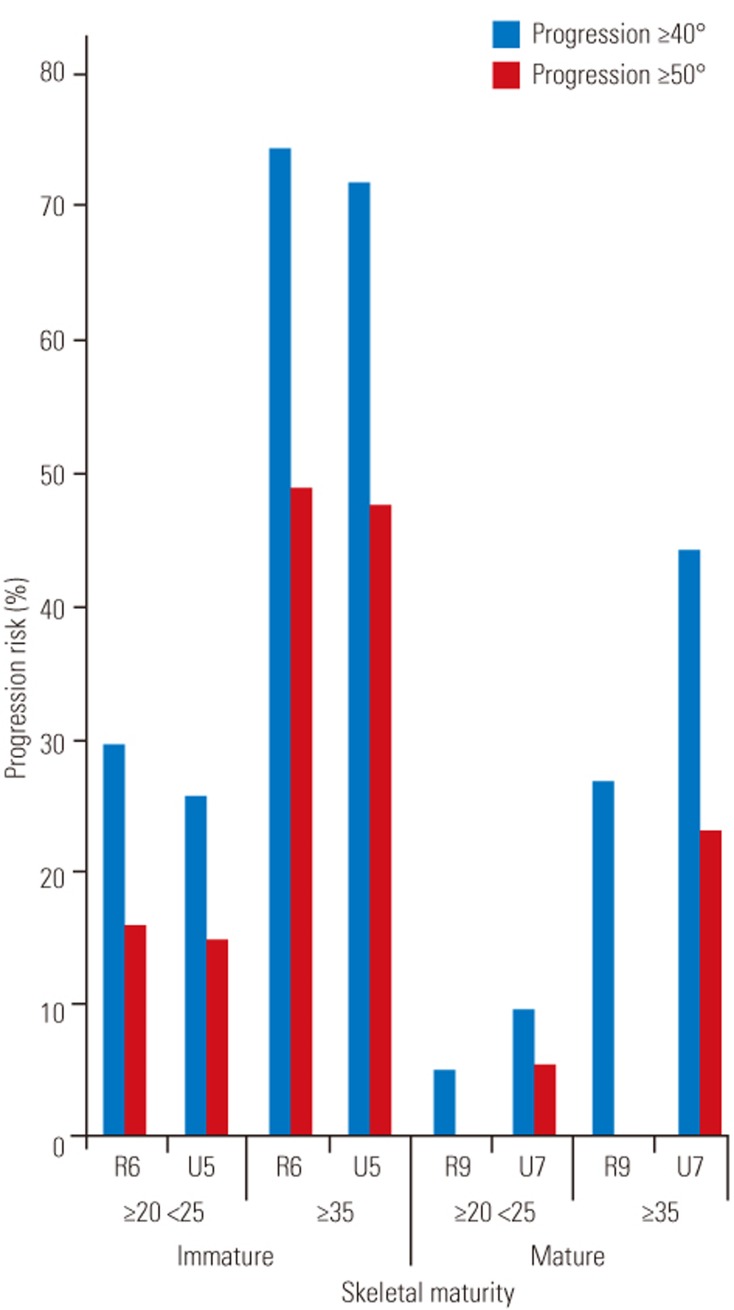
In general, those who presented with larger Cobb angles were more likely to reach the 40° or 50° threshold (Fig. 3). At the final outcome point, 162 (31.6%) reached the 40° threshold and 74 (14.4%) reached the 50° threshold. The Cobb angle for 148 of our patient (28.8%) was ≥20° to <25° at initial presentation. The regression model for curve progression to the 40° threshold is presented in Tables 4, 5. The overall correct predictions for the radius and ulna classification grades were 74.5% and 71.5%, respectively. Similarly, the regression model (Tables 6, 7) for curve progression to the 50° threshold had high overall prediction accuracies of 85.6% and 86.0% for the radius and ulna classification grades, respectively. At R6 and U5, most curves with a Cobb angle of >25° progressed, while at R8 and U7, only those with a Cobb angle of ≥35° were at risk of unfavorable outcomes. At R9 and U8, most curves did not progress. A simple summary of the relationship between the initial Cobb angle and the DRU classification grade is illustrated in Table 8 and Fig. 4.
Discussion
The present study illustrates the utility of the DRU classification grade to predict curve magnitude outcomes at skeletal maturity. Based on a large sample of AIS patients, the DRU classification grades together with the corresponding initial Cobb angles were effectively predictive of the outcomes at skeletal maturity. Using both radius and ulna grades for prediction may provide the best forecast for future curve progression. The present study also utilized clinically relevant curve progression outcomes for Cobb angles of 40° or 50°. According to natural history studies, reaching either of these two values can be considered as poor outcomes due to the risks of adulthood deterioration and need for surgery [37].
The accurate prediction of which AIS patients will experience curve progression is dependent on the clinician's ability to interpret the remaining growth potential. At initial presentation, the severity of the deformity measured by the Cobb angle and growth rate can provide useful information regarding the likely future curve behavior [521]. Many radiographic parameters exist to predict growth but have known limitations, including poor prediction of PHV for the timing of brace treatment [2223242526], concerns with inter-observer reliability and complexity [272829], and the cumbersome nature of using them in a busy clinical setting [30]. In contrast, the DRU classification has been shown to be reproducible and have excellent intra- and inter-rater reliability and the capability to be simplified for clinical use [1819]. The DRU classification was found to be superior to the Risser sign, with its larger spread of grades prior to PHV so that both the acceleration and deceleration phases of growth can be determined during puberty [1]. The DRU classification has also been used to identify mismatches between growth and curve progression rates, which are not reported in other maturity parameters such as TW, Sanders stage, or Risser sign [20]. Hence, it is useful for determining the timing of both brace initiation and weaning. It has also been shown in this study that the DRU classification is superior to the Risser sign in terms of prediction, as patients with Risser 0 had near equal risk of adulthood progression and surgical threshold and those with Risser 3 still had a significant risk. This may be related to the unreliable Risser sign and mismatches observed with growth [1].
The risk of curve progression at PHV is of particular concern as prompt brace treatment at this point has been shown to reduce the number of AIS patients undergoing surgery [456]. From the analysis of those at PHV with R6/U5 [1], patients with a large Cobb angle of ≥35° at initial presentation are expected to reach both 40° and 50° thresholds with high probability (around 50%–70%). This suggests that the prognosis of patients who present with this curve magnitude at skeletal immaturity is poor. These patients should be provided brace treatment as soon as possible but are nevertheless likely to require surgical correction in the future. Even at R8/U7, which is near the expected growth cessation stage (R9/U7) [1], having such an initial curve magnitude will result in high (44.0%–51.2%) and moderate (22.8%–29.6%) predicted probabilities of reaching the 40° and 50° thresholds, respectively. This suggests that bracing intervention is still indicated even at near skeletal maturity for large curves to prevent these poor outcomes. A more aggressive bracing protocol should be considered in these patients.
It is fortunate that only a small number of patients in the general population (7.4%) present with a curve magnitude of ≥35° because of our long-standing school screening program. Most patients in our study presented with an initial Cobb angle of ≥20° to <25° (28.8%) or ≥25° to 30° (27.5%). Based on our results, the 25° threshold is the main cut-off for the likelihood of poor outcomes in our scoliosis patients at PHV (R6/U5) by reaching the 40° threshold. This is evidenced by only a 25.8%–29.4% probability in the ≥20° to <25° group with an increase to 48.1%–55.5% probability in the ≥25° to <30° group. However, patients are less likely to reach the surgical threshold, with only 14.8%–15.8% probability if they are in the ≥20° to <25° group and a 23.6%–26.8% probability in the ≥25° to <30° group. Hence, initial presenters at approximately 25° and at PHV should be monitored closely for any deterioration. Bracing for this group should be considered only for those who experience curve progression during follow-up as the probability of reaching the surgical threshold is not high. No significant probability of poor outcomes was observed for either group in patients who present at a more mature stage of R9.
It is important to note that 61.6% of the patients in the present series were referred for bracing. As seen in Table 2, many of those who were braced had poor outcomes. Unfortunately, due to lack of objective pressure or thermal sensors at the initiation of this study, we did not have compliance data to rigorously investigate the effects of bracing. Despite not having this information due to the study design, the probabilities presented are likely to be an underestimation of the true likelihood of reaching the 40° and 50° thresholds as these forecasts are based on the initial Cobb value rather than the treatment effect of bracing. Undoubtedly, with bracing, the probabilities will be more accurate and as such will require further studies. Nevertheless, one must be cautious to not underestimate the likelihood of poor outcomes. Despite not knowing the true bracing compliance for our patients, one is prudent to error on the side of relative overtreatment. However, this may be only true in the large initial Cobb angle group as the likelihood for reaching the surgical threshold is low for the ≤25° groups at the time of PHV. In addition, the indiscriminate use of bracing may cause physical and mental harm with spinal stiffness, poorer body image, worse self-esteem, and quality of life [111213].
There are several limitations to this study. Most significant is the lack of objective compliance data, which suggests that the probability data are an underestimation of the true risk of reaching poor outcomes. Nevertheless, the key objective of this study is to test the prediction power of the DRU classification based on the initial curve magnitude for determining outcomes. However, it appears that the radius has higher utility with a larger range of grades, including R9, which indicates a significant reduction in the risk of reaching a poor outcome. Another important limitation of the study is the assumption that curve progression patterns are similar among AIS patients, which is unlikely to be the case. Hence, the likelihood for successful bracing cannot rely only on the initial Cobb angle and DRU classification grade. Curve type may also influence the risk. Most patients with major thoracolumbar or lumbar curves do not progress to these clinically significant thresholds. It is likely that brace treatment is more effective in these curves than in those with thoracic curves [31]. The natural course of progression in AIS is not uniform, and some patients may not experience curve progression throughout growth, while others may only experience early or late deterioration. Hence, the results of this study do not indicate the duration of brace wear required. In addition, curve flexibility has been shown to greatly influence the outcomes of bracing and surgery [32333435]. This aspect of bracing, as well as the varied responses of different curve patterns, is beyond the intent of this study and should be addressed in future studies.
Conclusions
This research has shown the utility of using the DRU classification and initial Cobb angle to help forecast the likely outcome of AIS patients at skeletal maturity. With a better forecasting system for growth and curve progression, clinicians may be able differentiate which patients best respond to brace treatment without resorting to indiscriminate brace prescription and subjecting some patients to unnecessary bracing. Future studies should focus on specific effectiveness studies of bracing at certain maturity stages with proper compliance monitoring.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
This is the 2017 APSS-Asian Spine Journal Best Paper Award.