Risk Factors for Delirium after Spine Surgery: An Age-Matched Analysis
Article information
Abstract
Study Design
A retrospective cohort study.
Purpose
To investigate the risk factors for postoperative delirium after spine surgery, excluding older age, which has already been established as a strong risk factor.
Overview of Literature
More than 30 risk factors have been reported for delirium after spine surgery, making it challenging to identify which factors should be prioritized. We hypothesized that risk factors could not be prioritized to date because the factor of older age is very strong and influenced other factors. To eliminate the influence of older age, we performed an age-matched group comparison analysis for the investigation of other risk factors.
Methods
This study involved 532 patients who underwent spine surgery. Two patients of the same age without delirium (delirium negative group) were matched to each patient with delirium (delirium positive group). Differences in suspected risk factors for post-operative delirium between the two groups identified from previous reports were analyzed using univariate analysis. Multivariate analysis was performed for factors that showed a significant difference between the two groups in the univariate analysis.
Results
Fifty-nine (11.1%) of 532 patients developed postoperative delirium after spine surgery. Large amounts of intraoperative bleeding, low preoperative concentration of serum Na, high postoperative (day after surgery) serum level of C-reactive protein, low hematocrit level, low concentration of albumin, and high body temperature were detected as significant risk factors in the univariate analysis. Large amounts of intraoperative bleeding remained a risk factor for postoperative delirium in the multivariate analysis.
Conclusions
We should pay attention to and take precautions against the occurrence of postoperative delirium after spine surgery in patients of older age or those who experience severe intraoperative bleeding.
Introduction
Delirium is characterized by disturbances in attention and awareness associated with impairment in at least one cognitive function, including memory, orientation, language, visuospatial ability, or perception. These disturbances develop suddenly and fluctuate throughout the day [1]. Surgical stress associated with general anesthesia may cause a type of delirium called postoperative delirium, a clinical symptom characterized by acute attentional deficit experienced postoperatively. In general, postoperative delirium occurs after postoperative day 1 [2].
Identifying the possible risk factors for postoperative delirium may be helpful for its prevention. A large number of risk factors for postoperative delirium have been reported in connection with various types of surgery, including cardiovascular interventions, surgery for hip fracture, and total hip or knee arthroplasty [3-5]; therefore, it is unclear which factors should be considered when predicting the occurrence of this condition. Shi et al. [6] performed a meta-analysis of risk factors for postoperative delirium after spine surgery. Based on a univariate analysis of factors reported in different studies, they concluded that the most significant risk factors were older age (>60 years), female sex, polypharmacy, preoperative lower hematocrit (Hct) and albumin (Alb) levels, increased operative time and blood loss, postoperative hyponatremia, postoperative low hemoglobin (Hb) level, postoperative low Hct level, and fever. Among these, older age has been identified as a risk factor in all previous studies. Therefore, we performed an age-matched retrospective cohort study to detect risk factors for delirium after spine surgery, excluding older age.
Materials and Methods
1. Patients
This study involved 532 patients who underwent spine surgery at Ehime University Hospital from 2012 to 2014. There were 283 males and 249 females, with an average age of 64.2 years (range, 10–89 years). None of the patients had delirium or a history of delirium preoperatively. None of the patients had a history of psychiatric diseases requiring the use of psychotropic drugs. All operations were performed by one of the four senior spine surgeons having >10 years of clinical experience. All operations were performed under general anesthesia with propofol and isoflurane, enflurane complex with fentanyl, and rocuronium bromide or vecuronium bromide, and all the patients were supplied with oxygen (3–5 L/min) through a mask for at least 24 postoperative hours. The study was approved by the institutional review board at Ehime University (IRB approval no., 1801010).
2. Evaluation of delirium
The presence of delirium was determined based on the diagnostic and statistical manual of mental disorders (DSM-IV) criteria [7], which are the gold standard for psychiatric evaluation [8]. Nurses were trained for the detection of symptoms, including hyperactivity, hypoactivity, disarray, hallucination, and delusion, in patients according to the DSM-IV criteria. Patients both with and without symptoms of delirium were observed during regular postoperative care from day 0 to 7. When a patient was suspected with symptoms of delirium, the nurse called two doctors to discuss whether the patient actually had delirium. Patients were finally diagnosed as having delirium when both the doctors confirmed the diagnosis. The presence of delirium and its symptoms were recorded in the medical records after the decision.
3. Evaluation involving all the patients
The clinical records of all 532 patients were retrospectively reviewed, and patients were divided into two groups: delirium positive and negative groups. The overall and age group-related incidences of delirium were calculated, and statistical analysis was performed to compare the age between the delirium positive and negative groups.
4. Age-matched group analysis
After the evaluation of incidence in all the patients, each patient with delirium (age-matched delirium positive group) was matched with two patients of the same age in the delirium negative group (age-matched delirium negative group). The selection of patients from the database of spine surgeries was carried out by one of the co-authors who was not informed of the patients’ backgrounds. If there was no patient of the same age, we selected patients within 2 years of age difference. Risk factors in the agematched delirium positive group were compared with those in the age-matched delirium negative group. Preoperative risk factors included age, sex, ambulatory status, number of medication, smoking history, habit of alcohol use, history of surgery under general anesthesia, comorbidities (diabetes mellitus, cardiovascular disease, and neurological disorder), white blood cell (WBC) count and C-reactive protein (CRP), Hb, Hct, Alb, and sodium (Na) levels. Intraoperative factors included cervical surgery, operative time, and intraoperative blood loss. Postoperative factors included WBC count and CRP, Hb, Alb, and Na levels on postoperative day 1 and highest body temperature until the delirium or within 7 postoperative days. All the data were obtained from medical or nursing records. No patient data was lost.
5. Data analysis
All the data were analyzed using JMP ver. 9.0.3 for Macintosh (SAS Institute Inc., Cary, NC, USA). The mean age of the delirium positive and negative groups is presented as a five-number summary, whereas other numerical variables are presented as the mean and standard deviation. The Mann–Whitney U-test was used for the statistical analysis of the difference in the mean values between the groups for non-normally distributed and ordinal variables. The Student t-test was employed for normally distributed variables. The chi-square test was used to compare categorical variables. A p-value of <0.05 was considered statistically significant. Multivariate logistic regression models, with backward elimination, were constructed to find independent risk factors associated with the occurrence (positive or negative) of postoperative delirium. Factors with p<0.05 in the previous univariate analysis were included. Odds ratios and their 95% confidence intervals were calculated. A p-value of <0.05 was considered statistically significant.
Results
1. Incidence and characteristics of delirium in all patients
Delirium occurred after spine surgery in 59 of 532 patients (11.1%). The age-specific incidence of delirium and mean age at the onset of delirium (for age of 60–89 years presented in 5-year intervals) were calculated (Table 1). The incidence of delirium increased with increasing age. In the 80–84 and 85–89 years age groups, the incidence was 35.6% and 50.0%, respectively (Table 1). The mean age of the delirium positive group was significantly higher than that of the delirium negative group (77.6±6.6 versus 62.5±17.3 years, respectively; p<0.001) (Fig. 1). Almost all the cases of delirium were observed between the day of the surgery and three days after it. Two patients had delirium on postoperative days 4 and 5. All the patients recovered from the delirium by postoperative 1 week.
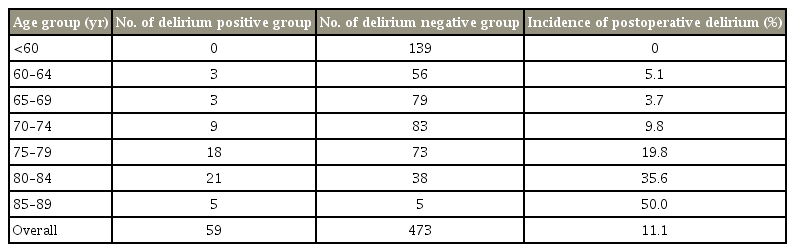
Incidence of postoperative delirium overall and according to age in the delirium positive and negative groups
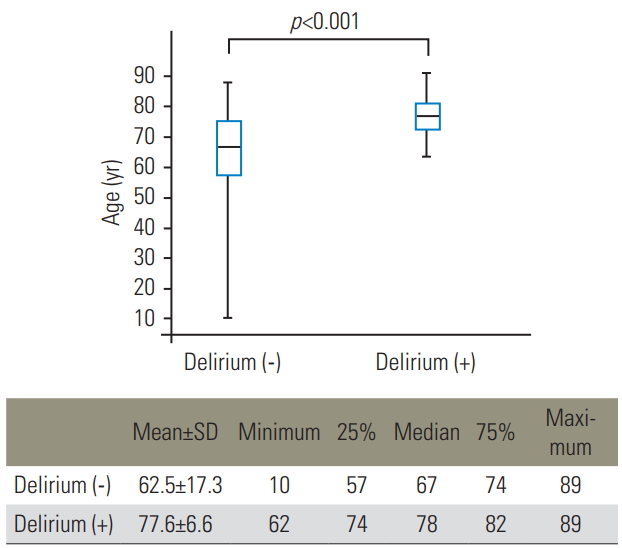
Age distribution and mean age in the delirium negative and positive groups. The upper graph shows the age distribution of each group, presented as a five-number summary. The lower table presents the mean±SD age, minimum, first quartile, median, third quartile, and maximum age for each group. A significant difference in age is seen between the two groups (p<0.001). SD, standard deviation.
2. Univariate analysis in the age-matched groups
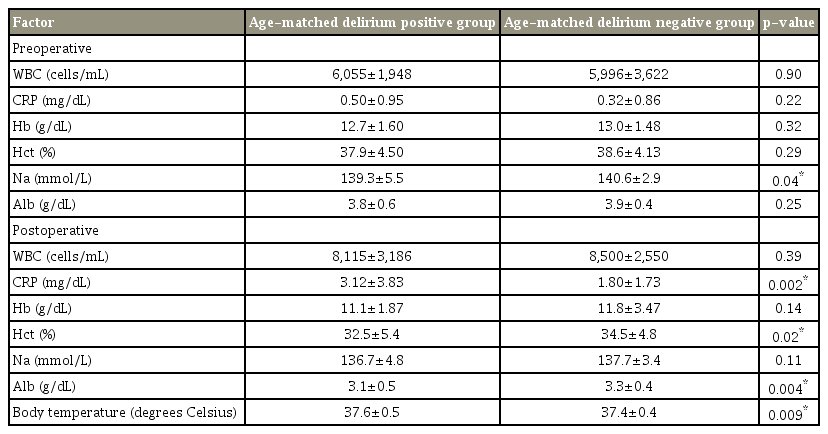
The age-matched delirium positive group included 59 patients, while the age-matched delirium negative group included 116 patients. Univariate analysis was initially performed. Regarding preoperative data, male sex, cervical operation, and nonambulatory status tended to be associated with delirium (p<0.1), but the association was not statistically significant. There was no significant difference in the number of medications, history of smoking and alcohol use, history of surgery under general anesthesia, and comorbidities (diabetes mellitus, cardiovascular disease, and neurological disease) (Table 2). Regarding the preoperative laboratory data, blood Na levels were significantly lower in the age-matched delirium positive group than in the age-matched delirium negative group (p=0.04). Other factors, including WBC count and CRP, Hb, Hct, and Alb levels, were not significant (Table 3). Regarding intraoperative data, blood loss was significantly higher in the age-matched delirium positive group than in the agematched delirium negative group (p=0.004). Longer operative times tended to be associated with delirium (p=0.055) (Table 2). Regarding postoperative data, high CRP levels, low Hct and Alb levels, and high body temperature on postoperative day 1 were identified as significant risk factors for delirium (p=0.002, 0.02, 0.004, and 0.009, respectively) (Table 3).
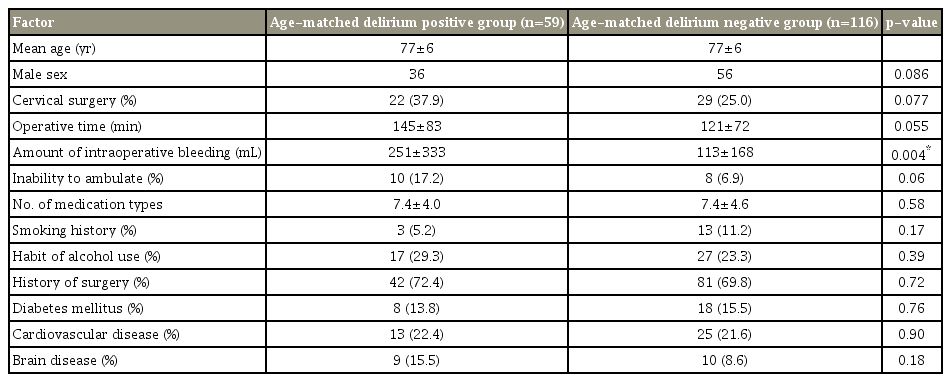
Univariate analysis of patient background and intraoperative data in the age-matched delirium positive and delirium negative groups
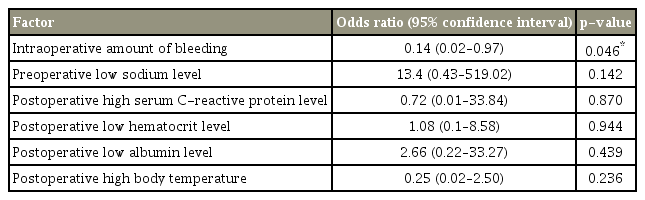
3. Multivariate analysis in the age-matched groups
Subsequently, multivariate logistic regression analysis was performed. Preoperative Na levels; intraoperative blood loss; postoperative CRP, Hct, and Alb levels; and body temperature (detected as significant risk factors of delirium in the univariate analysis) were analyzed. Intraoperative blood loss was the only significant risk factor identified (odds ratio, 7.07; 95% confidence interval, 0.02–0.97) (Table 4).
Discussion
Common symptoms of postoperative delirium are disarray, hallucination, and delusion. Patients may become hyperactive or hypoactive. Adverse outcomes have been reported in association with postoperative delirium. Patients and their families are negatively affected during hospitalization, and the condition may lead to increased mortality rates, accidents (e.g., falls and self-removal of intravenous lines), impediment to treatment, attrition of medical staff, higher medical care expenses, and elongation of hospital stay [9-12]. Moreover, after discharge, patients who experience postoperative delirium have a high likelihood of presenting to a nursing facility due to further onset of other complications or recurrence of delirium [13,14]. Thus, postoperative delirium leads to worse treatment outcomes. However, the mechanisms and prevention methods for postoperative delirium remain unclear.
Many studies have reported on postoperative delirium. Dasgupta et al. [15] reported an incidence rate of 47% after cardiac surgery and 5.1%–52% after noncardiac surgery. In orthopedics, the incidence rate of postoperative delirium has been reported to be 28%–61% after general orthopedic surgery, 26%–61% after hip fracture surgery, and 13%–41% after total hip arthroplasty [16]. The incidence seems to vary according to the type of surgery. After spine surgery, the incidence of postoperative delirium has been reported to be 3.3%–18% [17-19]. The variation in incidence may be attributed to the differences in operative stress, such as the duration of surgery and anesthesia, blood loss, pain severity, and duration of bed rest postoperatively. Therefore, research aimed at the detection of risk factors for postoperative delirium should focus on the operation type. We only analyzed patients who underwent spine surgery. In our study, the incidence of postoperative delirium was 11.1%, 15.0%, and 21.0% in all patients, those aged >60 years, and those aged >70 years, respectively. These rates were relatively similar to those reported in recent previous studies on postoperative delirium after spine surgery [17,20,21].
Numerous risk factors have been reported to be related to postoperative delirium. Almost all studies have suggested that older age is a risk factor for postoperative delirium; some studies have targeted patients aged >65 or 70 years at the beginning of the study. In the present study, older age was associated with a higher incidence of postoperative delirium. Based on these findings, older age can be considered one of the strongest risk factors for postoperative delirium. We performed an age-matched control study to eliminate the influence of age on other risk factors.
In the current study, severe bleeding was found to be a significant intraoperative risk factor for postoperative delirium (p=0.004), but longer operative time was not (p=0.055). In a meta-analysis of risk factors for postoperative delirium after spine surgery [6], both severe bleeding and longer operative time were found to be risk factors for postoperative delirium. Generally, longer operative time is associated with large amounts of bleeding, and the two factors are possibly confounding. Severe bleeding induces anemia, which decreases oxygen transport to the brain, resulting in declined brain function. The findings of our study indicated that to prevent delirium after spinal surgery, efforts should be taken to reduce intraoperative bleeding as much as possible, especially in elderly patients.
A limitation of this study was that we did not examine some risk factors that have been previously reported, such as the types of medication used preoperatively and degree of pain.
Conclusions
In the present study, we performed an age-matched analysis to identify the risk factors for postoperative delirium after spine surgery for eliminating the influence of age as a risk factor. Large amounts of intraoperative bleeding, low preoperative serum Na levels, high postoperative serum CRP levels, low Hct and Alb levels, and high body temperature were found to be significant risk factors in the univariate analysis. Large amounts of intraoperative bleeding remained a risk factor for postoperative delirium in the multivariate analysis. We should be aware of and take precautions against the occurrence of postoperative delirium after spine surgery in patients of older age and experiencing severe intraoperative bleeding.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Tadao Morino: conception and design; Masayuki Hino: data acquisition and analysis; Shintaro Yamaoka, Hiroshi Misaki, Hiroshi Imai: data acquisition; Tadanori Ogata: critical revision; and Hiromasa Miura: supervision.