 |
 |
- Search
| Asian Spine J > Volume 10(1); 2016 > Article |
Abstract
Purpose
To introduce a free-hand pedicle screw (PS) insertion technique without fluoroscopic guidance in the C7 vertebra and evaluate the procedure's feasibility and radiologic outcomes.
Overview of Literature
Although PS insertion at C7 has been recognized as a critical procedure in posterior cervical fusion surgery, conventional techniques for C7 PS have several limitations.
Methods
Thirty two patients (64 screws) who underwent PS insertion in C7 with the novel technique were included in this study. Postoperative clinical and radiological outcomes were evaluated. Special attention was paid to the presence of any problems in the screw position including cortical breaches of the PS and encroachment of the PS into the spinal canal or the vertebral foramen. This novel technique for PS insertion in C7 without fluoroscopy guidance had three key elements. First, the ideal PS entry point was chosen near the C6–7 facet joint using preoperative images. Second, the convergent angle distance was measured at axial computed tomography (CT) imaging, which defined the distance between the tip of C7 spinous process and the extended line passing through the pedicle axis from the ideal entry point. Third, the cranial-caudal angle distance was measured in sagittal CT images, which defined the distance between the tip of the C7 spinous process and the extended line passing through the pedicle axis.
Results
Cortical breach on postoperative CT images was observed in three screws. All violated only the lateral wall of the affected pedicle. The breached screws occurred in the initial five cases. Postoperative neurologic deterioration was not observed in any patient, regardless of cortical breaching.
Posterior stabilization procedures with screw-rod systems are frequently used to treat various cervical pathologies in the cervical spine including cervical stenosis, segmental instability, and fracture-dislocation [12345]. In the cervical spine, placement of a posterior screw requires a lateral mass screw, laminar screw, and a pedicle screw (PS). In all cervical vertebrae, except C1 and C7, screws are selected to accommodate the surgeon's preferences and to match the surgical situation. However, a PS is the firstline selection for posterior stabilization in C7, because the lateral mass of this vertebra is smaller than those of other vertebrae. Thus, C7 is not strong and solid enough to accommodate other screws [1267]. In addition, a laminar screw alone is not strong enough to endure segmental motion [1689]. However, the insertion of a PS in C7 is difficult due to its steep convergence angle, the lack of an apparent entry point for screw placement, and the positioning of critical structures near the pedicle, such as the spinal cord and the nerve root [1234571011].
Since careful positioning of the screw is paramount, almost every surgeon carries out PS placement under fluoroscopic guidance. Unfortunately, fluoroscopic guidance during PS placement in C7 has several drawbacks. The anatomic structures of C7, such as its pedicle and vertebral body, can be concealed by shadowing of the shoulder, which make the checked fluoroscopic image to be bootlessly (Fig. 1). There is a risk of radiation exposure for both surgeons and patients. There is a risk of contamination and postoperative infections from intraoperative medical imaging machines, such as the C-arm. Finally, the operation time is longer due to the extensive preparation required and the movements of the machine to ensure proper imaging. The problems associated with radiation exposure during surgery have received increased attention by surgeons [245612]. These studies have clearly shown that the amount of continuous radiation exposure resulting from fluoroscopic guidance for PS insertion is not negligible.
To avoid these risks of fluoroscopy, it is important to develop new fluoroscopy-free methods for better positioning a PS in C7. In this study, we describe the safety and clinical and radiological outcomes of a novel technique in C7 with PS insertion that does not require fluoroscopic guidance.
This study was approved by the Institutional Review Board of corresponding Pohang Semyeng Christianty Hospital, and informed consent was obtained from all study participants. This study was a retrospective review of medical records and radiologic images. Between March 2013 and June 2014, 32 patients (64 screws) who underwent PS insertion in C7 using our technique were enrolled. All operations were performed under a surgical microscope by a single surgeon (the corresponding author), without the aid of fluoroscopy.
This study was conducted only on the patients who complied fully with the following inclusion and exclusion criteria. The inclusion criteria were: (1) patients with compression of cervical spinal cord due to multilevel cervical spondylotic myelopathy or ossification of posterior longitudinal ligament, which were diagnosed using cervical spine radiographs and magnetic resonance imaging (MRI) that corresponded to clinical manifestations and physical examinations; and (2) patients who underwent multilevel posterior cervical fusion with PS fixation at C7 by author's technique. Those who met any of the following criteria were excluded: (1) infection or tumors in the cervical spine; (2) patients with hemorrhagic disorders, such as hemophilia and thrombocytopenia; and (3) patients judged unsuitable by the corresponding author.
All operations were performed with Mayfield tongs, with the patient in the prone position. A typical midline skin incision was made over the affected level of the cervical spine. In general, screw insertion was carried out after the main procedure, which included posterior decompression, decortication, and bone grafting to the facet joint. Prior to preparation and insertion of the PS in C7, careful periosteal dissections were performed to better expose the cortical bone and C6–7 facet joint. To achieve optimal placement of the PS in C7 without fluoroscopy using our technique, three critical elements were determined preoperatively: (1) the determination of the ideal PS entry point; (2) the convergent angle distance (CVAD); and (3) the cranial-caudal angle distance (CCAD), which were preoperatively determined with an Infinitt picture archiving and communication system (Bracknell, Berkshire, UK) and V-works three-dimensional (3D) simulation software (Cybermed Inc., Reston, VA, USA) based on preoperative fine-cut CT images. First, to choose the ideal PS entry point, a bony mark near the C6–7 facet joint, such as a tiny groove or protruded osteophyte, was initially identified at the 3D-simulated images based on preoperative CT images. Most cases had suitable bony marks near the facet joint (Fig. 2). By identifying the relationship between the bony marks and the ideal entry point and preoperatively simulating the ideal point, the actual position of the ideal entry point was identified in the surgical field. Second, the CVAD was measured preoperatively using preoperative axial CT images, which was defined as the distance between the tip of C7 spinous process and the extended line passing through the pedicle axis at the same height (Fig. 3). Finally, the CCAD was also measured preoperatively at sagittal CT images, which was defined as the distance between the tip of C7 spinous process and the extended line passing through the pedicle axis at the same height (Fig. 4). To validate the values of the CVAD and CCAD in the actual surgical situation, determination of the two distances was facilitated by the use of strict instrument such as K-wire, which aided to identify the distance from the spinous process tip of C7 to the ideal pre-determined screw trajectory measured preoperatively, as described above (Fig. 5). The ideal entry point was marked with a 1.8 mm burr, which was then advanced to a depth of approximately 1 cm with the preservation of the two pre-determined distances (Fig. 5). The determination of the ideal entry point for PS, CVAD, and CCAD can be carried out more easily with 3D-simulated images and preoperative multidirectional CT images. After verifying the absence of a cortical breach by using a ball-tipped probe, the hole was deepened for PS placement using a straight Lenke probe, which preserved the pre-determined angles. After carefully confirming the absence of a cortical breach with a ball-tipped probe in the direction of the pedicle, the PS was inserted under a surgical microscope, but without aiding fluoroscopy (Fig. 5).
Demographic, clinical, and radiologic data were retrospectively collected from medical records and radiologic images. Radiologic evaluation was performed postoperative cervical radiographs and 1.0-mm interval CT scans using a Mx8000 IDT device (Philips Medical Systems, Best, Netherlands). Special attention was paid to the presence of a cortical breach of the PS, or the encroachment of the PS into the spinal canal or the vertebral foramen (Fig. 6). A cortical breach was defined as any violation of the exterior margin of the cortical bone at the pedicle of C7. The location of a cortical breach was classified as medial, lateral, superior, or inferior to the pedicle. The following data were collected for each operation: whether or not the PS invaded the exterior margin of the cortical bone of the pedicle in any direction, and the relationship between the encroachment of the PS and its postoperative clinical manifestations. All radiologic images were analyzed by one surgeon who was not otherwise involved in this study.
Of the 32 patients (64 screws) enrolled in this study, 15 were men and 17 were female. The mean patient age was 67.8±13.0 years (range, 38–86 years). Preoperative diagnoses included 18 cervical spondylotic myelopathies, 12 diagnoses of ossification of the posterior longitudinal ligament, and two diagnoses of cervical spondylotic radiculopathy. All patients underwent a posterior fusion operation with a screw-rod system, including PS insertion into C7, by the author's technique.
Of 64 screws, cortical breach was observed in three screws, including two screws in the right PS and one screw in the left PS. The three breaches occurred in the first five patients. Outside of the initial placements, there was no cortical breach in any cases. The three breached screws violated only the lateral cortex of the pedicle. Postoperative neurologic deterioration was not observed in any of enrolled patients, including the three screws with a cortical breach.
Here, we describe a new technique for free-had PS insertion in C7 without the aid of fluoroscopy. Cortical breach of the pedicle was observed on the postoperative CT scans of three (4.7%) out of total of 64 PS screws performed by our technique, and all of the three breached screws violated the lateral cortex of the affected pedicle. No postoperative neurologic deterioration was found to be associated with a PS cortical breach. The cortical breaches occurred in the first five patients. Thereafter, no breach occurred in 27 patients (54 screws). The data presented here indicated that this technique can allows for successful PS insertion in C7. Moreover, the technique is associated with low rates of cortical breach and postoperative neurologic complications, and with a short learning-curve period. In addition, since the technique presented here was performed only under a surgical microscope, in the absence of fluoroscopic guidance, PS placement in C7 may be achieved with minimal risk of radiation exposure and minimal risk of contamination from an intraoperative medical imaging machine, such as a C-arm.
Accurate PS placement in C7 is critical for stabilizing the vertebral segments. Among the three screw types (lateral mass screw, laminar screw, and PS), PS has been recognized as a superior option for posterior stabilization due to its high degree of strength, which can endure segmental motion [1211]. Several experimental and clinical studies have demonstrated that PS screws can provide more strength for de-stabilized cervical segments compared with other screws [137]. Lateral mass screws in C7 are often suboptimal, since the lateral mass of C7 is smaller and shorter than other cervical vertebrae [1712]. The use of laminar screws is also limited in C7, because the strength of these screws to endure segmental motion has not yet been determined [1]. In addition, laminar screws are highly likely to violate the cortical bone, especially the cortical margin located near the spinal cord, which could lead to disastrous complications, such as quadriparesis due to spinal cord injury [789]. Due to the limitations of lateral mass screws and laminar screws in C7, PS has become the first-line choice for posterior stabilization in C7.
A critical drawback regarding the use of a PS in C7 is that it is extremely difficult to position accurately. Moreover, cortical breach can occur during insertion, which may result in serious complications such as spinal cord injury. Since placement of a PS in C7 requires careful screw positioning, the majority of surgeons carry out PS placement under fluoroscopic guidance.
PS insertion in C7 has been recognized as a reasonable option for posterior stabilization; however, this procedure also has several drawbacks. Most importantly, intraoperative fluoroscopic lateral images of C7 bony structures, such as the pedicle and the vertebral body, are sometimes obscured by shoulder shadows, even when the patient is positioning properly (Fig. 1). In such cases, fluoroscopy guidance is carried out during PS insertion in C7. Surgeons have long debated the best method for approaching the further insertion of the screw. In addition, the use of a radiation-emission machine, such as a C-arm, can increase the risk of contamination of the surgical field, the risk of postoperative infection, the total time of the operation due to the time needed to prepare the machine and move it into position, and can lead to higher risks of radiation exposure for both spinal surgeons and patients [2456]. Recently, the hazards of radiation exposure from intraoperative medical imaging machines have garnered much attention among spinal surgeons. Numerous articles have demonstrated that human radiation exposure exceeding a specific dose is significantly associated with mutations in human genes and tumorigenesis. Moreover, exposure also has a negative impact on human organs, such as the eyeball, thyroid, liver, spleen, and skin [6]. Due to these risks, many clinicians have attempted to minimize intraoperative imaging approaches in spinal surgery procedures. However, PS insertion in C7 without fluoroscopic guidance had rarely been described. To our knowledge, this description of a microscope-assisted free-hand PS insertion technique at C7 without the aid of fluoroscopy is novel. The three cortical breaches that occurred using this technique took place early in the study, and tended to involve the right-sided PS. Compared to the rate of cortical breach associated with free-hand PS insertion into the cervical spine, our technique exhibited a lower rate of cortical breach with no screw-related neurologic impairment [471011]. Cortical breaches were likely higher in the right PS compared with the left PS because the surgeon was right-handed, which resulted in frequent interruptions of the surgical procedure. The data presented here indicate that this technique allows for safe and feasible PS placement in C7. Moreover, this technique has a short learning-curve and may avoid the risk of radiation exposure from intraoperative imaging machines.
The present study has some limitations. First, this is a retrospective study with a relatively small sample size. To better establish the feasibility of our technique for PS placement in C7, more studies with larger sample sizes and a prospective study design should be performed. Second, the distance measurement (CCAD or CVAD) during surgery should be verified to confirm the better radiological and clinical outcomes compared to conventional technique with angle measurement, although after surgery using our technique we were convinced that the measurement of CCAD or CVAD can be associated with more simple and precisely placement at C7 PS placement than conventional technique using angle. Thus, further studies of thoroughly comparing conventional technique and novel our technique for inserting C7 PS should be necessary. Finally, the determination of the ideal entry point for C7 PS was performed based on the preoperative data from 3D-simulation software. The utilization of 3D-simulation software may be a limitation because the software has not been widely utilized. However, due to the paucity of articles describing PS insertion techniques without fluoroscopic guidance, this study can be considered to be a cornerstone for further research of free-hand techniques that do not require fluoroscopic guidance for insertion of a PS into the cervical spine.
Here, the authors introduce a new free-hand technique for PS insertion in C7. The data indicate that this technique allows safe and feasible PS placement in C7. Moreover, this technique has low rates of cortical breach and no postoperative neurologic complications, as well as a short learning-curve. In addition, since this technique was performed only under a surgical microscope without fluoroscopic guidance, it is associated with a reduced risk of radiation exposure and contamination by intraoperative imaging machines. Further studies with larger sample sizes and longer follow-up times are needed to validate the feasibility and availability of the technique.
Acknowledgements
This study was presented at Cervical Spine Research Society, Asia-Pacific section (CSRS-AP) in 2015.
Conflict of Interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Hong JT, Qasim M, Espinoza Orias AA, Natarajan RN, An HS. A biomechanical comparison of three different posterior fixation constructs used for c6-c7 cervical spine immobilization: a finite element study. Neurol Med Chir (Tokyo) 2014;54:727–735. PMID: 24418790.



2. Li J, Zhao H, Xie H, et al. A new free-hand pedicle screw placement technique with reference to the supraspinal ligament. J Biomed Res 2014;28:64–70. PMID: 24474966.


3. Liu J, Li Y, Wu Y, Zhu Q. A novel method of cervical pedicle screw placement from C3 to C5 and its clinical applications. Spine (Phila Pa 1976) 2013;38:E504–E512. PMID: 23354110.


4. Park JH, Jeon SR, Roh SW, Kim JH, Rhim SC. The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: a series of 45 consecutive patients. Spine (Phila Pa 1976) 2014;39:280–285. PMID: 24299725.


5. Wang Y, Xie J, Yang Z, et al. Computed tomography assessment of lateral pedicle wall perforation by freehand subaxial cervical pedicle screw placement. Arch Orthop Trauma Surg 2013;133:901–909. PMID: 23632781.


6. Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res 2014;472:1711–1717. PMID: 24510358.



7. Yoshihara H, Passias PG, Errico TJ. Screw-related complications in the subaxial cervical spine with the use of lateral mass versus cervical pedicle screws: a systematic review. J Neurosurg Spine 2013;19:614–623. PMID: 24033303.


8. Koltz MT, Maulucci CM, Sansur CA, Hamilton DK. C7 intralaminar screw placement, an alternative to lateral mass or pedicle fixation for treatment of cervical spondylytic myelopathy, kyphotic deformity, and trauma: a case report and technical note. Surg Neurol Int 2014;5:4PMID: 24575319.



9. Padua MR, Yeom JS, Em HT, et al. Feasibility of laminar screw placement in the upper thoracic spine: analysis using 3-dimensional computed tomographic simulation. Spine (Phila Pa 1976) 2013;38:1146–1153. PMID: 23385137.


10. Mahesh B, Upendra B, Mahan RS. The medial cortical pedicle screw--a new technique for cervical pedicle screw placement with partial drilling of medial cortex. Spine J 2014;14:371–380. PMID: 24444420.


11. Reinhold M, Magerl F, Rieger M, Blauth M. Cervical pedicle screw placement: feasibility and accuracy of two new insertion techniques based on morphometric data. Eur Spine J 2007;16:47–56. PMID: 16628443.


12. Ra IH, Min WK. Radiographic and clinical assessment of a freehand lateral mass screw fixation technique: is it always safe in subaxial cervical spine? Spine J 2014;14:2224–2230. PMID: 24704682.


Fig. 1
Preoperatively (A) and after pedicle screw placement in C7 (B), the C7 structure (asterisk), which includes the pedicle and vertebral body, can be concealed in surgical situations due to shadowing from the shoulder, despite proper positioning of the patient. This shadowing can impede interpretation of the fluoroscopic images.

Fig. 2
To identify the ideal entry point (asterisk) of the pedicle screw (PS) during surgery, a bony mark (arrows) near the C6–7 facet joint was detected for each patient during the preoperative planning for PS placement. The distance and relationship between the two points should also be acknowledged preoperatively. Ball-tipped line denotes an ideal PS trajectory of each pedicle to be determined preoperatively by the three-dimensional simulation software.
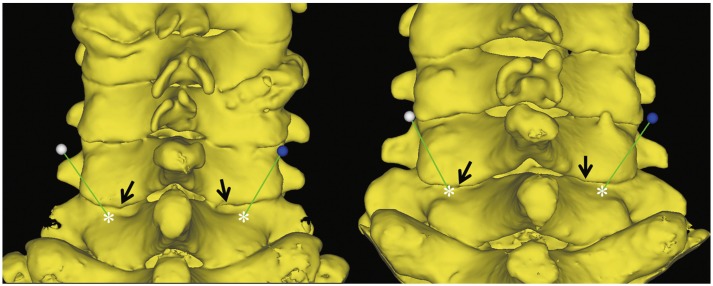
Fig. 3
The CVAD was measured preoperatively using preoperative axial computed tomography images, which was defined as the distance (a) between the tip of C7 spinous process and the extended line passing through the pedicle axis at the same height. CVAD, convergent angle distance.

Fig. 4
CCAD was also measured preoperatively at sagittal computed tomography images, which was defined as the distance (a) between the tip of C7 spinous process and the extended line passing through the pedicle axis at the same height, which line could be drew in sagittal image to see the pedicle and body of C7 well (A) and utilized the line in sagittal image to see the spinous process of C7 well (B). CCAD, cranial-caudal angle distance.
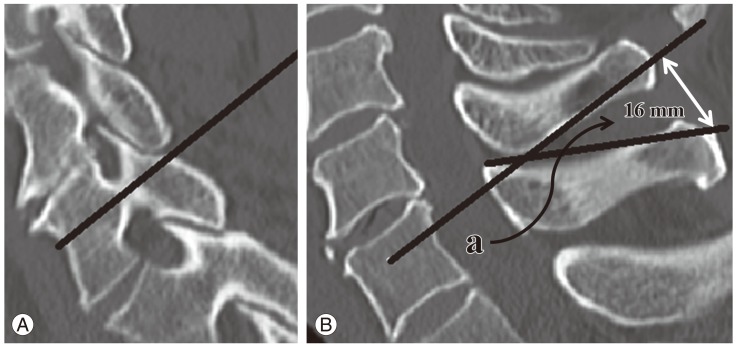
Fig. 5
The ideal entry point was marked using a 1.8 mm burr after taking into account the three elements of the ideal entry point, CVAD, and CCAD (A). The burr was readily advanced without the aid of fluoroscopic guidance (B). During surgery, the two distances were easily identified by utilizing straight bar such as K-wire (asterisk), which aided in the detection of the tip of the C7 SP. In addition, preoperatively determined distances (CVAD and CCAD) from tip of C7 spinous process were also utilized in real surgery to confirm whether the screw trajectory is correct (C). CVAD, convergent angle distance; CCAD, cranial-caudal angle distance.

- TOOLS







