|
 |
- Search
| Asian Spine J > Volume 12(3); 2018 > Article |
|
Abstract
Purpose
A new biomechanical model of the vertebra has been developed that accounts for the inhomogeneity of bone and the contribution of the pedicle toward the holding strength of a pedicle screw.
Overview of Literature
Pullout strength studies are typically carried out on rigid polyurethane foams that represent the homogeneous vertebral framework of the spine. However, the contribution of the pedicle region, which contributes to the inhomogeneity in this framework, has not been considered in previous investigations. Therefore, we propose a new biomechanical model that can account for the vertebral inhomogeneity, especially the contribution of the pedicles toward the pullout strength of the pedicle screw.
Methods
A bilayer foam model was developed by joining two foams representing the pedicle and the vertebra. The results of the pullout strength tests performed on the foam models were compared with those from the tests performed on the cadaver lumbar vertebra.
Results
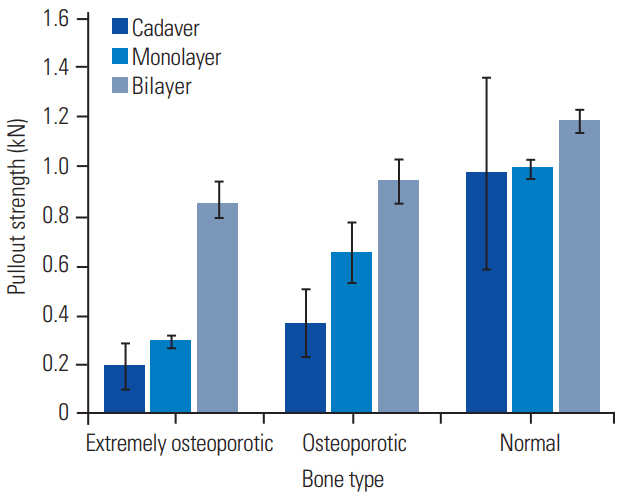
Significant differences (p <0.05) were observed between the pullout strength of the pedicle screw in extremely osteoporotic (0.18┬▒0.11 kN), osteoporotic (0.37┬▒0.14 kN), and normal (0.97┬▒0.4 kN) cadaver vertebra. In the monolayer model, significant differences (p <0.05) were observed in pullout strength between extremely osteoporotic (0.3┬▒0.02 kN), osteoporotic (0.65┬▒0.12 kN), and normal (0.99┬▒0.04 kN) bone model. However, the bilayer foam model exhibited no significant differences (p >0.05) in the pullout strength of pedicle screws between osteoporotic (0.85┬▒0.08 kN) and extremely osteoporotic bone models (0.94┬▒0.08 kN), but there was a significant difference (p <0.05) between osteoporotic (0.94┬▒0.08 kN) and normal bone models (1.19┬▒0.05 kN). There were no significant differences (p >0.05) in pullout strength between cadaver and bilayer foam model in normal bones.
Conclusions
The new synthetic bone model that reflects the contribution of the pedicles to the pullout strength of the pedicle screws could provide a more efficacious means of testing pedicle-screw pullout strength. The bilayer model can match the pullout strength value of normal lumbar vertebra bone whereas the monolayer foam model was able to match that of the extremely osteoporotic lumbar vertebra.
It is estimated that approximately 85% of adults experience lower back pain at some point in their lives [1]. According to Waddell [2], chronic lower back pain due to instability of the spine causes pain in the lumbosacral region, buttocks, and thighs. These conditions are often treated using spine-stabilization devices, which prevent the shift of vertebrae that may damage the roots of the cauda equina. The superiority of the pedicle-screw system lies in its ability to obtain osseous purchase in the vertebra until solid fusion has been achieved. The rate of revision surgeries and complications in the osteoporotic spine for spine fixation and deformity correction is approximately 30% [3].
Osteoporosis is a disease associated with decreased bone mass and strength, leading to increased fracture risk. Patients above the age of 50 years have higher rates of osteopenia and osteoporosis, reaching as high as 46% and 31%, respectively [4]. One of the problems with osteoporotic patients is the loosening of pedicle screws. Achieving a stable implant fixation to weak bones is a challenge faced by both spinal surgeons and screw designers. Therefore, a thorough understanding of the stability and fixation ability of pedicle screws is required [5]. Osteoporosis affects the cancellous bone more profoundly than the cortical bone; hence, the fixation strength of pedicle screws is weak in low-density bones. Based on the literature, it has been reported that in case of healthy spines, pedicle-screw anchorage contributes 60% of the pullout strength [6,7]. Hence, there is a need to improve the pullout strength of pedicle screws in osteoporotic bone [5].
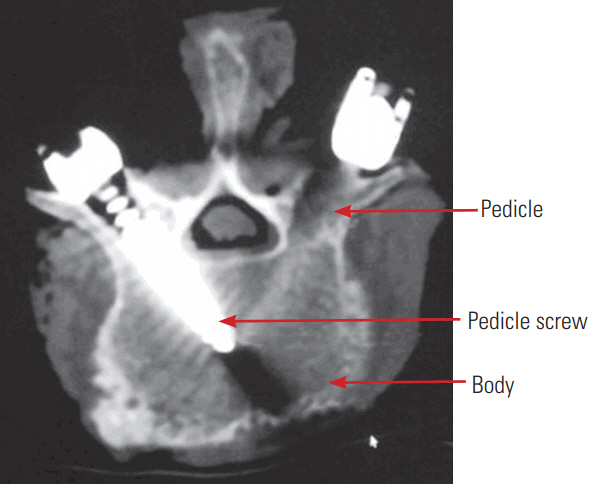
Cadaver bone surrogate models are widely used to understand the holding power of pedicle screws [8-10] but are associated with inter-individual variability of bone mineral density (BMD), size, and other complication such as availability, delicate handling, storage condition, etc. Thus, synthetic bone models made with rigid polyurethane foam aid in the development of a suitable biomechanical model of the vertebra and have been widely used in literature to study the pullout strength phenomenon [11-19]. The available research on pullout strength of pedicle screws on foam models is carried out on homogeneous foams of differing density representing osteoporotic and normal bones [10,20,21]. The pedicle region shown in Fig. 1 with a dense concentric subcortical ring surrounding the tubercular core is an important site for secure fixation, and it contributes 60% of the pullout strength at the bone-screw interface versus 15% to 20% from the vertebral body [5].
The conventional single layer foam models used for pullout strength investigations capture only the contribution of the vertebral body. Therefore, there is a need to develop better synthetic bone samples that capture the inhomogeneity of the vertebra, especially the contribution of pedicle to the pullout strength mechanism of pedicle screws. The universal use of these artificial foam models would afford researchers a cheaper, readily available, nontoxic, and easily stored cache of tools as an alternative to the fresh-frozen vertebra. Researchers have used foam blocks with epoxy resin matrix [22] to represent humeri to study the pullout strength of bicortical screws. However, no such models/studies have been reported in literature in case of pedicle screws. Hence, the objective of the current study was to design and test the capabilities of a bi-layer model of polyurethane foam to determine pedicle screw pullout strength and to determine if it is a closer representation of actual vertebra in comparison with monolayer foam model. To accomplish this, the pullout strength of pedicle screws with the proposed model were compared with the conventional monolayer foam models and cadaver lumbar spine specimens. Important considerations for the current investigation were that the complex geometry of the vertebra was not considered, as it was assumed that the geometry influences the loading pattern physiologically. Only axial pullout strength was considered as the scope of the paper was to represent the initial holding power of pedicle screws. Other loading conditions such as cyclic loading were also not considered.
A commercial polyaxial, cylindrical, and self-tapping pedicle screw (M8, Medtronic; Sofamor Danek, Memphis, TN, USA) of length 40 mm and outer diameter 5.5 mm made from medical grade titanium alloy was used in this investigation (Fig. 2). The dimensions of the pedicle screw were: outer diameter, (Douter)=5.5 mm; inner diameter, (Dinner)=3.9 mm; thread length, (L)=40 mm; and pitch, (p)=2.7 mm.
Polyurethane foam models help to reduce the interindividual variability of size, BMD, non-homogeneity of bone, geometry, etc. and is widely used for the representation of vertebra [8,16,17,23]. Conventionally, a monolayer of homogeneous polyurethane foam of different density is used to represent bones of differing density. The foams for the current study were obtained from Polynate Foam (Polynate Foams Pvt. Ltd., Bangalore, India) and adhered to the American Society of Testing Materials (ASTM F1839; ASTM, West Conshohocken, PA, USA) standards for use as standard material for testing of orthopedic devices and instruments [24]. The material properties and equivalent representation of the bone type are presented in Table 1. The foam block was cut into 60 mm├Ś120 mm├Ś45 mm dimensions as shown in Fig. 3A.
The proposed bilayer model in this study is designed to represent the vertebra and the pedicle and consists of two layers of foam as shown in Fig. 3B. The bottom layer of foam represents standardized human bone densities of cancellous bone according to grades. A 20-mm thick layer of 300 kg/m3 foam glued to this foam represents the cortico-cancellous pedicle [25]. The thickness of the corticocancellous region was selected based on the anatomical size of the pedicle [26].
Pilot holes were drilled (in both monolayer and bilayer models) along the longitudinal axis of the pedicle screw with a drill bit of 3.2 mm diameter. Holes were drilled 25 mm away from each other to avoid interaction effects. The foam block instrumented with pedicle screw was placed on a jig for the pullout strength test as shown in Fig. 4A.
Pullout strength studies in cadaver lumbar spine samples were performed to compare the pedicle-screw pullout values obtained in conventional monolayer foam models and the proposed bilayer foam models. Three embalmed intact lumbar spines (L1ŌĆōL4) were obtained from the anatomy department of Christian Medical College, Vellore, Tamil Nadu, India. And the Institutional Review Board clearance is not required for the study. Specifications included age, gender, BMD, and T-score as described in Table 2. Vertebrae exhibiting fracture, osteophytes, or severe disc degeneration were excluded from further testing after visual and radiographic inspections. Soft tissues such as muscle and ligaments were left intact to represent the in vivo condition. BMD and bone mineral content were obtained using a dual energy X-ray absorptiometry (DEXA) scanner (Discovery A; Hologic Inc., Bedford, MA, USA). Muscles were removed but ligaments were kept intact before instrumenting with the pedicle screw. Pilot holes were drilled and taps were created using tapping screws. Pedicle-screw insertion was performed by a spine surgeon using a free-hand technique. Pedicle screws were placed unicortically. A computed tomography (CT) scan was performed on the instrumented specimen to check for any wall breach by the screw. Pedicle screws were attached to a 5.5-mm diameter rod inserted into the screw heads (as shown in Fig. 4B) and connected to the testing machine using a special jig. The specimen was then placed in such a manner that the pedicle-screw axis was coaxial with the pullout direction on the jig.
The depth of the pilot hole and screw insertion into the foam blocks were the same as those in the cadaveric specimens. A 5.5-mm diameter tensile steel rod was fixed to the pedicle screw using a set screw mimicking the actual configuration of the pedicle screw. This was fixed to the universal chuck on BiSS Nano-25 (Bangalore Integrated System Solutions Pvt. Ltd., Bangalore, India) having a specification of 15 kN force actuator operating at 50 Hz data acquisition. A 5 mm/min of the tensile load was applied to the test specimen until the screw released from the test block. The procedures were controlled under the provision of ASTM F543-07 protocol [27]. Load and displacement values were recorded, and the maximum load generated during screw pullout was defined as the pullout strength.
Statistical analyses were carried out using two-tailed Student t-test with equal variance at 0.05 level of significance (p<0.05).
The cross-sectional view of the failed sample in bilayer and monolayer foam models is shown in Fig. 5. It can be seen that the failure occurred at the threadŌĆōfoam interface and not at the interface between the two foams. An additional experiment was carried out to rule out the influence of the adhesive used to join foam blocks on pullout strength of pedicle screws in bilayer foam models. Based on the study it was found that there is no significant difference (p>0.05) between the pullout strength of foam models which were joined using adhesives and joined by clamping the two foam blocks. Thus, the pullout values in bilayer synthetic foam models developed in this study are dependent on the foam properties only.
The pullout strength increased with an increase in density, which was the case for cadaver lumbar vertebra (Fig. 6). A significant difference (p<0.05) was observed in pullout strengths between the different bone types. Pullout strength was highest in normal bone (0.97┬▒0.39 kN) and was the lowest in extremely osteoporotic bones (0.17┬▒0.11 kN). There was a significant 62% decrease (p<0.05) in pullout strength between normal and osteoporotic bones (0.60 kN). In cases of osteoporotic and extremely osteoporotic bones, there was a statistically significant 51% decrease (p<0.05) in pullout strength (0.19 kN). The pullout strength of the pedicle screw increased with an increase in density in both monolayer and bilayer foam models (Fig. 6).
The highest pullout strength in the monolayer model was observed in normal (0.240 g/cm3) bone models at 0.99┬▒0.04 kN, whereas the lowest pullout strength was observed in the extremely osteoporotic bone models (0.080 g/cm3) at 0.30┬▒0.02 kN. There was a significant 34% decrease (p<0.05) in pullout strength between osteoporotic and normal bones (0.34 kN). There was a 54% decrease (0.35 kN) in pullout strength between osteoporotic to extremely osteoporotic bone models, and the difference was significant (p<0.05).
No significant differences (p>0.05) were observed in the pullout strength between osteoporotic (0.85┬▒0.08 kN) and extremely osteoporotic bone models (0.94┬▒0.08 kN), a 10% (0.09 kN) in the bilayer foam model. There was a significant difference (p<0.05) in the pullout strengths between the osteoporotic (0.94┬▒0.08 kN) and normal bone model (1.19┬▒0.05 kN), a 21% decrease (0.25 kN) was observed.
In the extremely osteoporotic model, there were no significant differences (p>0.05) in pullout strengths between cadaver and monolayer models. However, there was a significant difference (p<0.05) between cadaver and bilayer models.
Significant differences (p<0.05) were observed in pullout strengths between the cadaver and both the foam models in the osteoporotic comparisons. In case of the normal model, there were no significant differences (p>0.05) in pullout strengths between cadaver and both the foam models.
A steady effort to develop pedicle screws with improved fixation capabilities to provide high-quality fixation devices for spinal surgery is underway worldwide. Surgeons, design engineers, radiologists, and statisticians have all contributed toward developing these screws, which are currently on par with those used in fixations available for long bones [28]. This study was designed to create a vertebral model that can be used to study the factors affecting the holding power of pedicle screws. These screws rely primarily on the cancellous bone for purchase, with the pedicle providing approximately 60% of the pullout strength [5]. Screw loosening has been reported to occur at the bone-screw interface due to mechanical failure or instability in osteoporotic subjects [29]. The pullout strength of the screws inserted in osteoporotic bone becomes a crucial quality, particularly as the patient ages; as osteoporosis deteriorates the bone tissue enhancing the possibility of fracture and also poses challenges in treating fractures. Studies with human cadaver models have a restriction regarding availability and inter- and intra-sample variation. It is challenging to develop animal models for osteoporosis research as it involves hormonal intervention or dietary restrictions that significantly increase cost and length of experiments. Hence, there is a need to establish a vertebral model for studying the pullout strength phenomenon of pedicle screws.
This study aimed to develop a bone model that captures the inhomogeneity of the vertebra and the contribution of the pedicle, which is one of the most crucial anatomic structures in reconstructive spinal surgery toward holding power of pedicle screws. In the current investigation, a bilayer synthetic model was developed, which represented the inhomogeneity of the vertebra and also the pedicle region. This model showed no significant differences (p>0.05) in pullout strength compared with that of a bone of normal density. Also, the bilayer model was able to match the trend in change of pullout strengths with density more closely with the cadaver results (i.e., the decrease in pullout strength from normal density to osteoporotic bone is more when compared to that between osteoporotic and extremely osteoporotic bones). In the monolayer foam model, the increase in pullout strength between the different densities shows a linear trend, which is not the case with cadaver bones where the trend is nonlinear. This phenomenon is more evident in the bilayer model compared with the monolayer model. This difference in trend might be caused due to the difference in bone architecture at the vertebral body and pedicle region. Pullout strength of the bilayer foam model was higher than monolayer foam model for all foam densities. This is probably owing to the presence of denser foam layers representing pedicle in the bilayer model. There was no significant difference (p<0.05) in pullout strength between extremely osteoporotic model using cadaver and monolayer model. Hence, monolayer foam model can be used for representing extremely osteoporotic vertebra.
The architectural development of trabecular bone in the pedicle plays a critical role in determining the holding power of pedicle screw. A recent report by Inceoglu et al. [30] demonstrates the differences in the trabecular architecture of the pedicle and vertebral body, and that the bone volume fraction within the pedicle isthmus could not be predicted by vertebral BMD. Trabeculae of the pedicle are thicker, more isotropic, and exhibit plate-like characteristics with less spacing network [30], whereas in the vertebral body, they are anisotropic. This suggests that measurements of BMD within the pedicle before surgery in spine patients could provide a better sense of fixation quality. It may also be feasible, and important to treat the elderly spine patients before surgery to increase the strength of pedicular cancellous bone and to improve fixation quality. DEXA scans are used to measure the density of vertebra in the clinic. This provides a density measurement of the whole vertebra. The contribution of the facet joint and spinous process influences the measurement of the density. This can lead to an unnecessary increase in measured density. A new protocol aimed at measuring the density of individual regions of a vertebra, such as quantitative CT (qCT) would help in estimating the strength of the pedicle region. Currently, qCT results in additional patient radiation exposure. Hence, the development of low-intensity radiation techniques for better visualization and quantitative estimation of the strength of vertebra without other risks is warranted.
In the proposed bilayer model, it was assumed that the pedicle region is unaffected by osteoporosis and hence the uniform density of foam was used to represent the cortical-cancellous region. Due to this assumption, the pullout strength value obtained for the bilayer model is higher than the cadaver lumbar vertebra. Until now, due to the lack of available literature, the impact of osteoporosis on the pedicle region has been considered to be uniform. However, improved imaging and histological techniques will help in aiding our understanding of this phenomenon. Further studies aimed at understanding the strength of each region of the vertebra, such as a pedicle, facet joints, spinous process could aid in building a model closer to that experienced in the clinic. Additional tests with E-glass-filled epoxy sheets of differing thicknesses attached to a stable, rigid polyurethane foam would mimic the cortical layer on the cancellous bone block and evaluated for studying the role of cortical bone thickness on the primary stability of pedicle screws. The current investigation demonstrates that while the absolute values of pullout strength remained markedly different, the patterns of pullout strength were very similar between the two testing models. This can be attributed due to variation in the cadaveric sample due to intra-individual non-homogeneity, geometric and material properties of bone. Better imaging and histological studies will help in understanding the osteoporosis at pedicle region, and its density can be measured and used to create better biomimetic synthetic foam models.
One limitation of the current study is that only a simple axial loading was studied, which represented the initial holding period of the pedicle screw. Furthermore, the inhomogeneity due to the presence of fat, bone marrow, and blood inside the vertebra is challenging to model in a foam model. It was assumed that the contribution of these components is negligible. The current results apply to the screws of dimensions as described. Hence, caution should be exercised while extrapolating the results to other screw types.
The current study was aimed at developing a new synthetic bone model of the vertebra which could be used to study the inhomogeneity of vertebra and the contribution of the pedicle region for the pullout strength of pedicle screws. The model consisted of bilayer foam that reflects the density differences between cortico-cancellous pedicle and the cancellous vertebral body. This model was compared with results produced from tests done on a cadaver bone model. The bilayer model proposed here could be used to represent a typical bone for studying pullout strength phenomenon. The monolayer model can be used to describe extremely osteoporotic bone as it was able to match the pullout strength.
Acknowledgments
The authors would like to thank Suresh J.A, Lab in charge, Fatigue Lab, Department of Engineering Design, IIT Madras for helping in designing the fixtures and carrying out the experiments.
Fig.┬Ā3.
Foam model used in the current study. (A) Conventional monolayer foam model and (B) bilayer foam model.
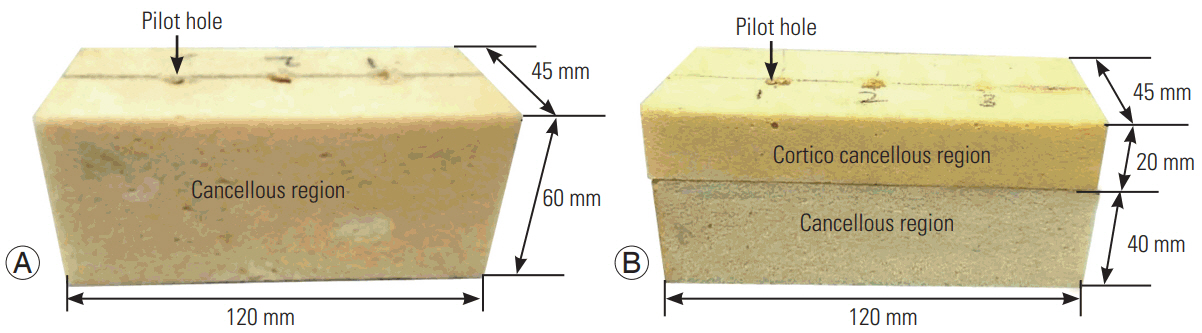
Fig.┬Ā4.
Experimental setup for studying pullout strength for (A) synthetic bone samples and for (B) cadavers.
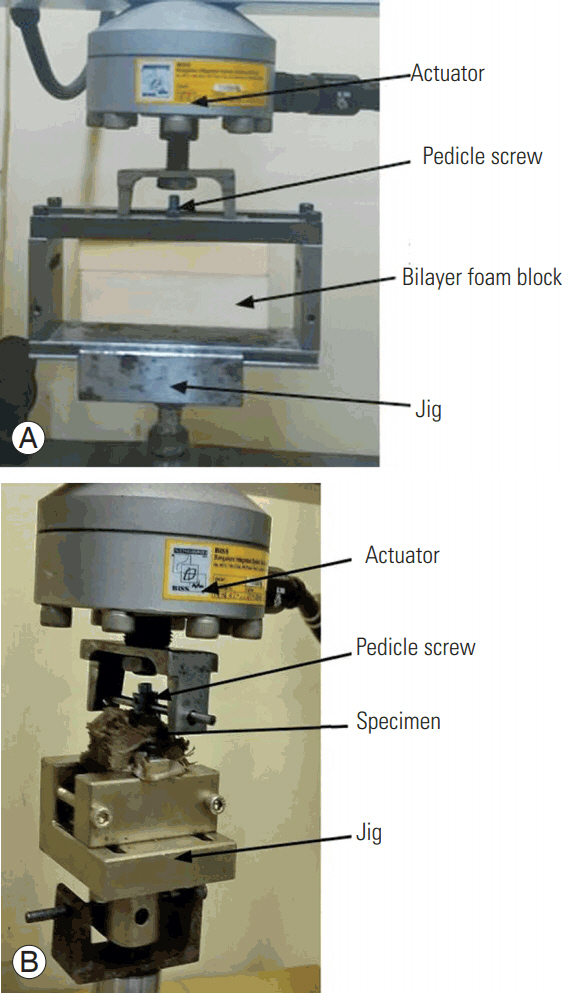
Fig.┬Ā5.
A cross-sectional view of the failed sample. (A) Monolayer foam model and (B) bilayer foam model.
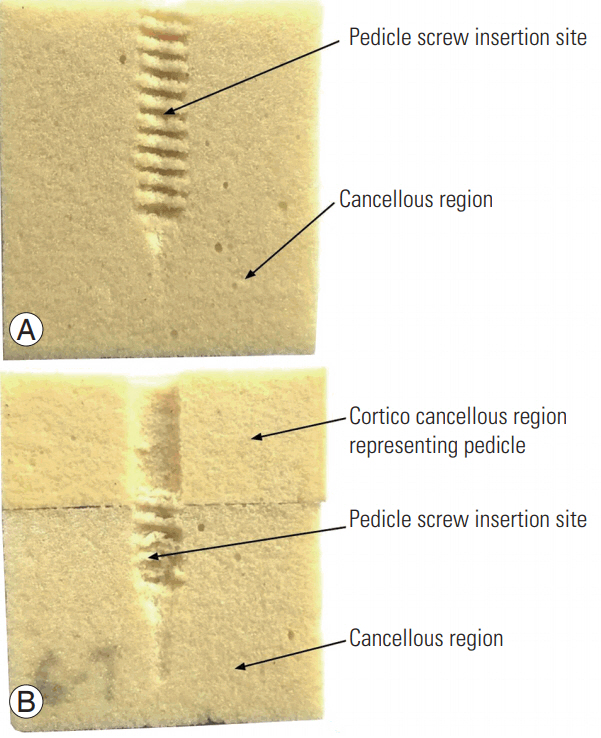
Fig.┬Ā6.
Effect of density on the pullout strength of pedicle screws in monolayer and bilayer foam models.
Table┬Ā1.
Material property of foam used in the study
| No. | Bone type | Density (g/cm3) |
|---|---|---|
| 1 | Extremely osteoporotic | 0.080 |
| 2 | Osteoporotic | 0.160 |
| 3 | Normal | 0.240 |
| 4 | Cortico-cancellous | 0.300 |
Table┬Ā2.
BMD measurement of the samples and corresponding bone types
References
1. Heliovaara M, Makela M, Knekt P, Impivaara O, Aromaa A. Determinants of sciatica and low-back pain. Spine (Phila Pa 1976) 1991;16:608ŌĆō14.


2. Waddell G. The back pain revolution. 2nd ed. Edinburgh: Churchill Livingstone; 2004.
3. Mok JM, Cloyd JM, Bradford DS, et al. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine (Phila Pa 1976) 2009;34:832ŌĆō9.


4. Chin DK, Park JY, Yoon YS, et al. Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int 2007;18:1219ŌĆō24.


5. Hirano T, Hasegawa K, Takahashi HE, et al. Structural characteristics of the pedicle and its role in screw stability. Spine (Phila Pa 1976) 1997;22:2504ŌĆō9.


6. Becker S, Chavanne A, Spitaler R, et al. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur Spine J 2008;17:1462ŌĆō9.



7. Burval DJ, McLain RF, Milks R, Inceoglu S. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976) 2007;32:1077ŌĆō83.


8. Inceoglu S, McLain RF, Cayli S, Kilincer C, Ferrara L. Stress relaxation of bone significantly affects the pullout behavior of pedicle screws. J Orthop Res 2004;22:1243ŌĆō7.


9. Tolunay T, Basgul C, Demir T, Yaman ME, Arslan AK. Pullout performance comparison of pedicle screws based on cement application and design parameters. Proc Inst Mech Eng H 2015;229:786ŌĆō93.


10. Arslan AK, Demir T, Ormeci MF, Camuscu N, Tureyen K. Postfusion pullout strength comparison of a novel pedicle screw with classical pedicle screws on synthetic foams. Proc Inst Mech Eng H 2013;227:114ŌĆō9.


11. Krishnan V, Varghese V, Kumar GS. Comparative analysis of effect of density, insertion angle and reinsertion on pullout strength of single and two pedicle screw constructs using synthetic bone model. Asian Spine J 2016;10:414ŌĆō21.



12. Varghese V, Venkatesh K, Kumar GS. Pull out strength of pedicle screw in normal and osteoporotic cancellous bone models. In: Proceedings of the 2014 IEEE Conference on Biomedical Engineering and Sciences (IECBES); 2014 Dec 8-10; Miri, Malaysia. Piscataway (NY). Institute of Electrical and Electronics Engineers. 2014 https://doi.org/10.1109/IECBES.2014.7047541

13. Varghese V, Ramu P, Krishnan V, Saravana Kumar G. Pull out strength calculator for pedicle screws using a surrogate ensemble approach. Comput Methods Programs Biomed 2016;137:11ŌĆō22.


14. Varghese V, Saravana Kumar G, Krishnan V. Effect of various factors on pull out strength of pedicle screw in normal and osteoporotic cancellous bone models. Med Eng Phys 2017;40:28ŌĆō38.


15. Varghese V, Kumar GS, Venkatesh K. A finite element analysis based sensitivity studies on pull out strength of pedicle screw in synthetic osteoporotic bone models. In: Proceedings of the 2016 IEEE EMBS Conference on Biomedical Engineering and Sciences (IECBES); 2016 Dec 4-8; Kuala Lumpur, Malaysia. Piscataway (NY). Institute of Electrical and Electronics Engineers. 2016 https://doi:10.1109/IECBES.2016.7843478

16. Yaman O, Demir T, Arslan AK, et al. The comparison of pullout strengths of various pedicle screw designs on synthetic foams and ovine vertebrae. Turk Neurosurg 2015;25:532ŌĆō8.

17. Demir T, Camuscu N, Tureyen K. Design and biomechanical testing of pedicle screw for osteoporotic incidents. Proc Inst Mech Eng H 2012;226:256ŌĆō62.


18. Varghese V, Krishnan V, Kumar GS. Simulation of axial pull out of pedicle screw in synthetic bone models. In: Proceedings of the 2nd International Conference on Biomedical Systems, Signals and Images; 2016 Feb; Chennai, India. https://doi.org/10.13140/RG.2.1.3355.8643

19. Demir T, Basgul C. The pullout performance of pedicle screws. Cham: Springer International Publishing; 2015.
20. Kim YY, Choi WS, Rhyu KW. Assessment of pedicle screw pullout strength based on various screw designs and bone densities: an ex vivo biomechanical study. Spine J 2012;12:164ŌĆō8.


21. Chen YL, Chen WC, Chou CW, et al. Biomechanical study of expandable pedicle screw fixation in severe osteoporotic bone comparing with conventional and cement-augmented pedicle screws. Med Eng Phys 2014;36:1416ŌĆō20.


22. Zdero R, Shah S, Mosli M, Bougherara H, Schemitsch EH. The effect of the screw pullout rate on cortical screw purchase in unreamed and reamed synthetic long bones. Proc Inst Mech Eng H 2010;224:503ŌĆō13.


23. Aycan MF, Tolunay T, Demir T, Yaman ME, Usta Y. Pullout performance comparison of novel expandable pedicle screw with expandable poly-ether-etherketone shells and cement-augmented pedicle screws. Proc Inst Mech Eng H 2017;231:169ŌĆō75.


24. ASTM International. ASTM F1839-08(2016): standard specification for rigid polyurethane foam for use as a standard material for testing orthopaedic devices and instruments [Internet]. West Conshohocken (PA): ASTM International. 2016 [cited 2017 Apr 16]. Available from: https://www.astm.org/Standards/F1839.htm
25. Hickerson LE, Owen JR, Wayne JS, Tuten HR. Calcium triglyceride versus polymethylmethacrylate augmentation: a biomechanical analysis of pullout strength. Spine Deform 2013;1:10ŌĆō5.


26. Mitra SR, Datir SP, Jadhav SO. Morphometric study of the lumbar pedicle in the Indian population as related to pedicular screw fixation. Spine (Phila Pa 1976) 2002;27:453ŌĆō9.


27. ASTM International. ASTM F543-07e1: standard specification and test methods for metallic medical bone screws [Internet]. West Conshohocken (PA): ASTM International. 2016 [cited 2017 Apr 16]. Available from: https://doi.org/10.1520/F0543-07E01

28. Gaines RW Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am 2000;82-A:1458ŌĆō76.

- TOOLS