Clinical Outcomes of Surgical Treatments for Traumatic Spinal Injuries due to Snowboarding
Article information
Abstract
Study Design
Retrospective study.
Purpose
To assess treatment outcomes of snowboarding-related spinal and spinal cord injuries.
Overview of Literature
Snowboarding-related spinal or spinal cord injury have a great impact on social and sporting activities.
Methods
A retrospective review of 19 cases of surgically treated snowboard-related injury was done. Analyzed parameters included site of injury, type of fracture, peri- and postoperative complications, pre- and postoperative neurological status, activities of daily living, and participation in sports activities at the final follow-up.
Results
The major site of injury was the thoracolumbar junction caused by fracture-dislocation (13/19 cases). The remaining 6 cases had cervical spine injuries. Over 60% of the patients had Frankel A and B paralysis. All patients were surgically treated by posterior fusion with instrumentation. Five underwent additional anterior fusion. Surgical outcome was restoration of ambulatory capacity in 12 patients (63.2%). Ultimately, 15 patients (78.9%) could return to work. Patients with complete paralysis upon admission showed reduced ambulatory capacity compared to those with incomplete paralysis. None of the patients again participated in any sports activities, including snowboarding.
Conclusions
Snowboarding-related spinal or spinal cord injury has a great impact on social as well as sports activities. It is necessary to enhance promotion of injury prevention emphasizing the snowboarders' responsibility code.
Introduction
The huge popularity of snowboarding has rapidly changed the scene of ski slopes worldwide. Data from Europe and North America have indicated that as much as 50% of the mountain slopes are occupied by snowboarders in some resorts [1]. Unfortunately, this surge in popularity has been accompanied by an increase in the incidence of snowboarding-related trauma [2,3], notably head and spinal injuries [4,5,6]. Spinal cord injuries, along with severe head injuries, are the most devastating and costly types of injury associated with recreational sports. Head and spinal injuries account for an estimated 4%-28% of all snow sports-related injuries, with the majority of cases being mild in nature [7]. Generally, spinal injuries associated with snowboarding tend to occur in young men (94.4%), due to jumping failures (83.3%), and at the thoracolumbar junction (66.7%) accompanied by severe paralysis classified as Frankel A or B (83.3%) [8]. Although there have been reports of snowboarding injuries, little information is available regarding their neurological involvement, including clinical course after operations, return to work, and return to playing sports. We performed a retrospective study of our experience and clinical outcomes in treating 19 patients with traumatic spinal cord injury, associated with vertebral fractures resulting from snowboarding accidents.
Materials and Methods
1. Subjects
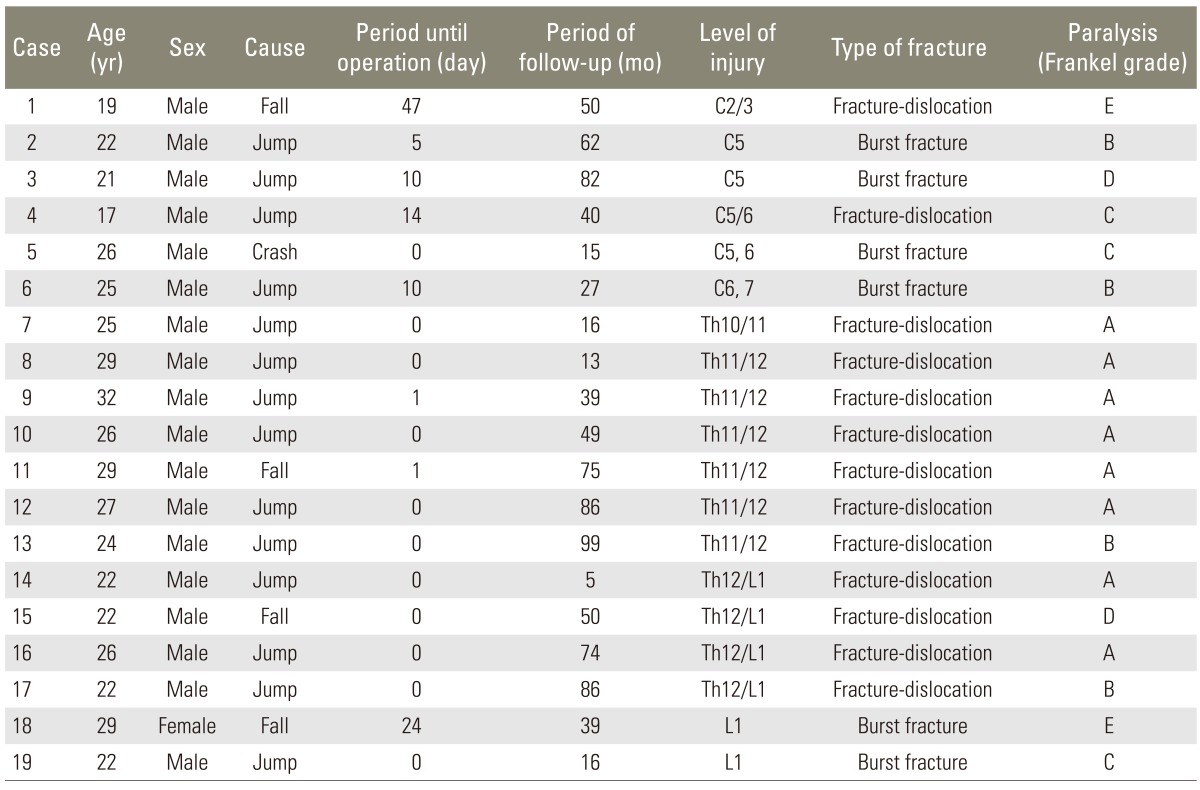
Subject information is summarized in Table 1. Nineteen patients (18 men and 1 woman) with spinal injuries due to snowboarding who underwent operations at our institution between 1997 and 2009 were assessed retrospectively. Diagnoses were made by physical examination and imaging information from X-ray and computed tomography (CT). Presently, patients with severe spinal injuries are transferred by helicopter through primary emergency hospitals; transport to our hospital takes only 20 to 30 minutes. Our prefecture has many ski facilities serviced by the highway and the number of participants coming from other nearby prefectures is increasing. Therefore, most of the injured patients tend to be residents from other prefectures. To facilitate the early transfer of these patients to their home area, they undergo operations with implantation as soon as possible depending on their general condition. Even in patients with complete spinal cord injury, it is prudent to perform operations earlier to secure damaged neural structures and promote early rehabilitation. A delay may have led to complications, such as pneumonia, pressure sores, and venous thrombosis. All patients received intravenous methylprednisolone within 8 hours of injury in accordance with a published protocol [9].
On admission to our hospital, informed consent is routinely sought for the use of patient data in clinical studies. The present study was approved by the Institutional Review Board of Gifu University Graduate School of Medicine.
2. Assessment of clinical outcomes
The clinical features of these patients were reviewed with respect to the nature of their spinal cord injuries, including the site of injury, fracture pattern, and neurological status. Neurological status was graded according to the Frankel scale (grade A, complete; B, sensory only; C, motor useless; D, motor useful; E, recovery) [10]. The patients were also classified into two groups with regard to primary paralysis. The complete group consisted of Frankel grade A and the incomplete group consisted of the other grades. For assessment of surgical interventions, the operation time, blood loss, and peri- and postoperative complications were assessed. Changes in neurological improvement, status of daily life, work and sports activities, and participation in any type of sports activity, including snowboarding, were assessed. These outcomes were compared between the Complete and incomplete groups.
3. Statistical analysis
Differences between patients in the complete and incomplete groups were assessed statistically using Stat View ver. 5.0 (SAS Institute, Cary, NC, USA). Final neurological status of Frankel type was assessed by chi-square test, while ambulatory capacity and other status were assessed by Fisher's exact probability test. In all analyses, p < 0.05 was taken to indicate statistical significance.
Results
1. Clinical features
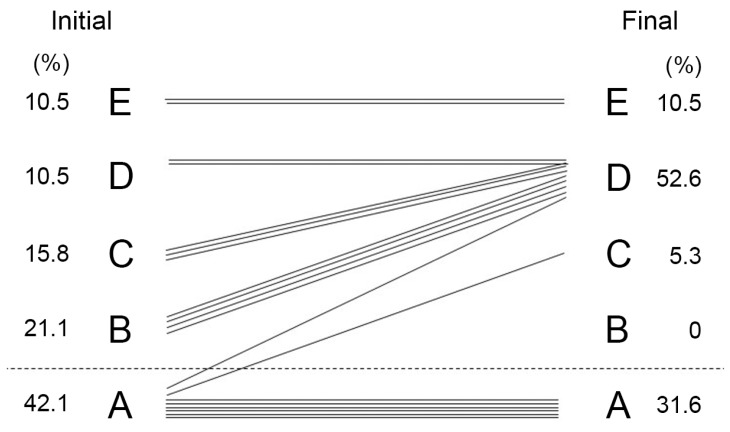
Clinical features are summarized in Table 1. The average age of patients was 24.5 years (±standard deviation [SD], 3.8; range, 17-32 years). The injuries were due to jumping failures in 14 cases, falls in 4 cases, and a crash in 1 case. The average period of postoperative follow-up was 49.6 months (±SD, 31.6; range, 5-99 months). The average period from admission to operation was 5.4 days (±SD 12.1; range, 0-47 days). While most of the patients underwent an emergency operation on the day of injury, 2 cases without neurologic injury (Frankel type E, cases 1 and 18) (Table 1) underwent surgery later. The major site of injury was the thoracolumbar junction (13 cases), followed by the cervical spine in 6 cases. The fracture patterns were burst fractures in 1 of the 13 injuries at the thoracolumbar junction and 4 of the 6 cervical injuries. The others were all anterior fracture-dislocation. Paralysis was classified as Frankel type A (n=8), B (n=4), C (n=3), D (n=2), and E (n=2). More than 60% of the patients sustained severe paralysis (Frankel type A or B) (Fig. 1). All of the patients classified as Frankel type A had sustained fracture-dislocation at the thoracolumbar junction caused by high energy impact.
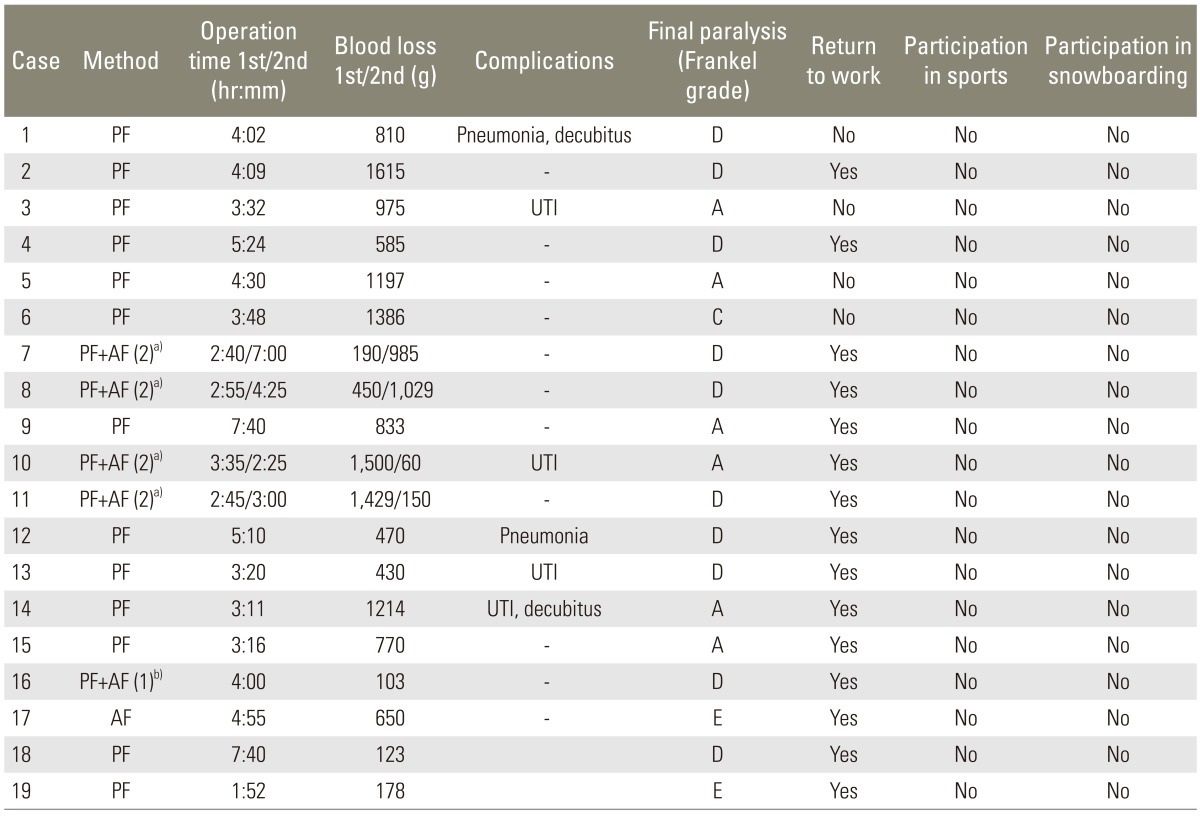
2. Operative assessment (Table 2)
Eleven of the 19 patients underwent an emergency operation. Only 1 patient with cervical injury underwent one-stage operation with anterior and posterior fusion, while the others underwent posterior fusion during the first operation. Four patients with thoracolumbar junction injury underwent anterior fusion at the second operation. The operation time was 247 (±SD 91) minutes at the first operation (n=19) and 252±122 minutes at the second operation (n=4). Blood loss was 784±493 g in the first operation and 556±522 g in the second operation. We performed autotransfusion if possible. Two patients developed pneumonia postoperatively. These patients had cervical spine injury, Frankel type B paralysis, and underwent operations on several occasions. Three of 4 patients who developed urinary tract infections (UTI) belonged to the complete group. The severe bladder disorder due to the spinal cord injuries in these patients may have led to a tendency to develop UTI.
3. Postoperative activities of daily living (ADL), sports, and participation in sports activities in patients with complete and incomplete paralysis at the onset of injury
1) Neurological assessment and ADL after surgery (Table 3, Fig. 1)

Postoperative activities of daily living, sports, and participation in sports in patients with complete and incomplete paralysis at the onset of injury
The primary paralysis in 6 of 8 patients with Frankel type A did not improve, while that in the other 2 patients improved to Frankel type D. Most of the patients classified as Frankel type B or C showed improvement in paralysis to Frankel type D (Fig. 1). Finally, 7 of 8 patients in the complete group required a wheelchair at the final follow-up. The other 12 patients (63.2%) could walk with or without assistance at the final follow-up, including 7 patients initially classified as Frankel type B or C. Fifteen patients (78.9%) returned to work, but none participated in sports activities since their spinal injury. There were no significant differences in the rates of returning to work or participation in sport activities between the Complete and incomplete groups (Table 3). Furthermore, 13 patients (68.4%) still had neurological bladder disorder, comprising 7 of 8 patients in the complete group (87.5%) and 6 of 11 patients in the incomplete group (54.5%).
4. Case reports
1) Case 1
A 26-year-old man had incomplete tetraplegia (Frankel type C) after crashing into a tree while snowboarding. The results of X-ray and CT scan showed burst fracture (flexion-compression) in C5 and C6 (Fig. 2). On the same day as the injury, the patient received intravenous administration of methylprednisolone, and emergency operation for posterior spinal decompression and fusion with instrumentation (Fig. 3). Fifteen months postoperatively, he could walk without any assistance and returned to work.
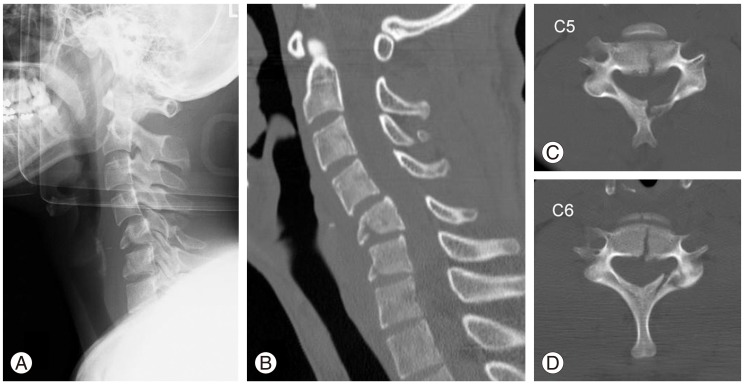
Case 1: preoperative X-ray (A) and computed tomography (B-D) of the cervical spine. C5 and C6 had burst fracture and developed kyphotic deformity.
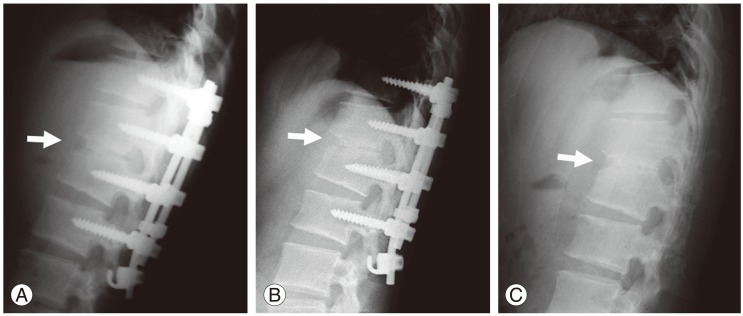
2) Case 2
A 26-year-old man had complete paralysis in both legs (Frankel type A) after a jumping failure while snowboarding. The results of X-ray and magnetic resonance imaging scan showed distractive-flexion between Th11 and Th12 (Fig. 4). On the same day as the injury, the patient received intravenous administration of methylprednisolone, and emergency operation for posterior spinal reposition and fusion with instrumentation. After 2 months, he underwent anterior decompression and fusion. The posterior implants were removed when bone union was achieved (Fig. 5). Paralysis recovered to Frankel type D.
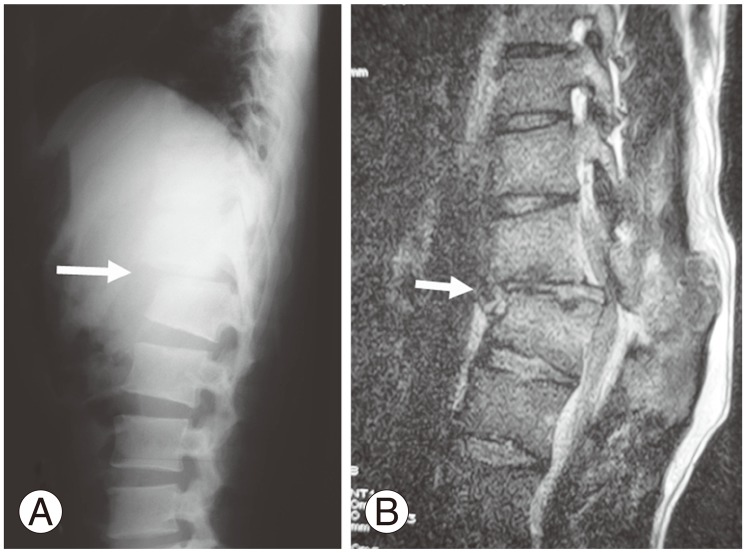
Case 2: preoperative X-ray (A) and magnetic resonance imaging (B) of thoracolumbar junction. The spine developed kyphotic deformity.
Discussion
This is the first report regarding the clinical course of paralysis related to snowboarding and their ADL. Importantly, all injured snowboarders included in the present study stated that they no longer participated in snowboarding or any other sports activity since their injuries. As physically handicapped individuals can still participate in many types of sport, these results clearly illustrated the severe physical and psychological impact of spinal and spinal cord injuries on snowboarders.
1. Characteristics of snowboarders who sustain spinal injuries
Wakahara et al. [8] reported that most injured snowboarders were young men, with thoracolumbar junction injury caused by jumping, and over half of the patients showed severe paralysis classified as Frankel type A or B. Siu et al. [11] suggested that young male snowboarders have an elevated risk of neck and head injury. Seino et al. [12] suggested that the predominance of male patients may reflect the aggressive and reckless snowboarding behavior of young men. Chow et al. [13] also documented the close association between the performance of aerial maneuvers by snowboarders and the propensity to injure the head, abdomen, and spine. In the present study, the characteristics of patients were compatible with those described in previous reports. In all injuries related to snowboarding, 4.7% were vertebral injuries and 0.3% were spinal cord injuries [14]. These proportions were 4 times higher than those related to skiing [14]. The major fracture pattern in snowboarding is fracture-dislocation, which requires high energy, and tends to accompany severe spinal cord injury [8,12]. In the present study, the same characteristics were obtained.
2. Operative intervention
There is no consensus in the literature regarding the timing of surgery for spinal cord injurys. Cengiz et al. [15] reported significantly better recovery when paralysis was incomplete and decompression was performed within 8 hours. Furlan et al. [16] suggested early surgical intervention was safe and feasible and could improve clinical and neurological outcomes and reduce health care costs. In contrast, McKinley et al. [17] suggested early spinal surgery (<72 hours after injury) reduces pulmonary complications. However, there were no differences in neurological or functional improvements between the early and late surgical groups. We performed spinal operations as soon as possible to promote early rehabilitation and reduce the risk of secondary complications. In terms of neurological improvement, urgent operations may not have played a significant role in amelioration of severe paralysis, but it was presumed that they at least helped to reduce the risk of complications [17].
3. Neurological outcomes of surgically treated snowboarders who sustained spinal injuries
Among the patients included in the present study, those with complete paralysis classified into Frankel type A tended not to recover at all, similar to cases reported previously [15]. Fisher's exact probability test confirmed that the patients in the complete group showed a significantly higher rate of requiring a wheelchair compared to those in the incomplete group (Table 3). The recovery rates of the patients with some paralysis were different between the Complete and incomplete groups, while it seemed that final recoveries were focused to Frankel type A and D (total in both, 84.2%). Improvement of paralysis was observed in only 2 of 8 patients (25.0%) in the complete group, but in 7 of 9 patients (77.8%) in the incomplete group. This difference was significant, and the prognosis with regard to paralysis was markedly different between the two groups. Except in cases of complete paralysis, there was a good likelihood of regaining ambulatory capacity in the incomplete group.
4. Performance in daily activities and sports in surgically treated snowboarders who sustained spinal injuries
As the patients in this study could be characterized as young adults who have to work for a living and who had actively participated in sports, this study focused on their postoperative activities in both working and sporting activities. There was no significant difference in the ratio of patients who could return to work between the Complete and incomplete groups (Fig. 3). Furthermore, none of the subjects included in the present study participated in any sports activities, including snowboarding, after the spinal operations. We speculate that they were traumatized psychologically as well as physically. There were no significant differences in the rates of returning to driving, playing sports, and snowboarding between the Complete and incomplete groups. Thus, the results of the present study indicate that participation in work and sports activities, including snowboarding, do not depend on the degree of primary paralysis or neurological improvement, but on the degree of psychological trauma.
5. Limitations of the present study
There were some limitations in this study. First, we assessed only patients that had undergone surgery. Combined or comparative analyses in patients with snowboarding-related spinal or spinal cord injury who were treated conservatively may provide additional data. Second, most snowboarders are young adults. Therefore, further evaluation of marriage status, sexual life, and mental condition would also provide relevant data. Third, the number of patients included in this study was small. Further studies in larger numbers of cases will be useful to evaluate the effects of surgical intervention on paralysis.
Conclusions
We performed operations in 19 patients with unstable spinal injuries due to snowboarding. Although most of the patients who initially had paralysis still had some paralysis at the average of 4-year follow-up, 79% of the patients returned to work. However, these spinal injuries markedly influenced their social and sports activities. It will be necessary to enhance promotion of injury prevention emphasizing the snowboarders' responsibility code.
Notes
No potential conflict of interest relevant to this article was reported.