Prognostic Value of Preoperative Coping Strategies for Pain in Patients with Residual Neuropathic Pain after Laminoplasty for Compressive Cervical Myelopathy
Article information
Abstract
Study Design
Single-center retrospective cohort study.
Purpose
To clarify the prognostic value of preoperative coping strategies for pain due to compressive cervical myelopathy.
Overview of Literature
Preoperative physical function, imaging and electrophysiological findings are known predictors of surgical outcomes. However, coping strategies for pain have not been considered.
Methods
Postoperative questionnaires, concerning health-related quality of life (HRQOL) and daily living activities, were sent to 78 patients with compressive cervical myelopathy who had suffered from neuropathic pain before laminoplasty, and been preoperatively assessed with respect to their physical and mental status and coping strategies for pain. Hierarchical multiple regression analysis was performed to clarify the extent to which the patient's preoperative coping strategies could explain the variance in postoperative HRQOL and activity levels.
Results
Forty-two patients with residual neuropathic pain after laminoplasty were analyzed by questionnaires (28 men, 14 women; mean age, 62.7±10.2 years; symptom duration, 48.0±66.0 months). The valid response rate was 53.8%. Hierarchical multiple regression analysis showed that preoperative coping strategies, which involved coping self-statements, diverting attention, and catastrophizing, were independently associated with postoperative HRQOL and activity level, and could explain 7% to 11% of their variance. Combinations of the coping strategies for pain and upper/lower motor functions could explain 26% to 36% of the variance in postoperative HRQOL and activity level.
Conclusions
Preoperative coping strategies for pain are good predictors of postoperative HRQOL and activities of daily living in patients with postoperative residual neuropathic pain due to compressive cervical myelopathy.
Introduction
Neuropathic pain not only restricts the activities of daily living and work, but also causes deterioration in health-related quality of life (HRQOL) [1,2]. Many patients who have undergone laminoplasty for compressive cervical myelopathy experience residual neuropathic pain. Therefore, a means of effectively managing persistent neuropathic pain in patients with compressive cervical myelopathy is needed. Such a management technique would not only help to identify the presence of cross-sectional relationships between neuropathic pain and HRQOL at a given time point, but also enable prediction of the outcomes of laminoplasty using the preoperative status for early pain interventions in patients with compressive cervical myelopathy. Previous studies have reported that preoperative physical functioning [34], imaging findings [3567], and electrophysiological findings [78] are associated with surgical outcomes in patients with compressive cervical myelopathy. When considering the tran-sactional model of stress [9], it can be hypothesized that coping strategies may also be useful to predict surgical outcomes. However, the prognostic value of coping strategies for pain is unknown. Additionally, coping strategies are defined as "cognitive" and "behavioral" efforts to manage specific external and/or internal demands (e.g., pain) [9] and are crosssectionally associated with pain and HRQOL [1011]. For example, catastrophizing is a cognitive coping strategy characterized by a tendency to misinterpret and exaggerate situations that may be threatening [12]. Conversely, pain behavior is a behavioral coping strategy and involves activities such as doctor shopping and drug abuse.
The present study aimed to clarify the prognostic value of preoperative pain-coping strategies for postoperative outcomes in patients with postoperative residual neuropathic pain due to compressive cervical myelopathy. To accomplish this goal, we inspected the associations between preoperative factors (including coping strategies for pain) and postoperative HRQOL and activities of daily living for at least one year postoperatively.
Materials and Methods
1. Study design
This retrospective cohort study was conducted in September 2014 at a spine care center in a general hospital in Japan. The study was performed after gaining approval from the ethics committee of the Takasaki University of Health and Welfare.
2. Participants
A questionnaire with an explanatory leaflet of the present study and a consent form for participation were mailed to patients who had undergone compression cervical myelopathy due to spondylosis and/or ossification of the posterior longitudinal ligament, both of which were diagnosed based on neurological and radiological findings. The treatment period was from September 2011 to September 2013, and only those patients were included whose complete preoperative assessment data were available. The exclusion criteria were absence of neuropathic pain before laminoplasty, and pain that was derived from factors other than cervical myelopathy, such as peripheral circulatory disturbances, musculoskeletal disorders, or neurological disorders.
We required the registration of each responder's name in a questionnaire to coordinate the obtained data with the preoperative data. The patients were also required to return a written, signed consent form with the completed questionnaire.
3. Assessment items
1) Postoperative survey
The postoperative questionnaire mainly comprised the medical outcomes study short form 8-item health survey (SF-8) and life-space assessment survey.
The SF-8, the reliability and validity of which has been confirmed [13], was used to assess HRQOL. The SF-8 comprises the following eight domains: general health (GH), physical functioning (PF), role physical (RP), bodily pain (BP), vitality (VT), social functioning (SF), mental health (MH), and role emotional (RE). The physical component summary (PCS) and mental component summary (MCS) are calculated using the following formula:
PCS= 0.23024 (GH)+0.40674 (PF)+0.38317 (RP)+0.33295 (BP)+0.07537 (VT)-0.01275 (SF)-0.30469 (MH)-0.14803 (RE)+0.67371;
MCS= 0.0202 (GH)-0.19972 (PH)-0.16579 (RP)-0.15992 (BP)+0.16737 (VT)+0.27264 (SF)+0.57583 (MH)+0.42927 (RE)+4.34744.
Higher scores of the eight domains, as well as of the PCS and MCS, indicates a better health status of the subject.
The life-space assessment survey, the reliability and validity of which has also been shown [14], was used to assess activities in daily living. The frequency and independence of activities in each of the following five life-space levels were determined in the questionnaire: rooms except a bedroom, outside home, neighborhood, town, and beyond town. Points assigned were between 1-5 to each of the five above-mentioned life-space levels. Grading of points, as the frequency scores. For frequency scores, 1-4 points were given for <1 time/week, 1-3 time(s)/week, 4-6 times/week, and every day, respectively. For independence scores, 1.0, 1.5, and 2.0 points were given for personal assistance needed, equipment only, and no assistance, respectively. The life-space index (LSI) was obtained with the following formula: the first life-space score of rooms except a bedroom (1)×frequency score (1-4) at the first life-space×assistance score (1-2) at the first lifespace+…+the fifth life-space score of beyond town (2)×frequency score (1-4) at the fifth life-space×assistance score (1-2) at the fifth life-space (total range, 0-120 points). A higher score indicates greater level of activities of daily living. Conversely, 0 point indicated that a person lived only in his/her bedroom.
2) Preoperative survey
Pain intensity, physical functioning, psychological state, and coping strategies for pain were assessed before surgery. An 11-point numerical rating scale (NRS) was used (0, no pain; 10, unbearable pain). Patients were asked about their maximum intensity of pain during daily living.
The Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) [15], which was developed through scientific procedures [16], was used to assess physical functioning. The JOACMEQ is classified into the following five subcategories: cervical spine function, motor function of the upper extremities, motor function of the lower extremities, bladder function, and quality of life. Each subcategory score was calculated by an established formulae (range, 0-100 points; 0, patients felt severe dysfunction or poor health). Scores of all subscales except quality of life were calculated in the present study.
The hospital anxiety and depression scale (HADS) [17], the reliability and validity of which has been shown [18], was used to assess the degree of anxiety and depression. The HADS is divided into anxiety and depression subscales, and each comprises seven questions (range, 0-21 points). A higher score for these subscales indicates a greater degree of anxiety or depression.
The Japanese short version of the Coping Strategies Questionnaire (CSQ-J) was also used [19]. The CSQ-J is based on the original CSQ [20]. Both the CSQ-J and the original CSQ assess six cognitive strategies (praying or hoping, catastrophizing, coping self-statements, diverting attention, reinterpreting pain sensations, and ignoring pain sensations) and two behavioral strategies (increasing pain behavior and increasing activity level). These subscales were graded on a 7-point Likert scale (0, never do; 6, always do that when in pain) for the coping strategies subscales. The CSQ-J contains two questions for each cognitive and behavioral strategy; therefore, the scores of each coping strategy range from 0 to 12 points.
4. Analytic procedure
Fundamental statistics of the assessed items were calculated. Pearson product-moment correlation coefficients (r) were determined between postoperative factors (PCS, MCS, and LSI) and preoperative factors (NRS pain score and subscale scores of the JOACMEQ, HADS, and CSQ-J). Values of r<0.1, 0.1≤r<0.3, 0.3≤r<0.5, and r≤0.5 were considered to be insubstantial, small, moderate, and large correlations, respectively, based on Cohen [21] criteria. Hierarchical multiple regression analysis was then performed. Postoperative factors were used as dependent variables, and the preoperative factors that were significantly correlated with postoperative factors in previous univariate analyses were used as independent variables. Changes in the R2 and F-values were calculated by addition of the CSQ-J as a second block of independent variables to the NRS, JOACMEQ, and HADS as a first block of independent variables. The number of independent variables used was circumscribed within one-tenth of the number of analyzed participants to obtain reliable multivariate regression models. Half of the independent variables used were allocated to the first block, and the remaining variables were allocated to the second block. Preoperative factors for which Pearson product-moment correlation coefficients with postoperative factors were higher than others were preferentially selected as independent variables. The multicollinearity among independent variables was confirmed using variance inflation factors.
All statistical analyses were performed using SPSS ver. 21 (IBM Japan, Tokyo, Japan). Values of p<0.05 were considered to be statistically significant.
Results
1. Responders
Complete responses were received from 59 of the 78 patients to whom the questionnaires were sent (response rate, 74.7%). Seventeen patients were excluded because eight had no preoperative neuropathic pain at the postoperative follow-up survey; eight had undergone treatments for knee osteoarthritis/injury, low back pain, deep vein thrombosis, rectal cancer, or amyotrophic lateral sclerosis; and one lost her husband within the previous month. Therefore, 42 patients with residual neuropathic pain after laminoplasty were analyzed (28 men, 14 women; mean age, 62.7±10.2 year; symptom duration, 48.0±66.0 months [range, 3-360 months]). The valid response rate was 53.8%. The average number of days after surgery was 793.5±220.7 days (range, 391-1,171 days). With the exception of the symptom duration, the demographic characteristics of the excluded patients (11 men, 6 women; mean age, 60.0±12.2 years [range, 30-75 years]; symptom duration, 33.7±39.2 months [range, 4-124 months]) were not different from those of the analyzed patients.
The results of the preoperative assessment are shown in Table 1. The postoperative PCS, MCS, and LSI at the postoperative follow-up survey were 40.8±7.8 (range, 18.3-53.7), 48.6±8.0 (range, 31.2-64.4), and 90.8±26.4 (range, 35.5-120.0), respectively.
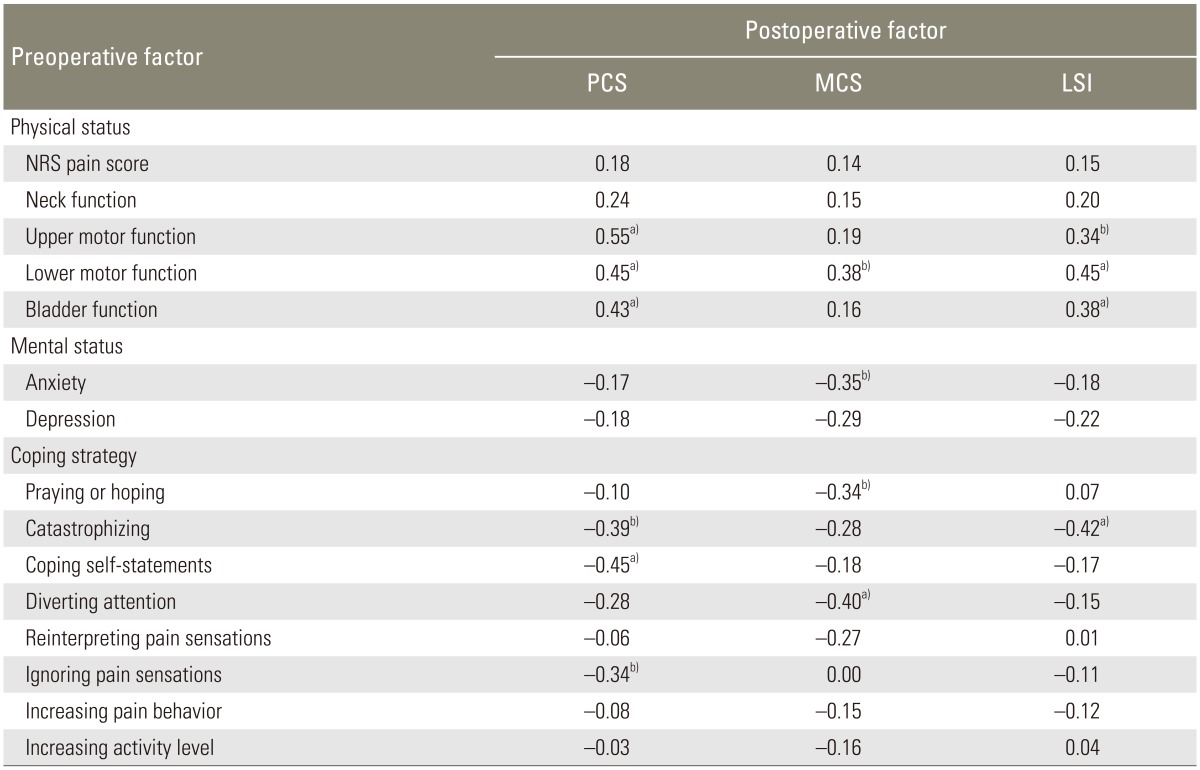
2. Correlation between postoperative and preoperative factors
Table 2 shows Pearson product-moment correlation coefficients between the postoperative PCS, MCS, and LSI, and the preoperative NRS for pain intensity, JOACMEQ, HADS, and CSQ-J.
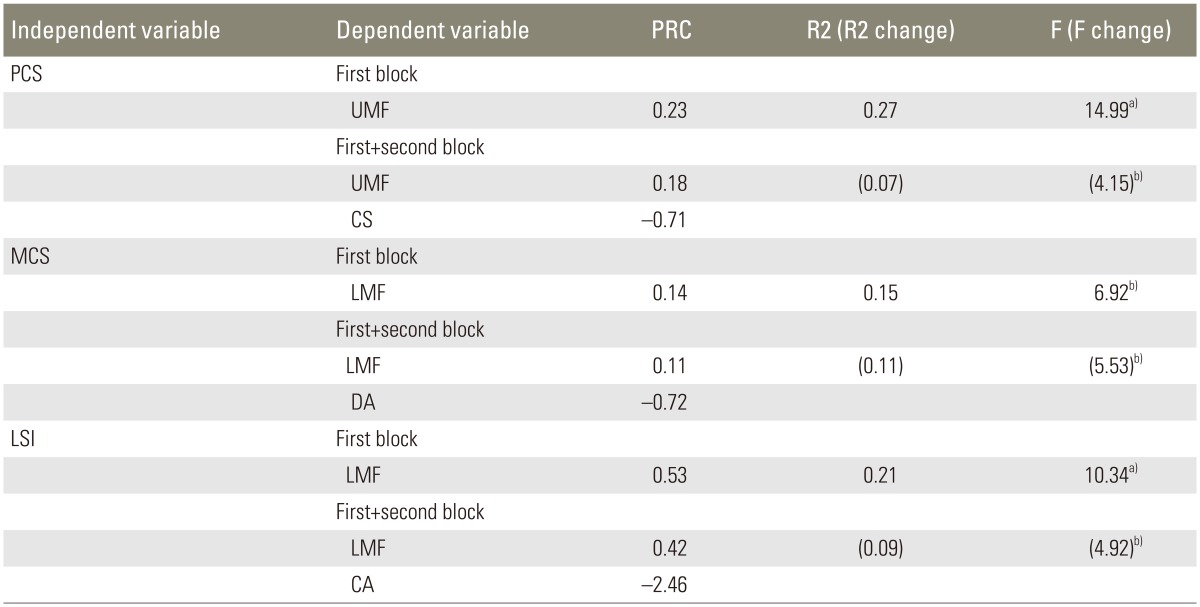
A maximum of two independent variables could be used in each block of the hierarchical multiple regression analysis because the number of analyzed respondents was 42; therefore, the preoperative motor functions of the upper and lower extremity subcategories of the JOACMEQ were used as independent variables of the first block, and the catastrophizing and coping self-statement subcategories of the CSQ-J were used as independent variables of the second block, when using the postoperative PCS as a dependent variable. Additionally, the preoperative motor function of the lower extremity subcategory of the JOACMEQ, the anxiety subcategory of the HADS, and the praying/hoping and diverting attention subcategories of the CSQ were used as independent variables of each block in the case of the postoperative MCS, and the preoperative motor function of the lower extremity and bladder function subcategories of the JOACMEQ were used in the case of the postoperative LSI. The results of the hierarchical multiple regression analysis are summarized in Table 3. The variance inflation factors of the independent variables used ranged from 1.05 to 1.19.
Discussion
The results of the present study can be summarized as follows: (1) the valid response rate of the follow-up mailing questionnaire was 53.8%; (2) not only the preoperative physical and mental status, but also the coping strategies were at least moderately correlated with the postoperative PCS, MCS, and LSI; (3) preoperative coping strategies, which involved coping self-statements (i.e., encouraging oneself or persuading oneself that there is no risk), diverting attention (i.e., paying attention not to pain, but instead to an activity or thought), and catastrophizing (i.e., comprehending pain extremely pessimistically), could independently explain the postoperative PCS, MCS, and LSI, respectively (from 7% to 11%).
1. Characteristics of responders
More than three-fourths of the patients (59 of 78 patients) responded to our postoperative questionnaire, and most of them (42 of 59 patients) were analyzed (valid response rate, 53.8%). With the exception of symptom duration, the characteristics of the excluded responders did not differ from those of the analyzed responders. Moreover, the severity of cervical myelopathy among the analyzed responders was at most moderate because the scores of the JOACMEQ subcategories were high. Therefore, we believe that our sample represented patients with compressive cervical myelopathy who underwent surgery before aggravation of myelopathy, and had postoperative residual neuropathic pain.
The postoperative PCS and MCS of our patients with residual neuropathic pain due to compressive cervical myelopathy were still lower than the national standard values (50 points). Many patients with residual neuropathic pain following compressive cervical myelopathy had frequently gone out on their own despite low physical and mental health perceptions.
2. Preoperative predictors of postoperative HRQOL and level of activity
In the univariate correlation analysis, the postoperative physical health perception and activities of daily living were only associated with the preoperative physical status, whereas mental health perception was associated with both the physical and anxiety status. However, the anxiety subcategory was not selected as an independent variable in the multiple regression analysis when the MCS was used as a dependent variable. Although the mental status is closely related to HRQOL [122], preoperative anxiety cannot accurately predict a patient's postoperative mental health perception. Additionally, the preoperative pain intensity cannot predict the postoperative physical health perception and level of activity. These findings may indicate that pain intensity and anxiety are likely to change synchronously after surgical treatment in patients with compressive cervical myelopathy, as has been confirmed in patients with chronic low back pain [23]. This is also why the predictive power for future HRQOL and level of activity was poor.
The preoperative coping self-statements, diverting attention, and catastrophizing subcategories were associated (independently of the upper and lower motor function subcategories) with the postoperative PCS, MCS, and LSI, respectively, and could explain 7% to 11% of their variance, in addition to the motor function subcategories. Only two preoperative factors, motor function and coping strategies for pain, could explain 26% to 36% of the variance in the postoperative physical and mental health perceptions and activities of daily living. However, HRQOL and activity level were influenced by many factors, including both personal factors (e.g., values and beliefs) and environmental factors (e.g., human relationships and living environments).
Catastrophizing is a known predictor of surgical improvement of pain intensity in patients with spinal cord injury [24] and postsurgical pain intensity after total knee arthroplasty or breast surgery [25]. Preoperative catastrophizing, coping self-statements, and diverting attention were good predictors of postoperative HRQOL and daily living activities in patients with postoperative residual neuropathic pain due to compressive cervical myelopathy. These coping strategies for pain, including catastrophizing, were cognitive immanent acts based on pain-induced suffering because of the negative relationship among the three coping strategies, physical and mental health perceptions, and activity level. Therefore, we should pay attention not only to the physical and mental functions, but also to coping strategies before surgery in pain ridden patients with compressive cervical myelopathy.
3. Study limitations and future prospects
There are two major limitations in the present study. First, our sample size was small, and the study was retrospectively conducted in a single center. Therefore, supplementary examinations using other samples and settings are needed to generalize the present findings. Second, preoperative coping self-statements, diverting attention, and catastrophizing were negative predictors of postoperative outcomes in our cohort. Although coping strategies for stressors do not always have a specific effect on all persons, they do have bidirectional effects according to the context. For example, passive and avoidance coping strategies to escape stressful situations without solving the underlying problems are risk factors for postsurgical outcomes [2627]. However, when persons constructively use the same coping strategy to extend the time available to solve problems, the coping strategy may eventually generate an effect of decreasing stress reactions or lead to fair treatment outcomes. The cognitive process involved in the selection of coping strategies for pain should be clarified to more deeply understand the associations between preoperative coping strategies and postoperative outcomes.
Conclusions
We investigated the relationships between the preoperative physical and mental status and coping strategies for pain, and the postoperative HRQOL and activities of daily living in 42 patients with residual neuropathic pain after laminoplasty for compressive cervical myelopathy. We found that preoperative coping strategies for pain, coping self-statements, diverting attention, and catastrophizing, independently predicted postoperative HRQOL and activity level. Combinations of coping strategies for pain and upper/lower motor functions could explain 26% to 36% of the variance of postoperative HRQOL and activity level. We should pay attention not only to physical and mental functions, but also to coping strategies before surgery in pain ridden patients with compressive cervical myelopathy.
Acknowledgments
The author is grateful to Nodoka Manabe, a medical doctor at Harunaso Hospital, for kindly providing support in the present study.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.