|
 |
- Search
| Asian Spine J > Volume 9(3); 2015 > Article |
Abstract
Purpose
To assess the accuracy of detecting lateral mass and facet joint injuries of the subaxial cervical spine on plain radiographs using computed tomography (CT) scan images as a reference standard; and the integrity of morphological landmarks of the lateral mass and facet joints of the subaxial cervical spine.
Overview of Literature
Injuries of lateral mass and facet joints potentially lead to an unstable subaxial cervical spine and concomitant neurological sequelae. However, no study has evaluated the accuracy of detecting specific facet joint injuries.
Methods
Eight spinal surgeons scored four sets of the same, randomly re-ordered, 30 cases with and without facet joint injuries of the subaxial cervical spine. Two surveys included conventional plain radiographs series (test) and another two surveys included CT scan images (reference). Facet joint injury characteristics were assessed for accuracy and reliability. Raw agreement, Fleiss kappa, Cohen's kappa and intraclass correlation coefficient statistics were used for reliability analysis. Majority rules were used for accuracy analysis.
Results
Of the 21 facet joint injuries discerned on CT scan images, 10 were detected in both plain radiograph surveys (sensitivity, 0.48; 95% confidence interval [CI], 0.26-0.70). There were no false positive facet joint injuries in either of the first two X-ray surveys (specificity, 1.0; 95% CI, 0.63-1.0). Five of the 11 cases with missed injuries had an injury below the lowest visible articulating level on radiographs. CT scan images resulted in superior inter- and intra-rater agreement values for assessing morphologic injury characteristics of facet joint injuries.
Although the proportion of cervical spine injuries in the adult major trauma population is relatively small (3.5%) [1], missed diagnosis of such an injury could result in serious disability [2]. Routine computed tomography (CT) scans of the spine in the diagnostic work-up of trauma patients is implemented in approximately 80% of level I trauma centers in order to reduce the number of missed injuries [34]. However, a recent report demonstrated that clinicians continue to use radiographs of the cervical spine in low-risk adult trauma patients [5].
The lateral masses, superior and inferior articular processes of the subaxial cervical spine form the central pillars of anteroposterior (transverse) and rotational stability [6]. Injuries of these structures potentially lead to an unstable subaxial cervical spine and concomitant neurological sequelae. While several reports on the accuracy of detecting general cervical spine injuries on plain radiographs and CT scans have been published [789], no study has evaluated the accuracy of detecting specific facet joint injuries.
Moreover, no spinal injury classification including specific morphological characteristics of the cervical spinal facet joints and lateral masses has yet been accepted and endorsed worldwide. In 2007, Dvorak et al. [10] grouped 90 unilateral facet joint injuries into 9 morphological categories. Subsequently in 2009, Lee and Sung [6] proposed a categorization of lateral mass and facet joint fractures into 6 groups. Both studies, however, did not include bilateral facet joint injuries nor did they present agreement data.
The aim of the current study was twofold. First, we assessed the accuracy of detecting facet joint and lateral mass injuries of the subaxial cervical spine on plain radiographs using CT as a reference standard. Secondly, we assessed the agreement on judging morphological landmarks of the facet joints and lateral masses of the subaxial cervical spine. We conducted a radiologic imaging measurement study for this purpose.
Eight spinal surgeons attended a 1-day meeting to score 4 sets of randomly ordered cases with and without facet joint injuries of the cervical spine. The study was divided into 4 surveys: surveys 1 and 2 were a test and re-test of the same set of 30 randomly (re-)ordered series of conventional (i.e., anteroposterior and lateral) radiographic measurements; surveys 3 and 4 were a test and re-test of the same set of 30 randomly (re-)ordered series of CT scan images. Before the start of survey 1, a study outline describing the rationale and the definitions of the measurements to be made throughout the day was presented. Also, 2 training cases were completed under the guidance of the senior authors (JJvM, BG).
Cases were selected from a database comprising a consecutive series of high-energy blunt trauma patients admitted to a Dutch level 1 trauma centre serving a population of over 2.0 million inhabitants [11]. In this study, all admitted high-energy blunt trauma patients older than 15 years were included and underwent routine CT imaging of the cervical spine, thorax and abdomen after clinical evaluation and conventional radiographic work-up.
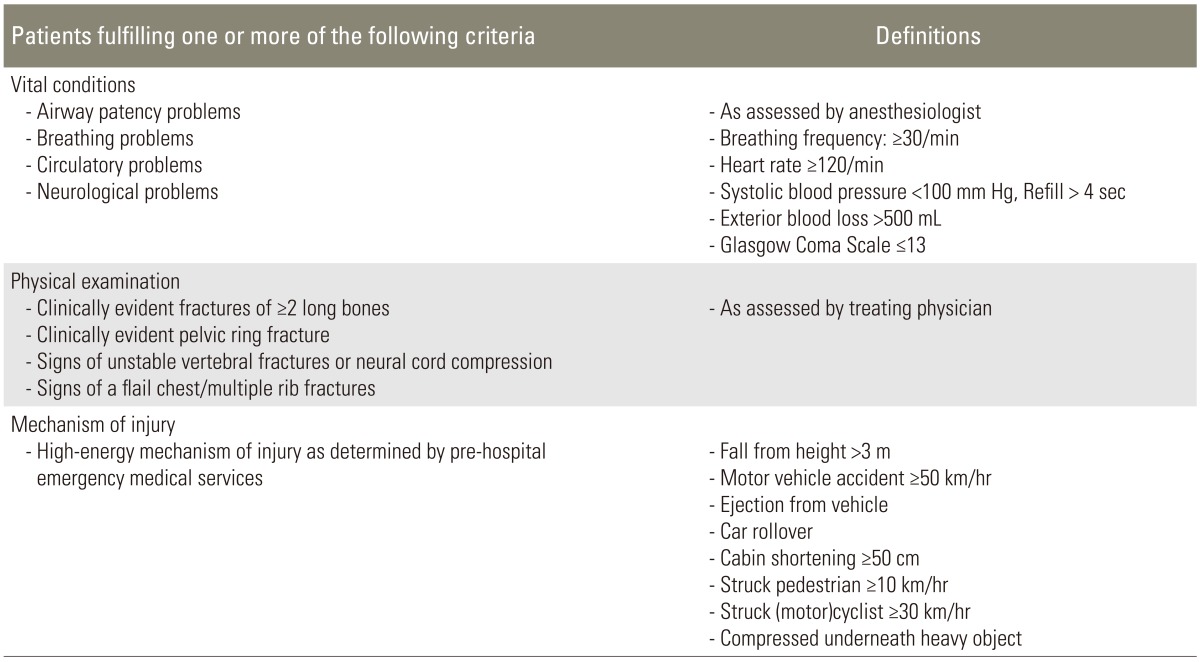
Included patients were those suffering from life-threatening vital conditions, showing signs of severe injuries during physical examination and/or involved in high-energy injury mechanisms as presented in Table 1. Patients were excluded from the protocol in case of (1) class 3 or 4 shock requiring immediate surgical intervention; (2) suspected or known pregnancy; and (3) neurological condition or deterioration requiring immediate cerebral CT evaluation without any diagnostic delay.
Routine CT protocol was conducted with a Somatom Sensation 16-slice multi-detector CT scanner with automated tube current modulation (Siemens Medical Systems, Erlangen, Germany). CT scans were executed at a tube potential of 120 kV, with a reference value of effective tube current time product of 200 mAs. The detector configuration was 16├Ś1.5 mm. Reconstructed section thickness was 3 mm for bone reconstruction kernel, with an increment of 1.5 mm. Sagittal and coronal reformatted images of the spine were also presented to the raters.
Radiological registrars evaluated all radiological examinations, documented, and entered them into the database under supervision of a trauma-dedicated radiologist. Patients with a subaxial cervical spine injury were retrieved from the database by 1 of the authors (JJvM). Along with the radiology reports, all cases were re-evaluated and categorized as having 'clinically insignificant' or 'clinically significant' injuries. Subaxial cervical spine injuries were considered 'clinically insignificant' if the injuries were isolated and involved Ōēź1 transverse process(es) (without involvement of the facet joint), spinous process(es) (without involvement of the lamina) or osteophytes. After exclusion of the cases with 'clinically insignificant' injuries, all remaining cases were arbitrarily assigned numbers. Subsequently, 30 cases were randomly selected using an online random integer sequence generator (www.random.org/integers). As a preferred ratio of 2 out of 3 cases with a facet joint injury was not met, 5 random cases without facet joint injury were replaced by 5 manually selected cases with facet joint injury. This resulted in a final cohort of 30 cases with significant subaxial cervical spine injury, of which 21 cases had a facet joint injury and 9 cases had none. The final cohort was arbitrarily re-assigned new numbers and an online random integer set generator (www.random.org/integer-set) was used to generate 4 sets of randomly ordered cases: 2 for the conventional radiography examination (survey 1 & 2) and 2 for the CT evaluation (survey 3 & 4).
Eight raters participated in the study. Four raters were fellowship-trained spine surgeons involved in the management of cervical spine injuries and the remaining 4 raters were orthopedic surgeons who were participating in a spinal surgery fellowship at the time of the study. Each rater was presented the same 4 sets of the randomly ordered cases. The raters were blinded to all other clinical information and none of the raters had any previous clinical information on the cases presented. All cases were scored individually and independently from other raters.
De-identified images were analyzed using ClearCanvas Workstation V2.0 (Toronto, Canada). The following measurements were made:
Before discerning the presence of an injury, raters were asked to report the most caudal spinal level visible on the lateral radiograph. Each level was documented as an articulating level, ranging from C2-C3 to C7-T1 (C, cervical; T, thoracic).
Raters were asked whether a facet joint injury of the subaxial spine was present or absent. If an injury was detected, the following injury characteristics were measured and reported.
Each level was documented as an articulating level, ranging from C2-C3 to C7-T1. In cases where Ōēź1 articulating level was affected, the rater was asked to report both the most severely affected level, as well as the other levels of injury.
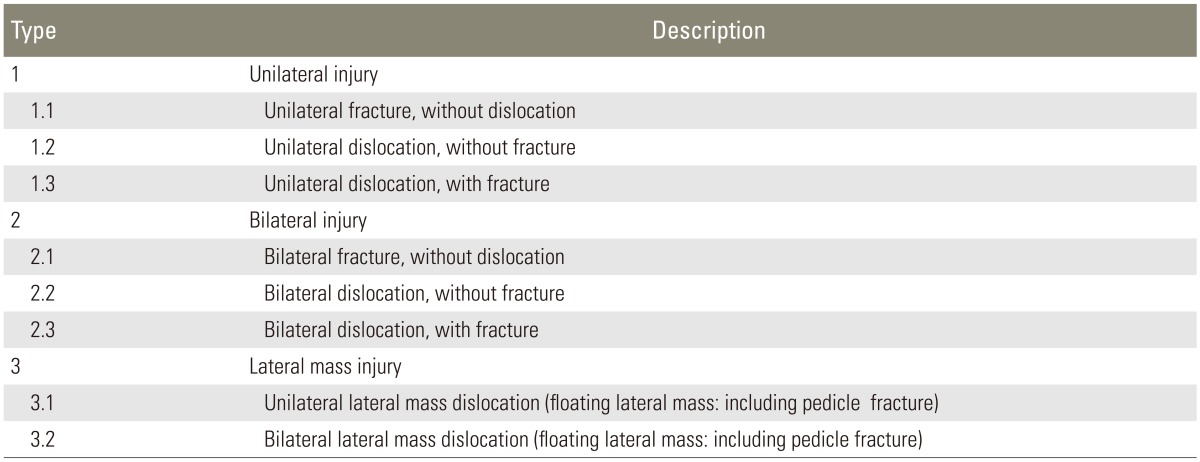
Since there is no widely accepted, endorsed classification of subaxial cervical spinal injuries including specific morphological characteristics of the facet joints and lateral masses, raters categorized each articulating level of injury according to the injury characteristics listed in Table 2. This morphological categorization was created in line with the spinal injury classification principles outlined in a recent paper [12]. Only 1 injury characteristic could be assigned to each level. When Ōēź1 characteristic was possible, the most severe (i.e., highest number) was documented.
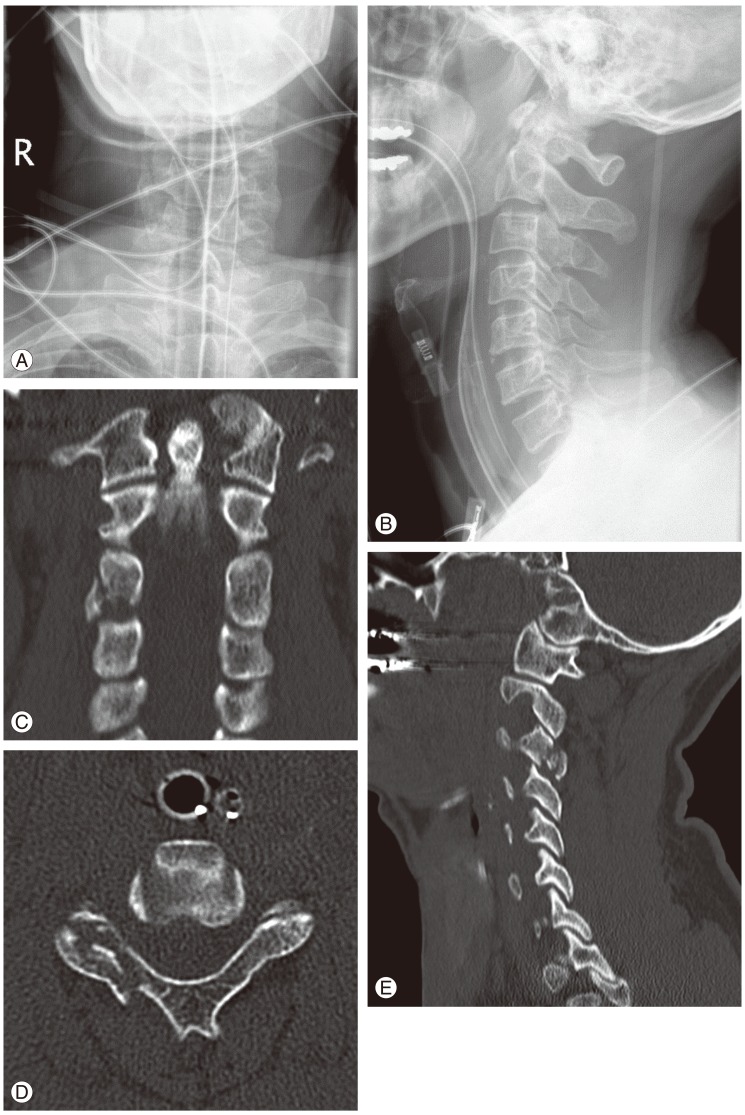
Vertebral body translation was measured for each articulating level of injury. The measurement technique reported by Bono et al. [13] was used for this purpose (Fig. 1). From a lateral perspective, a posterior tangent line is drawn along the injured and caudal vertebral bodies. The distance between these lines is measured at the level of the inferior aspect of the upper vertebra. Bono et al. [13] reported that when this measurement is made on sagittal CT images, the degree of translation might vary from the left to the right side. Therefore, it is recommended to record the maximal measured translation, since this best reflects the severity of the injury.
Accuracy is the degree to which the measurement actually represents what is intended. The accuracy of a test is best assessed by comparison to a reference standard technique that is accurately representative, when possible. We considered conventional radiographs as the 'test' and CT images as the reference standard. However, since a gold reference standard was missing, the most likely distribution of true imaging outcomes in the sample was estimated using different majority rules (>50%, >75%, and 100%).
Precision, or reliability, is the extent to which repeated measurements of the same case under similar conditions agree with each other. Observer variation is the most frequently assessed type of reliability and can be divided into 2 components: inter-rater reliability and intra-rater reliability. Inter-rater reliability assesses the reliability, or agreement, of identifying a facet joint or lateral mass injury when measured by different people under similar conditions. Intra-rater reliability assesses the reliability, or reproducibility, of injury identification when measured more than once by the same rater.
The inter-rater reliability of nominal and dichotomous variables was estimated using Fleiss Kappa [14]. The Fleiss Kappa is a multi-rater reliability statistic that is analogous to Cohen's Kappa that is applicable to 2 raters only. The intra-rater reliability for nominal and dichotomous variables was estimated as a Cohen's Kappa for the test/re-test pair for each observer. Kappa values range from -1.0 to 1.0, with negative values indicating disagreement and a positive value of 1.0 representing perfect agreement. A 0 value represents no agreement beyond what would be expected by chance. Fleiss [15] proposed the following categories for strength of agreement for the kappa coefficient: Ōēż0.4=poor, 0.4-0.75=fair to good, and Ōēź0.75-1=excellent agreement. Although this categorization is commonly applied, no consensus exists as to what constitutes an acceptable kappa coefficient [16]. The intraclass correlation coefficient was used to estimate correlation between all raters for the scale data. Pair-wise agreement coefficients were pooled using random effects model with a 95% confidence interval (Cl).
Injury specific measurements could only be calculated for those cases that had 100% agreement on the presence of a facet joint injury. All statistical analyses were considered significant when alpha was <0.05. Data analyses were performed using the SPSS ver. 16.0 (SPSS, Chicago, IL, USA) and MetaXL ver. 1.3 available from www.epigear.com.
Thirty cases were scored of which 21 had a facet joint injury and 9 did not. There were 21 male patients and 9 female patients. The mean patient age at the time of injury was 47 years (range, 17 to 93 years).
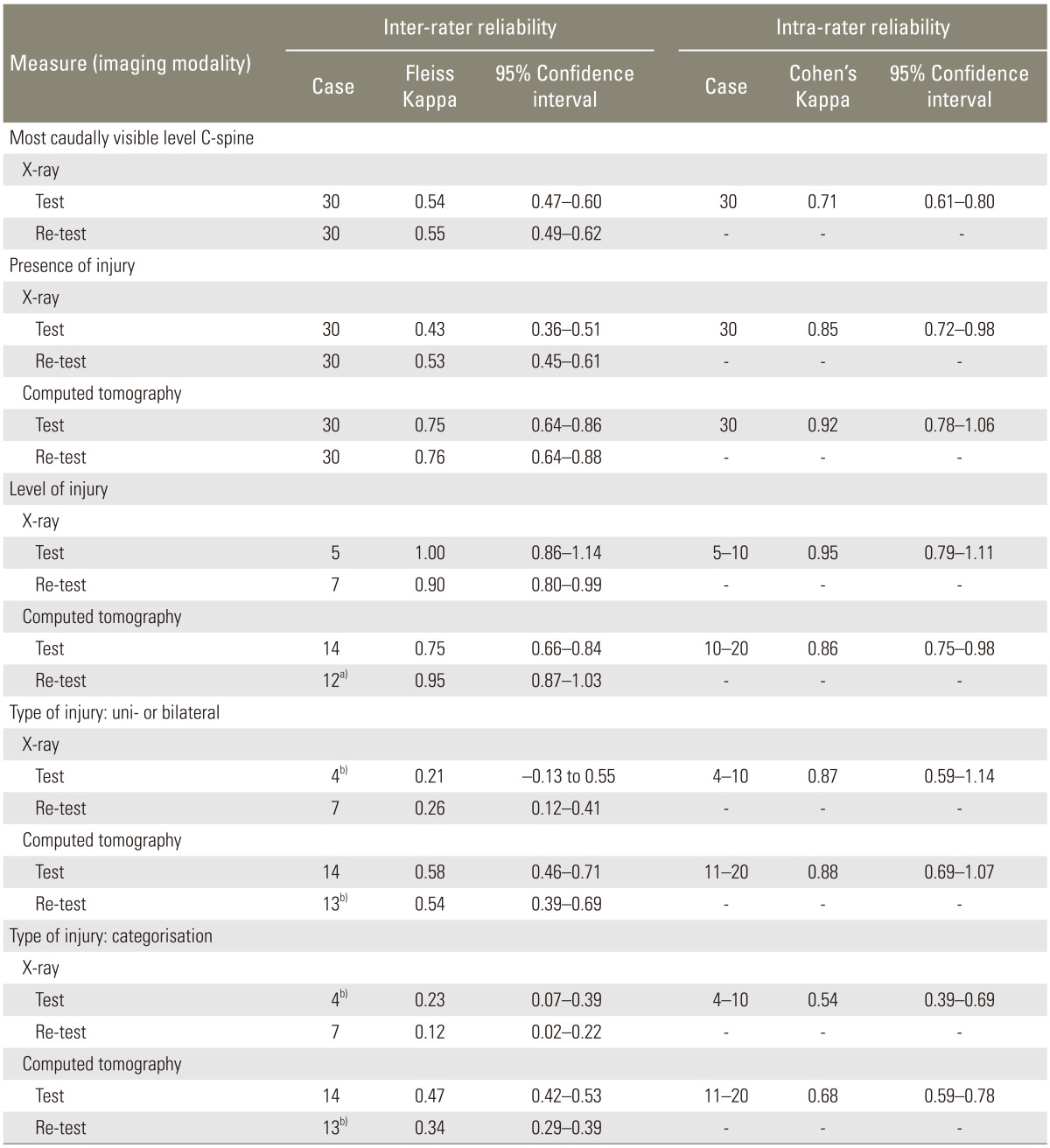
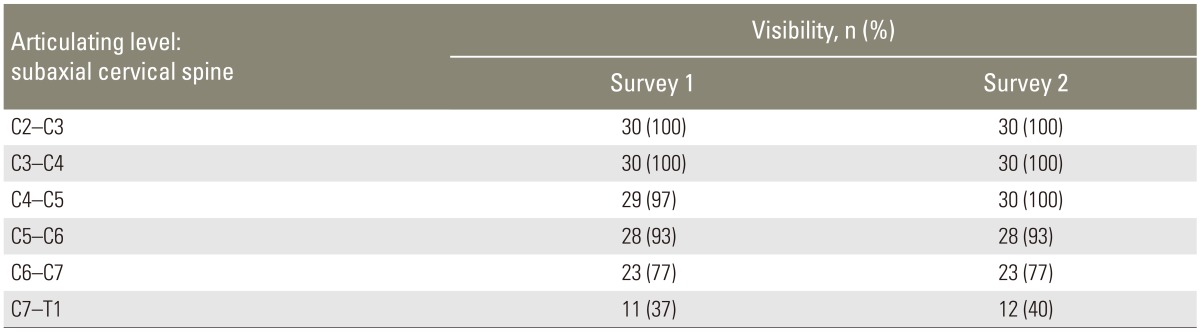
The visibility of each level of the subaxial cervical spine on lateral plain X-rays was presented in Table 3. The articulating level between C3 and C4 was visible in all cases, whereas the cervicothoracic junction was visible in 11 (37%) and 12 (40%) of the 30 cases in surveys 1&2, respectively. The raw agreement on the lowest visible level of the cervical spine was 70% (╬║0.54; 95% CI, 0.47-0.60) and 71% (╬║0.56; 95% CI, 0.49-0.62) for surveys 1 and 2, respectively.
In the absence of a gold reference standard, the most likely outcomes were estimated with 3 different majority rules (Table 4). Except for 1 case, there was 75% agreement on the presence or absence of a facet joint injury in all cases using CT scan images. Hence, the 75% agreement value was used as a proxy reference standard to assess the accuracy of facet joint injury detection on plain radiographs.
Of the 21 facet joint injuries discerned on CT images, 10 were detected in both plain X-ray surveys (sensitivity, 0.48; 95% CI, 0.26-0.70) by the majority of the raters. There were no false positive facet joint injuries in either of the first 2 X-ray surveys (specificity, 1.0; 95% CI, 0.63-1.0). Eleven of the 21 cases (52%) with facet joint injuries seen on CT scan images were missed in the plain radiograph series. Five cases had an injury below the lowest visible articulating level, on lateral-view radiographs; whereas the other 6 cases had a facet joint injury at a visible level on radiographs (Fig. 2).
The raw agreement on the presence of a facet joint injury was 72% (╬║0.43; 95% CI, 0.36-0.51) and 77% (╬║0.53; 95% CI, 0.45-0.61) for the first and second plain radiographic survey, respectively. Higher raw agreement values were seen in the third and fourth surveys with CT scan images: 89% (╬║0.75; 95% CI, 0.64-0.86) and 90% (╬║0.76; 95% CI, 0.64-0.88), respectively. Intra-rater reliability was strong for both plain radiography (╬║0.85; 95% CI, 0.72-0.98) and CT scan images (╬║0.92; 95% CI, 0.78-0.1.06) (Table 5).
The agreement on determining the most severely affected level of injury could be calculated for those cases that reached 100% agreement on the presence of a facet joint injury. Where the numbers of cases reaching 100% agreement in the first 2 plain radiographic surveys were low (5 and 7 cases, respectively), inter- and intra-rater agreement coefficients on the level of injury were higher than seen in the CT scan images surveys (Table 5).
There was poor agreement on whether an injury was of uni- or bilateral nature in the first (╬║0.21; 95% CI, -0.13 to 0.55) and second (╬║0.26; 95% CI, 0.12-0.41) plain radiography surveys. In contrast, the CT scan image surveys resulted in fair to good inter-rater agreement values (Table 5). Intra-rater reliability was strong for both plain radiography (╬║0.87; 95% CI, 0.59-1.14) and CT scan images (╬║0.88; 95% CI, 0.69-1.07).
Similarly, poor agreement values were seen for classifying the injuries according to the injury characteristics listed in Table 2 using plain radiographs (Table 5). CT scan image surveys resulted in higher inter-rater agreement values. Intra-rater reliability was fair to good for plain radiography (╬║0.54; 95% CI, 0.39-0.69) and CT scan images (╬║0.68; 95% CI, 0.59-0.78), respectively.
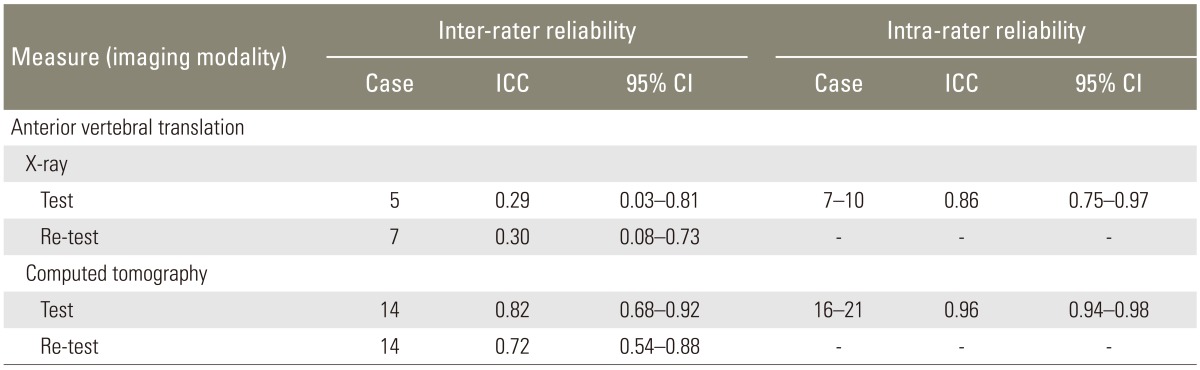
Compared to the plain radiography surveys, inter- and intra-rater agreement on the vertebral body translation was higher for the CT scan image surveys (Table 6).
In this radiologic imaging measurement study, more than half of the facet joint injuries detected on CT scan images were not detected on plain radiographs of the cervical spine. Since the injured levels were visible on the lateral views of plain radiographs in more than half of the cases, the missed injuries could not be simply attributed to poor visibility of lower cervical spinal levels. When compared to plain radiographs, CT scan images resulted in superior inter- and intra-rater agreement values for assessing morphologic injury characteristics of facet joint injuries. The fair to good agreement values found for the facet joint injury categories indicate that further refinement of definition s of these injury categories should be considered in future morphological classifications of the subaxial cervical spine.
The cases under study represent a pseudo-random sample from a consecutive series of high-energy, blunt trauma patients. Since the focus of this study was to examine the accuracy and precision of facet joint injuries of the subaxial cervical spine, we pre-defined a preferred ratio of 2 out of 3 cases with a facet joint injury. As this ratio was not met, 5 cases without facet joint injury were replaced by 5 cases with facet joint injury. This focused approach resulted in a limited epidemiological validity of our findings. Nonetheless, this study concurs with findings from previous studies [8], demonstrating the high specificity (i.e., ratio of true negative cases to all negative cases) of plain radiographs to detect cervical spine injuries. However, from a clinical perspective, the sensitivity of plain radiographs to detect cervical spine injuries is of primary interest. The current study is the first to demonstrate an alarmingly low sensitivity of plain radiographs (42%) to detect facet joint injuries of the cervical spine. Clearly, this study adds to the body of literature advocating the use of CT of the cervical spine in high-energy, blunt trauma patients [789].
The outcomes of the current study also have implications for future cervical spinal injury classification studies. Sample numbers were too small to calculate the accuracy of uni- or bilateral facet joint injury detection on plain radiographs. However, we demonstrated that the agreement on whether an injury is of uni- or bilateral nature using plain radiography is much lower than using CT scan images. Therefore the current study reinforces the notion that plain radiographs should not be used for the classification of cervical spine injuries [12]. The categorization of facet joint injuries of the cervical spine presented in Table 2 did not lead to satisfactory agreement values in the CT scan surveys. Further refined categorical descriptions of injury and introductions of graphic representations and example cases may result in higher agreement values. Another factor contributing to ambiguity of facet joint injury categories is that some surgeons consider facet joint injuries with the appearance of a unilateral injury on imaging as a bilateral injury by definition [17]. Some authors have advocated the use of magnetic resonance (MR) imaging for classifying facet joint injuries [18], however, a recent systematic review indicated that MR imaging resulted in poor agreement values for detecting discoligamentous injuries of the thoracolumbar spine [19]. This outcome might also be applicable to cervical spine injuries, hence, requires further study.
Strengths of our study included the prospectively collected data from a well-defined cohort of consecutively recruited trauma patients in a tertiary referral hospital, the use of complete series of plain radiographs and CT scan images and the use of raters blinded to clinical case history. Nonetheless, several potential limitations of our study warrant consideration. Although plain radiographs and CT scan images were blinded, 4 sets of randomly ordered cases were assessed in 1 day. This may have led to both recall bias and fatigue bias. For feasibility reasons, a number of randomly selected cases without a facet joint injury were replaced with cases with a facet joint injury. This has resulted in the limited epidemiological validity of our findings. Four fellowship-trained spine surgeons and 4 spinal surgery fellows scored the cases. The number of cases was too small to perform a subgroup analysis to adjust for raters' experience. Finally, the study findings cannot be generalized to the low-energy trauma population. Hence, further assessment of the accuracy of X-rays in facet joint injury detection in this particular population, are warranted.
Plain radiographs of the cervical spine are not reliable for the assessment of subaxial cervical spine trauma. Missed injuries cannot be simply attributed to poor visibility of lower cervical spinal levels on the lateral views of plain radiographs as raters also missed facet joint injuries on visible levels. When compared to plain radiographs, CT images resulted in equal or superior inter- and intra-rater agreement values for all studied facet joint related radiologic imaging measurements. Whilst the current study indicates that further refinements are needed, optimization of facet joint injury categories should be considered in future morphological classifications of the subaxial cervical spine.
Acknowledgments
The authors thank the Department of Radiology, Radboud University Medical Centre Nijmegen, the Netherlands for the availability of imaging material for the current study. We thank Melissa Anenden for her assistance in data collection and data processing. We acknowledge the AOSpine Asia Pacific Board for providing financial support for raters' travel and accommodation expenses to attend the investigators' meeting. We also thank Mr. Derek Lai for his assistance during the preparations of this study.
Conflict of Interest
Conflict of Interest: The AOSpine Asia Pacific Board provided financial support for raters' travel and accommodation expenses to attend the investigators' meeting. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. The authors have no financial interest in the subject of this article. The manuscript submitted does not contain information about medical device(s).
References
1. Hasler RM, Exadaktylos AK, Bouamra O, et al. Epidemiology and predictors of cervical spine injury in adult major trauma patients: a multicenter cohort study. J Trauma Acute Care Surg 2012 72:975ŌĆō981. PMID: 22491614.


2. Platzer P, Hauswirth N, Jaindl M, Chatwani S, Vecsei V, Gaebler C. Delayed or missed diagnosis of cervical spine injuries. J Trauma 2006 61:150ŌĆō155. PMID: 16832263.


3. Grossman MD, Reilly PM, Gillett T, Gillett D. National survey of the incidence of cervical spine injury and approach to cervical spine clearance in U.S. trauma centers. J Trauma 1999 47:684ŌĆō690. PMID: 10528602.


4. Thomas J, Rideau AM, Paulson EK, Bisset GS 3rd. Emergency department imaging: current practice. J Am Coll Radiol 2008 5:811ŌĆō816.e2. PMID: 18585658.


5. Sheikh K, Belfi LM, Sharma R, Baad M, Sanelli PC. Evaluation of acute cervical spine imaging based on ACR Appropriateness Criteria(R). Emerg Radiol 2012 19:11ŌĆō17. PMID: 22057542.


6. Lee SH, Sung JK. Unilateral lateral mass-facet fractures with rotational instability: new classification and a review of 39 cases treated conservatively and with single segment anterior fusion. J Trauma 2009 66:758ŌĆō767. PMID: 19276750.


7. Bailitz J, Starr F, Beecroft M, et al. CT should replace three-view radiographs as the initial screening test in patients at high, moderate, and low risk for blunt cervical spine injury: a prospective comparison. J Trauma 2009 66:1605ŌĆō1609. PMID: 19509621.


8. Gale SC, Gracias VH, Reilly PM, Schwab CW. The inefficiency of plain radiography to evaluate the cervical spine after blunt trauma. J Trauma 2005 59:1121ŌĆō1125. PMID: 16385289.


9. Griffen MM, Frykberg ER, Kerwin AJ, et al. Radiographic clearance of blunt cervical spine injury: plain radiograph or computed tomography scan? J Trauma 2003 55:222ŌĆō226. PMID: 12913629.


10. Dvorak MF, Fisher CG, Aarabi B, et al. Clinical outcomes of 90 isolated unilateral facet fractures, subluxations, and dislocations treated surgically and nonoperatively. Spine (Phila Pa 1976) 2007 32:3007ŌĆō3013. PMID: 18091494.


11. Schotanus M, van Middendorp JJ, Hosman AJ. Isolated transverse process fractures of the subaxial cervical spine: a clinically insignificant injury or not: a prospective, longitudinal analysis in a consecutive high-energy blunt trauma population. Spine (Phila Pa 1976) 2010 35:E965ŌĆōE970. PMID: 20479701.


12. van Middendorp JJ, Audige L, Hanson B, Chapman JR, Hosman AJ. What should an ideal spinal injury classification system consist of? A methodological review and conceptual proposal for future classifications. Eur Spine J 2010 19:1238ŌĆō1249. PMID: 20464432.



13. Bono CM, Vaccaro AR, Fehlings M, et al. Measurement techniques for lower cervical spine injuries: consensus statement of the Spine Trauma Study Group. Spine (Phila Pa 1976) 2006 31:603ŌĆō609. PMID: 16508560.


15. Fleiss JL. Statistical methods for rates and proportions. 2nd ed. New York: Wiley; 1981.
16. Audige L, Bhandari M, Kellam J. How reliable are reliability studies of fracture classifications? A systematic review of their methodologies. Acta Orthop Scand 2004 75:184ŌĆō194. PMID: 15180234.


17. Nadeau M, McLachlin SD, Bailey SI, Gurr KR, Dunning CE, Bailey CS. A biomechanical assessment of soft-tissue damage in the cervical spine following a unilateral facet injury. J Bone Joint Surg Am 2012 94:e156PMID: 23138243.


18. Vaccaro AR, Madigan L, Schweitzer ME, Flanders AE, Hilibrand AS, Albert TJ. Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine (Phila Pa 1976) 2001 26:1866ŌĆō1872. PMID: 11568695.


19. van Middendorp JJ, Patel AA, Schuetz M, Joaquim AF. The precision, accuracy and validity of detecting posterior ligamentous complex injuries of the thoracic and lumbar spine: a critical appraisal of the literature. Eur Spine J 2013 22:461ŌĆō474. PMID: 23208081.


Fig.┬Ā1
Measurement technique for vertebral body translation. From a lateral perspective, a posterior tangent line is drawn along the vertebral bodies. The distance between these lines is measured at the level of the inferior aspect of the upper vertebra.

Fig.┬Ā2
(A-E) This case represents a 42-year-old man who sustained both a closed head injury and a cervical spine injury.
Table┬Ā1
Inclusion criteria for the high-energy, blunt trauma study population from which a study sample was drawn
Table┬Ā2
A morphological categorization of lateral mass and facet joint injuries applied in this study
Table┬Ā3
Number and proportion of cases with visible articulating levels of the subaxial cervical spine on plain lateral X-rays as assessed in the first two surveys using median values (30 cases, 8 raters)
Table┬Ā4
Number and proportion of cases reaching a threshold of raw agreement on the presence or absence of a facet joint injury of the subaxial cervical spine in the 4 surveys (30 cases, 8 raters) using three different majority rules: >50%, >75%, and 100%