Radiographic Assessment of Effect of Congenital Monosegment Synostosis of Lower Cervical Spine between C2-C6 on Adjacent Mobile Segments
Article information
Abstract
Study Design
A prospective radiographic study of cervical spine with congenital monosegment fusion.
Purpose
To evaluate the effect of cervical synostosis on adjacent segments and the vertebral morphology.
Overview of Literature
There are numerous clinical studies of adjacent segment disease (ASD) after monosegment surgical fusion. However, there was no report on ASD in the cervical spine with congenital monosegment synostosis.
Methods
Radiograms of 52 patients, aged 5 to 90 years, with congenital monosegment synostosis (CMS) between C2 and C6, who complained of neck/shoulder discomfort or pain were studied. 51 were normally aligned and one was kyphotically aligned.
Results
Spondylosis was not found in the patients below 35 years of age. Only 12 out of 24 patients with normally aligned C2-3 synostosis had spondylosis in 19 more caudal segments, and only one at C3-4. A patient with kyphotic C2-3 had spondylolysis at C3-4. In 8 patients with C3-4 synostosis, spondylosis was found in only 9 caudal segments (4 at C4-5, 4 at C5-6, and 1 at C6-7). The caudate C4-5 disc was the most liable to degenerate in comparison with other caudate segments. Caudal corporal flaring and inwaisting of the synostotic vertebra were the features that were the most evident. In 2 of 9 C4-5 and 7 out of 10 C5-6 synostosis patients, spondylosis was found at the two adjacent cephalad and caudate segments, respectively. Only corporal inwaisting without flaring was found. In all cases, spondylosis was confined to the adjacent segments. More advanced spondylosis was found in the immediate caudal segment than the cephalad one.
Conclusions
It is concluded that spondylosis at the mobile segments in a synostotic spine is thought to be a fusion-related pathology rather than solely age-related disc degeneration. Those data suggested that CMS definitely precipitated the disc degeneration in the adjacent segments.
Introduction
Congenital cervical monosegment synostosis is a type of failed segmentation of unknown origin. It has two morphological alignment types: normally and abnormally aligned ones. Some consider it an incidental radiological finding unrelated to disease, while others consider it to be the cause of secondary mobility disturbances and degenerative changes of the adjacent segments in the same manner that an iatrogenically created immobile segment does [1,2,3,4,5,6,7,8,9]. Generally, it has been known that an iatrogenically created immobile segment in the spine predisposes to alterations of the biomechanics at the neighboring mobile segments and may result in high demands on the adjacent intervertebral segments; in addition, instability and degenerative changes at the adjacent segments (ASD) may occur, although completely opposite opinions have also been reported. Of course, it is already known that the incidence of ASD is higher in the cases of surgical lumbar spine fusion than cervical spine fusion, and that the incidence of ASD in thoracic spine fusion is the lowest [10,11,12,13,14,15]. We evaluated the morphologies of the synostotic cervical vertebra of different levels on radiograms and their effect on the cephalad and caudal adjacent discs and vertebrae.
Material and Methods
Radiographs of 52 patients (28 males and 24 females), aged 5 to 90 years, with congenital monosegment synostosis between C2 and C6, obtained at 7 hospitals between April 1995 to May 2012, were reviewed. All cases were found incidentally on radiograms (Table 1).

Monosegment synostosis of 4 different levels between C2-C6 on incidences of adjacent segment spondylosis (disc degeneration)
No patient clinically presented with an obvious short-neck appearance. The patients' complaints included neck/shoulder discomfort/pain (n=23), neck motion limitation (n=6), an acute wry neck, which was possibly an atlantoaxial rotatory subluxation (a 5-year-old boy), and post-traumatic transient myelopathy symptoms (SCIWORA; a 44-year-old man).
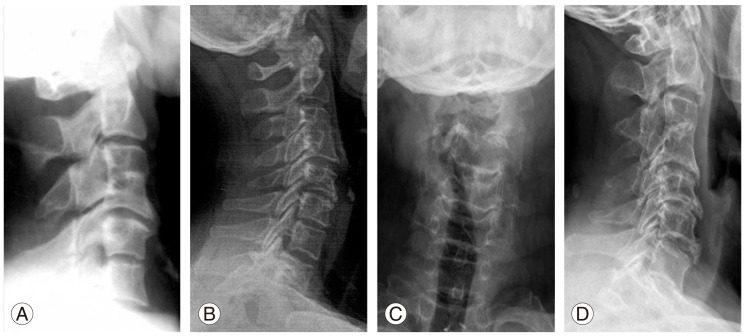
There was synostosis at four different levels: C2-3 in 25 (11 male/14 females), C3-4 in 8 (6 males/2 females), C4-5 in 9 (6 males/3 females), and C5-6 in 10 patients (5 males/5 females) (Fig. 1).
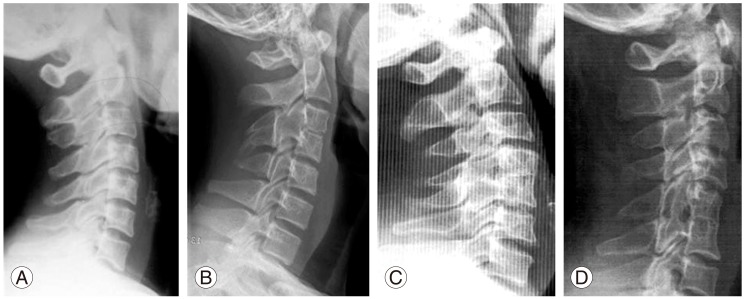
Congenital monosegment synostosis with intact adjacent joints at 4 different levels are shown: (A) C2-3 synostosis, (B) C3-4 synostosis, (C) C4-5 synostosis, (D) C5-6 synostosis.
The patients' ages ranged from 5 to 90 years: 5 to 74 years in C2-3 synostosis cases, 13 to 69 years in C3-4, 22 to 90 years in C4-5, and 11 to 67 years in C5-6 synostosis.
Neutral anteroposterior and lateral radiograms were obtained to evaluate the effect of the synostosis and its alignment on adjacent segments and vertebral bodies, the segmental mobility, cervical curve, and to assess the morphology of the synostotic vertebra and discs.
Results
The most common patients' complaints were nuchal discomfort/pain (n=23 patients). The other combined conditions were wry neck in a child (Fig. 2), neck motion limitation in 6 adults, herniated disc symptoms at C3-4 in an adult, SCIWORA in an adult, and C1 ring hypoplasia in an adult. In none was a short neck appearance found even in the case of kyphotic C2-3 synostosis (Fig. 3). All patients had a normal canal size of the lower cervical spine with the Pavlov ratio over 0.8.
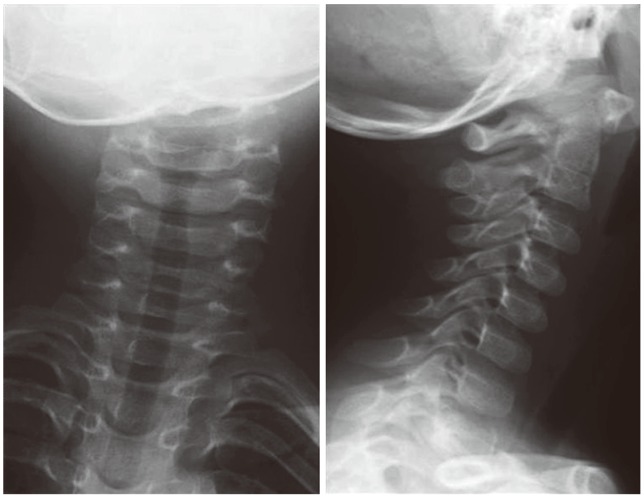
Acute onset torticollis in a 5-year-old boy without cervical disc degeneration, segmental instability, and other anomaly. The torticollis was thought to be unrelated with the C2-3 block vertebra, and to be caused by the sudden development of atlantoaxial rotatory subluxation after a bout of illness with the flu.
Kyphotic C2-3 block vertebrae in a 43-year-old female (A, B): Compensatory hyperlordosis of the caudal mobile segments, spondylosis at C3-4, and C4 retrolisthesis were complications. She had no neurological compromise.
1) Spondylosis were found in 13 out of 25 patients with C2-3 synostosis over the age of 40 years. Most of the cases of spondylosis were distributed in C4-5 and C5-6, and immediate adjacent segment involvement was found in only 2 patients (C1-2 in one [Fig. 4] and C3-4 in one, each). Among the twelve patients with normally aligned C2-3 synostosis, 8 had single level disc degeneration, 4 had 2 levels, and 1 had three levels (Fig. 5). C3-4 disc degeneration and C4 retrolisthesis in the compensatory hyperlodortic curve were found in a patient with kyphotic synostosis.
A 40-year-old lady with a C2-3 synostosis sustained injury of the neck. Left atlantoaxial facet (C1-2) arthrosis was found incidentally on plain radiograms. She was asymptomatic before the injury. No degenerative disc disease was found at the caudal mobile segments.

Lateral radiograms of the cervical spines of 4 subjects with C2-3 synostosis showing spondylotic segments. (A, B) Monosegment spondylosis at C5-6 in a 51-year-old and a 54-year-old female. (C) Two-segment spondylosis at C4-5 and C6-7 in a 55-year-old male. (D) Three-segment spondylosis at C4-5, C5-6, and C6-7 in a 52-year-old male
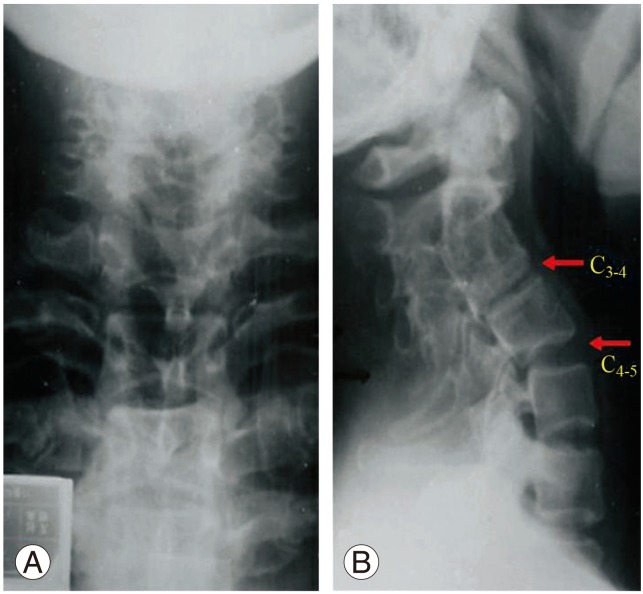
2) In 8 cases of C3-4 synostosis, the incidence of spondylosis was 62.5%; there was no spondylosis in the cephalad motion segments, while spondylosis was localized only to the caudal segments: C4-5 (4 patients), C5-6 segments (4 patients) and C5-6 segments (1 patient) (Fig. 6). Caudal corporal flaring and inwaisting of the synostotic vertebra were most evidently shown. Adaptive morphological enlargement of the caudal part of the synostotic vertebra and disc could not lessen the severity and progress of adjacent segment disease of the caudate segments.
Lateral radiograms of two patients, aged 40 years (A) and 42 years (B) with congenital C3-4 synostosis showing corporal flaring of the caudal half of the C3-4 block vertebra. In the (A) radiogram, the discs are not narrowed at the C4-5 and C5-6 levels, while on the (B) radiogram, mild disc degeneration is observed at C5-6 and C6-7, but not at C4-5. Radiograms of the cervical spine in a 69 year-old man (C, D), showing the flared caudal half of the synostotic C3-4 vertebrae; however, the upper part of C5 body did not develop the adaptive corporal flaring. Severe degeneration of the C4-5 and C5-6 discs, and large anterior claw spurs at the inferior margins of C4, C5, and C6 are shown. However, the C6-7 disc was not narrowed.
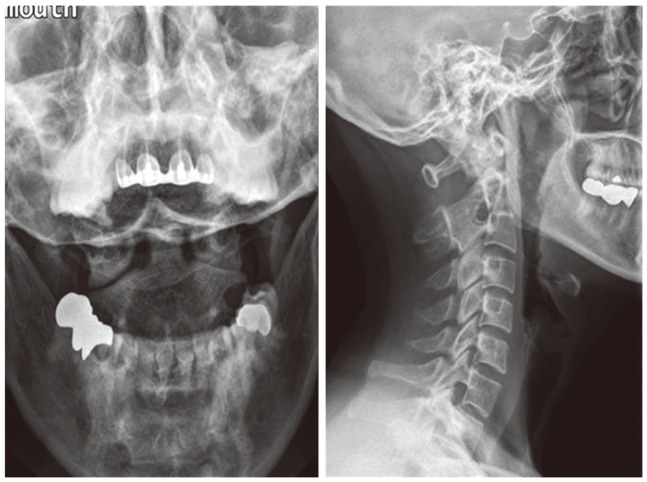
3) Among 9 patients with C4-5 synostosis, two (25%) out of 9 patients had spondylosis at the cephalad C3-4 segment, while 2 had spondylosis at caudate C5-6 (2) and C6-7 (1) (Fig. 7).

Lateral radiograms of 3 patients with congenital C4-5 synostosis (A-C), aged from 56 to 90 years, showing a slightly inwaisted fused vertebral body with some caudal corporal flaring. In all 3 patients, spondylotic changes were observed at the proximal and caudal discs, respectively.
4) Among 10 C5-6 synostosis patients, 7 (70%) had spondylosis; C3-4/C4-5 in 4 and C6-7/C7-T1 in 8 patients (Fig. 8).

Lateral radiograms of 7 subjects with C5-6 synostosis in normal alignment, aged 43 years (A), 44 years (B), 46 years (C), 51 years (D), 41 years (E), 58 years (F), and 67 years (G), showing the various degrees of disc degeneration with the flattened curve. In none of these patients were the cranial discs degenerated. Vertebral inwaisting is less evident. (E) Advanced disc degeneration at the adjacent cranial C4-5 segment and early disc degeneration at the caudal C6-7 segment. Loss of the normal lordotic curve is seen. (F) Relatively advanced disc degeneration is seen at both the immediate adjacent cranial (C4-5) and caudal (C6-7) discs. (G) Relatively advanced disc change is seen only at the caudal (C6-7) segment, but the cranial discs are all well preserved.
In summary, spondylosis was mostly confined to the adjacent segments, particularly the caudal segments. None of the cases were complicated by segmental hypermobility such as rotational and/or translational instability (Table 1).
Vertebral flaring of the caudal part of the C3-4 synostotic vertebra and the matching flaring of the upper part of the adjacent C4 vertebral body were most commonly seen together with relatively advanced ASD and remarkable inwaisting. However, these adaptive corporal morphological changes became less conspicuous in the cases of more caudal vertebral synostosis. Corporal inwaisting was the least in C2-3 synostotic vertebra and the most conspicuous in C3-4 synostotic vertebra, and became less the more caudal the synostotic vertebrae became, with less mobile segments.
Discussion
Intervertebral discs of the normal spine degenerate gradually in the course of the natural aging process. However, there are notable differences in the anatomy and loading characteristics between the cervical and lumbar spines which result in differences in the pattern of involvement, rate of degeneration and clinical presentation [16,17,18,19,20,21]. Unlike the lumbar spine, the cervical intervertebral discs experience significantly less axial loading over time. The cervical spine, anatomically, is also characterized by the presence of the uncovertebral joint. Luschka's joints contain fibrocartilage that can narrow and form osteophytes during the course of degeneration. Although the uncovertebral joints are less than one-third of the normal disc height, they are able to bear some of the axial load imparted to the cervical spine, thereby decreasing the overall loads placed on the intervertebral discs. These factors help to make the clinical entity of cervical disc herniation rare in individuals younger than 30 years and more common later during the fifth and sixth decades of life. Also the incidence of post-fusion adjacent segment pathology in the cervical spine is less than that of the lumbar spine.
Up until now, no one has studied adjacent segment pathology in the case of congenital monosegment synostosis in normal sagittal alignment, although the authors could find studies of the cervical spine in Kippel-Feil's syndrome. It is considered that congenital monosegment synostosis of the lower cervical spine may alter kinematics and exert extra stress on the adjacent unfused/mobile segments, resulting in progressive joint degeneration and segmental instability, which are seen frequently in cases of surgical fusion [15].
Disc degeneration at the adjacent joints after surgical cervical spine fusion has now become a really menacing problem because its reported incidence is high: 2.5% per annum and it has become 25% in 10 years. The controversial issue related with ASD is whether the ASD is a natural constitutional phenomenon or an iatrogenic one. To solve this controversial issue as the first step of an investigational study, congenital synostosis models were chosen as the control [15,16,17,18].
ASD has been known to be associated with age, presumably due to differences in physical adaptability to stress between children and adults. However, there has been argument over whether the fused spine transfers its lost bearing load and motion to the adjacent segments which are forced to compensate for the lost bearing load and motion. Also, there are conflicting reports on whether this actually occurs, and whether there is an observable relationship between motion and development of disc degeneration after the fusion.
In our study, ASD was mostly localized to the adjacent joints, particularly the caudal ones in the cases of synostosis between C2-C6. The interesting findings were that in the cases of C2-3 synostosis, ASD developed in the immediate cephalad unilateral facet joint (C1-C2), and that mostly caudal segments below C4-5 were involved by skipping the C3-4 segments. This fact suggested indirectly that the normally aligned C2-3 synostosis did not affect the immediate caudal segment (C3-4). Even the kyphotic C2-3 block vertebra did not precipitate ASD earlier than the normally aligned one, although the compensatory hyperlordosis below C2-3 block resulted in spondylosis at the C3-4 segment and C4 retrolisthesis at the apex of the hyperlordosis, which was not shown in the normally aligned segment of any level. Thus, it is speculated that the pediatric spine adapts well even to altered biomechanics. ASD in monosegment synostosis could be related to the block vertebra, because the discs distant from the fused vertebra were kept intact or were minimally degenerated in the current series.
In summary the adjacent disc degeneration seemed primarily to be precipitated by the constitutional factors including age, and additionally was exacerbated by the direct load and motion shift in a certain degree from the fused segments because disc degeneration was not observed before the age of 35 years regardless of the fusion alignment.
Also a question could be raised as to whether disc degenerates faster and more severely by fusion or not, and when the more compensatory role of the adjacent mobile segment starts to become imposed. Also it is assumed that ASD is unrelated with hypermobility secondary to synsostosis. Normal cervical lordosis could not be maintained in patients with multisegment spondylosis.
Through this study, it was again confirmed that the pediatric spine could adapt well to biomechanical alterations. Consequently, the adjacent motion segments of the monosegment block vertebra could compensate for the loss in motion and load by developing 1) the strong soft tissue stabilizers without losing the original supporting and mobility functions, and 2) adaptive morphological changes such as broadening of the disc, matching with the flared vertebral body and vertebral body inwaisting [20]. However, it is evident that the adult spine adapts poorly to the altered biomechanics, and that it can not develop the adaptive morphological changes seen in the pediatric spine except for corporal inwaisting.
Corporal flaring of the synostotic vertebra and disc enlargement are the most characteristic features of C3-4 synostosis, and are the manifestations of the morphological adaptations together with the corporal inwaisting that develop to meet the biomechanical need in the pediatric spine. The corporal flaring became less evident in the C4-5 synostotic vertebra and was not seen in the C5-6 synostotic vertebra.
Vertebral body inwaisting in general is seen in the normal human spine, in people aged over 2 years [17]. In the motionless spine such as in ankylosing spondylitis, each vertebral body is squared without inwaisting [17,18]. When segmental motion is excessive, more inwaisting develops [20]. This phenomenon suggests indirectly the degree of motion range at each motion segment. In the current series, inwaisting became less evident in the C5-6 synostotic vertebra and in the elderly with less mobile segments above and below due to spondylosis.
Limitations of this study were the small number of cases, the absence of cases with variably severe kyphotic fusion and the absence of cases that were not age-related among the cases of surgically fused monosegment synostosis that acted as controls.
It is debatable whether congenitally and surgically fused vertebrae affect the adjacent mobile segments in a similar way [1,15,16,17,18,19,20,21]. This would be possible only if 1) the segments adjacent to the block vertebrae are truly normal to start with, and 2) the side effects of the surgical fusion are negligible. Both assumptions are speculative [3]. Our findings on congenital monosegment synostosis of the lower cervical spine between C2-C6 may not be comparable to those of the surgically fused ones. Therefore, it is speculated that even normally aligned congenital monosegment synostosis is likely to precipitate the development of adjacent joint disease, though late in life. Thus, it could be concluded that synostosis is an ASD-precipitating factor which is not benign clinically, though none of the cases in the current series were subjected to surgical care because of ASD.
Conclusions
Spondylosis at the mobile segment in a synostotic cervical spine is thought to be a fusion-related pathology rather than solely age-related disc degeneration. The resultant data suggested that congenital monosegment synostosis precipitated definitely the ASD.
Notes
No potential conflict of interest relevant to this article was reported.