Accuracy of Free Hand Pedicle Screw Installation in the Thoracic and Lumbar Spine by a Young Surgeon: An Analysis of the First Consecutive 306 Screws Using Computed Tomography
Article information
Abstract
Study Design
A retrospective cross-sectional study.
Purpose
The purpose of this study is to evaluate the accuracy and safety of free-hand pedicle screw insertion performed by a young surgeon.
Overview of Literature
Few articles exist regarding the safety of the free-hand technique without inspection by an experienced spine surgeon.
Methods
The index surgeon has performed spinal surgery for 2 years by himself. He performed fluoroscopy-assisted pedicle screw installation for his first year. Since then, he has used the free-hand technique. We retrospectively reviewed the records of all consecutive patients undergoing pedicle screw installation using the free-hand technique without fluoroscopy in the thoracic or lumbar spine by the index surgeon. Incidence and extent of cortical breach by misplaced pedicle screw was determined by a review of postoperative computed tomography (CT) images.
Results
A total of 36 patients received 306 free-hand placed pedicle screws in the thoracic or lumbar spine. A total of 12 screws (3.9%) were identified as breaching the pedicle in 9 patients. Upper thoracic spine was the most frequent location of screw breach (10.8%). Lateral breach (2.3%) was more frequent than any other direction. Screw breach on the right side (9 patients) was more common than that on the left side (3 patients) (p<0.01).
Conclusions
An analysis by CT scan shows that young spine surgeons who have trained under the supervision of an experienced surgeon can safely place free-hand pedicle screws with an acceptable breach rate through repetitive confirmatory steps.
Introduction
Pedicle screws have been commonly used in posterior spinal surgeries since 1959 [1]. Because pedicle screws can stabilize all three columns of the spine, they are the most popular posterior spinal segmental fixation system, even in the deformed spine [2]. On the other hand, pedicle screw malposition has the potential risk for permanent neurological deficits. Several methods of pedicle screw installation (PSI) have been developed to enhance the accuracy of its usage, including intraoperative fluoroscopy, Kirschner wire, the funnel technique, and the stereotactic-guided technique [3,4,5,6,7,8,9,10]. PSI assisted by fluoroscopy is a commonly used technique.
Although the fluoroscopy-assisted technique offers two-dimensional images of pedicle and screw to guide placement, it is associated with increased radiation exposure to both patients and surgeons. In long-level screw placement for patients with adolescent idiopathic scoliosis or adult spinal deformity, radiation exposure may be especially dangerous [11,12]. In adolescent idiopathic scoliosis surgery, the surgeons are projected to receive 13.49 mSv of whole body ionizing radiation, exceeding the recommended limits of 10 mSv per year of life. At the levels estimated, a surgeon beginning his/her career at age 30 years would exceed the lifetime limit in less than 10 years [13]. Furthermore, adolescent patients have a risk of radiation-induced malignancy.
The accuracy and safety of the free-hand technique were addressed in several papers [14,15,16,17]. However, the free-hand technique was implemented by an experienced spine surgeon or under the guidance of an experienced surgeon in almost all previous studies. The purpose of this study was to evaluate the accuracy and safety of the free-hand technique performed by a young attending surgeon without inspection by an experienced spine surgeon.
Materials and Methods
1. Patients
We retrospectively reviewed the records of all consecutive patients receiving free-hand PSI in the thoracic or lumbar spine from December 2010 through July 2011. Thirty-six patients (17 males and 19 females) were included in this study. Free-hand PSI was performed by a young academic spinal surgeon. The index surgeon had performed spinal surgeries for two years by himself, excluding the period of his fellowship program. The index surgeon had practiced fluoroscopy-guided PSI during his first year. He then learned the free-hand technique from the senior author and practiced this skill on cadavers [14]. Three times he implemented the free-hand technique under the guidance of the experienced surgeon. He has used the free-hand technique continuously since then.
Postoperative computed tomography (CT) scans were obtained the day after surgery to evaluate the position of the pedicle screws by 3 mm thickness. The accuracy of each pedicle screw placement was objectively evaluated in three-dimensional CT scans. A prior investigation divided the pedicle violations into three grades as follows: grade I, screws within the pedicular cortical margin; grade II, screws that extended <2 mm beyond the pedicular cortex; and grade III, screws that extended ≥2 mm beyond the pedicular cortex [5]. In another study, the cortical breach was classified as <2 mm, 2-4 mm or >4 mm [18]. Other studies categorized the pedicle breach in 2-mm increments [4,15]. Similar to previous studies of the accuracy of PSI, we defined a breach as an extension of more than 2 mm outside the pedicular margin (Fig. 1). The direction of the cortical breach, such as medial, lateral, superior, or inferior, was also noted in each case. The malposition of the pedicle screws was determined by two independent spine surgeons who reviewed the CT scans.
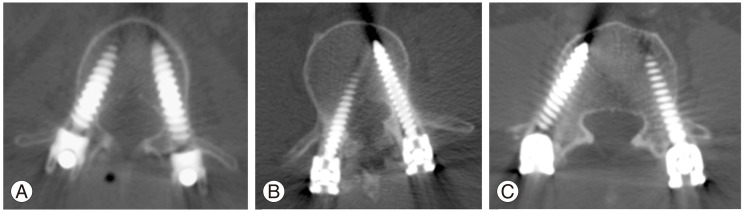
Postoperative computed tomography images show the relationship between the pedicle and the screw. (A) Screws were placed inside the pedicle. (B) The right screw was placed 2 mm beyond the medial side of the pedicle. We defined this as a medial breach. (C) The right screw was inserted more than 2 mm lateral of the pedicle wall.
2. Surgical technique
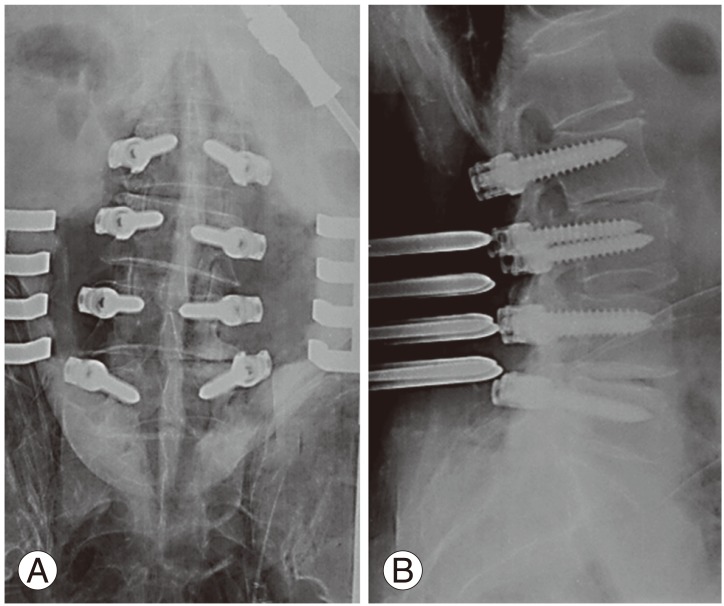
The index surgeon performed free-hand PSI as described by Kim et al. [14,19]. The technique is described in detail in our previous cadaveric study [20]. The first important component of a successful thoracolumbar screw placement is the meticulous exposure of the posterior elements along the subperiosteal plane. The spine was bilaterally exposed from lateral 1 cm from the transverse processes and to the lateral border of the superior articular process. The entry point of the vertebra was at the junction of the bisected transverse process and the lamina at the lateral border of the pars. Detailed entry points by each vertebra were followed based on the method by Kim et al. [14]. The curved pedicle probe was initially pointed laterally as a safety measure to avoid medial wall perforation (Fig. 2). After inserting the pedicle probe tip approximately 15-20 mm (to beyond the isthmic part of the pedicle), the pedicle probe was removed, and five bony walls were confirmed: a bottom and four walls (medial, lateral, superior, and inferior) through ball-tipped sounder. Then, the tip of the pedicle probe was turned to face medially. The pedicle probe was advanced to a maximum depth of 25-40 mm in the thoracic spine. A ball-tipped pedicle sounding device was utilized to repalpate five distinct bony borders. The screw was slowly placed down the pedicle into the body in the same alignment to confirm that it was threaded properly and to allow for viscoelastic expansion. Intraoperative anteroposterior and lateral radiographs were obtained in each patient to assess the presence of pedicle breaches and to confirm the harmonious position of the screws (Fig. 3). Intraoperative spinal cord monitoring including somatosensory and motor evoke potential was used in cases of deformities, tumor, and thoracic spinal cord-compressing lesion. However, direct screw stimulation using triggered electromyogram was not implemented.
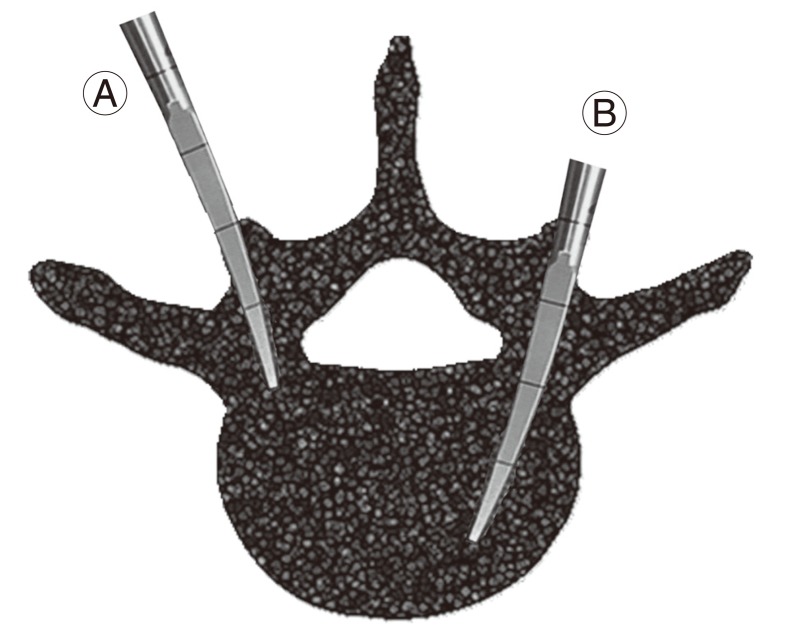
A curved pedicle probe was initially navigated into the lateral side to a depth of 20 mm (the approximate depth of the pedicle) to diminish the likelihood of medial pedicle perforationⒶ. Then the probe was removed, and all four walls were examined by palpation with a ball tipped sound. A curved pedicle probe redirected the probe into the medial side to a depth of 40 mmⒷ.
Results
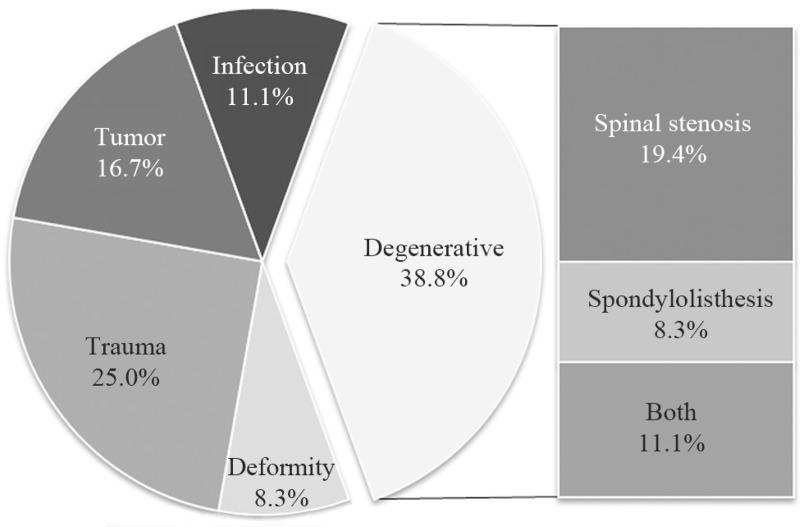
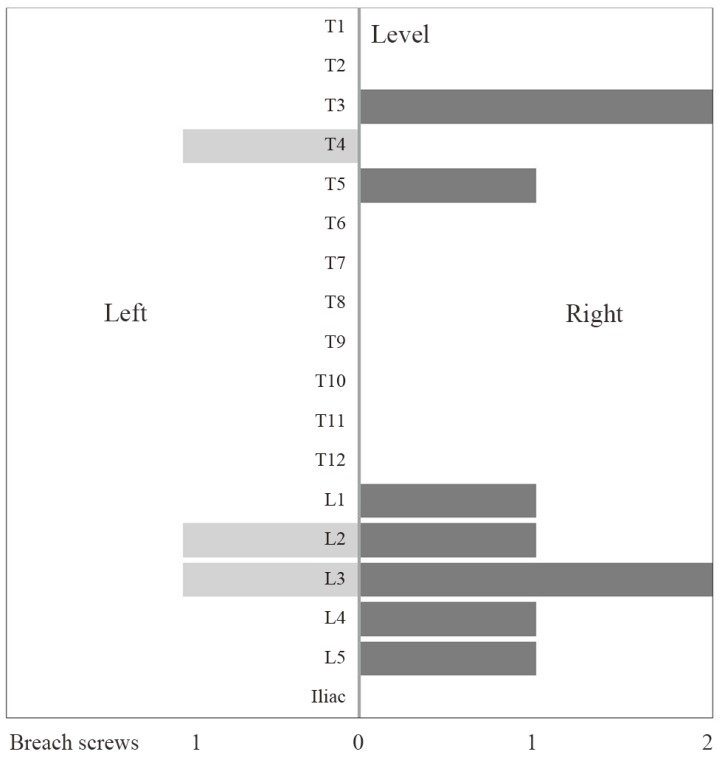
We identified 36 patients with a mean age of 55.6±18.4 years (range, 15-78 years) at the time of surgical treatment. Preoperative clinical symptoms were axial back pain in 19 patients, radiculopathy in 11 patients, and low extremity weakness in 11 patients. The causes of screw placement included degenerative disease (38.8%), trauma (25.0%), tumor (16.7%), infection (11.1%), and deformity (8.3%). Among the degenerative diseases, the indications comprised spinal stenosis (19.4%), spondylolisthesis (8.3%), and both stenosis plus spondylolisthesis (11.1%) (Fig. 4). Over a period of 8 months, a total of 306 consecutive pedicle screws were inserted in the thoracic and lumbar spine by the index surgeon using a free-hand technique. The lumbar spine was the most common region for screw placement, followed by the mid-thoracic and lower thoracic spine. The number of the screws inserted at each level were 2 at T1, 6 at T2, 12 at T3, 17 at T4, 18 at T5, 11 at T6, 12 at T7, 12 at T8, 8 at T9, 16 at T10, 13 at T11, 14 at T12, 26 at L1, 29 at L2, 28 at L3, 36 at L4, 34 at L5, 8 at S1, and 4 at the iliac bone (Fig. 5). There was no change during intraoperative neuromonitoring in all patients.
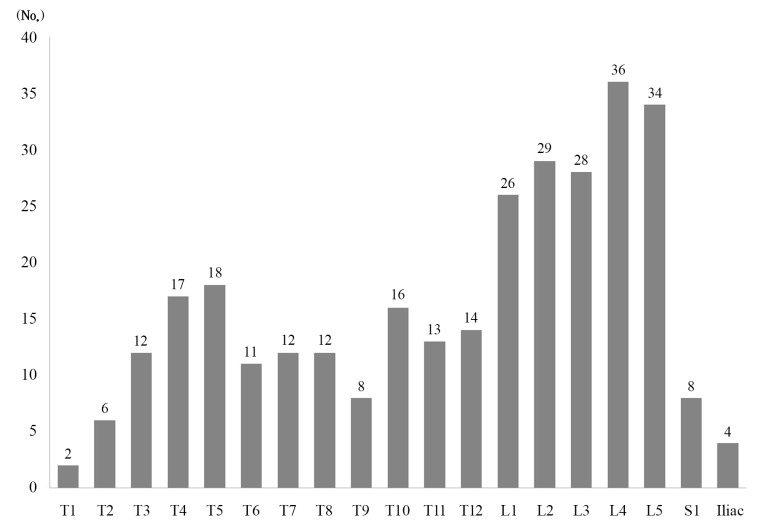
The number of pedicle screws at each level. Among 306 screws, 141 screws were placed in the thoracic spine and 165 screws in the lumbar spine. The lumbar spine was the most frequent site, followed by the upper thoracic (T3-5), and then the mid-lower thoracic spine.
Twelve screws (3.9%) were breached; four (2.8%) were thoracic screws and eight (4.8%) were lumbar screws (p=0.002). The upper thoracic spine (T3-5) demonstrated the highest breach rate (10.8%), and the lumbar spine had a breach rate of 5.2% despite more frequent site placement than in the thoracic spine. The direction of the breach was lateral in seven screws (58.3%), medial in three screws (25.0%), and superior in two screws (16.7%). There was no inferior breached screw. Three screws breached in the left side of patient. The index surgeon stood on the left side of patient while placing screws. Nine screws breached in the right side of patient to the contralateral side of the index surgeon. Thus, the right side screws breached three times more often than the left side screws (p<0.001) (Fig. 6). There was no revision case because of neurological or vascular complication in the patients. During placement of the first 102 screws, five screws breached. During placement of the second 102 screws, four screws breached. During placement of the third 102 screws, three screws breached.
Discussion
Three compartment fixation using pedicle screws in posterior spinal fusion is the most commonly used method. A few studies have indicated that free-hand technique is both as accurate as the fluoroscopy-guided placement, but also harmless in terms of radiation [6,14,21]. Previous researcher reported that even residents can perform PSI with an acceptable breach rate using the free-hand technique [16]. Another study suggested that novice residents should practice these skills on more than four cadavers in the laboratory before proceeding to the operating room [22]. Spine professionals differ from residents in that they have to charge their patients for the surgical outcome. Hence, young spine professionals may face difficulties performing this technique comfortably in the current medico-legal climate and given the technique's learning curve. In the present study, the overall breach rate was 3.9% in 306 screws. Considering the reported breach rate of 1.7% to 6.2%, this study suggests that a young spine surgeon can implement the technique with acceptable accuracy [11,14,23]. During placement of the first 102 screws, a breach occurred with five screws. During placement of the next 102 screws, four screws were misplaced. During placement of the final 102 screws, a breach occurred with three screws.
The majority of breaches (3.9%) were in the lateral (58.3%), medial (25.0%), and superior (16.7%) direction. This result may be attributed to the thicker medial and inferior cortical wall of the pedicle as well as the desire of the surgeon to avoid potential injury to the spinal cord or root. The breach incidence by level was significantly less frequent in the thoracic (2.8%) than the lumbar (4.8%) spine (p=0.002). This result is in contrast to previous studies, which showed that the thoracic spine was misplaced more frequently than the lumbar spine. The upper thoracic screws recorded the highest number of breaches, which was in agreement with previous studies [21]. One plausible reason for the frequent lumbar breach is that we often try to place screws as large as possible in the lumbar spine. We used under 75 mm diameter screws in the lumbar spine despite the 6-7 mm pedicle, considering the ability of the pedicle to expand up to 1.8 times; this may cause pedicle expansion, breach, and fracture [24]. The breach incidence occurred significantly more frequently on the right side (5.9%) than the left (2.0%) side of the spine (p<0.001). Unfortunately, we cannot find any reason or reference for similar findings. In the current study, the index surgeon stood on the left side of the patient to place the right side screws because this was more convenient for the right-handed surgeon. However, it was difficult to estimate adequate convergence for screws on the opposite side. Therefore, placing a pedicle screw on the opposite side is more difficult than on the ipsilateral side. We suggest that surgeons should be careful when placing screws on the opposite side or move to that side of patient.
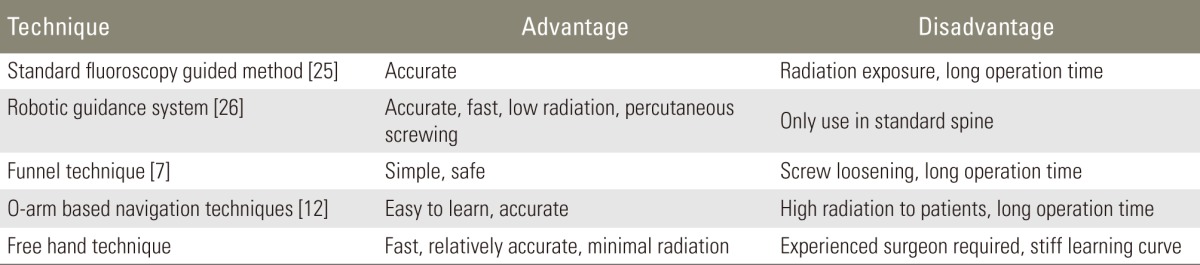
Several studies that have examined the accuracy and safety of pedicle screws are shown in Table 1 [7,12,25,26].
Previous studies have compared the free-hand group (152 screws) and the O-arm based navigation group (187 screws) in terms of accuracy. The accuracy rate was 94.1% in the free-hand group and 99% in the O-arm navigated group [12]. However, O-arm navigation has a high cost and requires a high dose of radiation. Another study introduced a miniature robotic guidance system [25]. This technique may be more accurate, be less time consuming, and have less risk of radiation exposure, and it could be applied in the normal vertebra without any deformation. Another investigator introduced the "funnel technique" [7]. It is simple and safe and provides entry-level surgeons with a safe way to identify and place thoracic pedicle screws with no postoperative clinical problems, although it has a risk of screw loosening because of excessive loss of cancellous bone, pedicle fracture, and long operation time.
The free-hand technique is based on the spinal anatomy and harmony of the spinal curve. It requires exposure of the transverse process, which may cause additional muscle injury, blood loss, and time. However, the wide exposure may help young surgeons to better understand the anatomy and spatial array. Furthermore, because it is based on the anatomy, it may enhance the accuracy of PSI as an assisting method when devices are not available or are useless, such as in a highly fatty or osteoporotic patient, in severe scoliosis, and at the cervicothoracic level. Nevertheless, before using this technique, young surgeons must have a thorough knowledge of vertebral anatomy by practicing on several cadavers and by operating under the supervision of an experienced surgeon. During the procedure, young surgeons should follow and use diligent and repetitive confirmatory steps to compulsively assure intraosseous placement.
This study had several limitations. First, this was not a case-controlled study. Screw placement was difficult in the severely deformed spine regardless of using fluoroscope. Certain diagnoses (congenital spinal deformity, scoliosis, and spondylolisthesis) may lead to a greater pedicle breach. During the study period, the number of patients with spinal deformities was small. Repositioning of screws by intraoperative radiograph was not counted among the breaches. Breach rate should be compared according to the diagnosis of the patients.
Conclusions
An analysis by CT scan shows that young spine surgeons can perform PSI with an acceptable breach rate using the free-hand technique, although this does not mean that the free-hand technique is easy. If a spine surgeon has been trained under the supervision of an experienced surgeon and uses repetitive confirmatory steps, even a young surgeon can safely place free-hand pedicle screws.
Notes
No potential conflict of interest relevant to this article was reported.