Quantifying the Amount of Bleeding and Associated Changes in Intra-Abdominal Pressure and Mean Airway Pressure in Patients Undergoing Lumbar Fixation Surgeries: A Comparison of Three Positioning Systems
Article information
Abstract
Study Design
Prospective, randomised controlled, single centre study of 45 patients posted for two level lumbar fixation surgery in the prone position.
Purpose
To compare intra-abdominal pressure (IAP), mean airway pressure mean airway pressure and blood loss during the spine surgery in prone position using three different positioning systems.
Overview of Literature
Studies have correlated IAP with the amount of perioperative bleeding. However, IAP and airway pressures while assessing the bleeding comparing two or more prone positioning systems are unclear.
Methods
This prospective study was conducted on a cohort of 45 patients scheduled for two-level lumbar fixation. Patients were randomly allocated to a spine table, Wilson's frame, and thermomodulated pads. Bladder pressure as an indicator of IAP, mean and peak airway pressures, and blood loss were monitored.
Results
IAP increased whenever patient position was changed to prone .The increase in pressure was more in the Wilson's frame group but was statistically significant only on prolonged positioning. Adopting the prone position always increased the mean airway pressure, but the increased was significant only in the Wilson's frame group. Mean airway pressure decreased in the spine table group and was statistically significant. The blood loss in the spine table group was significantly less as compared to the other groups.
Conclusions
Positioning on a spine table results in less blood loss and low mean airway pressure. The Wilson's frame results in high IAP, increased mean airway pressure, and more blood loss. The thermomodulated frame increases mean airway pressure and produces a moderate increase in IAP and airway pressure.
Introduction
Spinal decompression and instrumented fusion surgeries cause variable amounts of bleeding that can depend on patient positioning. Elevated intra-abdominal pressure (IAP) and airway pressure reflect improper prone positioning [1]. While other factors contributing to higher blood loss, such as blood pressure (BP) and coagulation profile, can be optimised before surgery, IAP elevation is normally a result of improper positioning [234].
Unlike other factors, IAP is not routinely monitored and specialised monitoring systems are rarely available. The correlation between IAP and the amount of perioperative bleeding has been addressed in three studies [256]. The influence of two or more prone positioning systems is unclear.
In this study we compared two newer prone positioning systems with the Wilson's frame system with respect to change in IAP, mean airway pressure (MAWP), and intraoperative bleeding. Few studies have monitored IAP and airway pressure while assessing bleeding in the three different prone positioning systems. We used a monitoring system assembly that is a modification of the technique described in earlier studies [7].
Materials and Methods
1. Patients
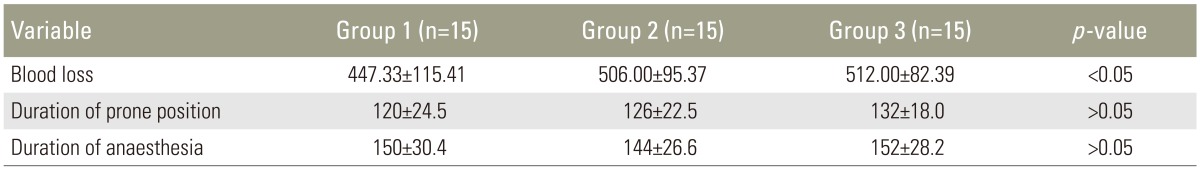
This prospective study was conducted on a cohort of 45 patients 18 to 50 years of age with an American Society of Anaesthesiologists (ASA) physical status I or II who were scheduled for two level posterior decompression and instrumented fusions at L4–5 and L5–S1 as a treatment for degenerative lumbar spine. Patients were excluded if they had a coagulation disorder; were receiving antiplatelet or anticoagulant therapy, even if stopped before surgery; central nervous system, cardiac, liver, or renal disorder; prior spinal, abdominal, or urethral surgery; contraindication to use of transurethral bladder catheter; and etiologies other than degenerative lumbar spine. The included patients were randomly allocated using simple randomisation table to the spine table group (group 1, n=15) (Fig. 1), Wilson's frame group (group 2, n=15) (Fig. 2), or thermomodulated pad group (group 3, n=15) (Fig. 3).
2. Medication and monitoring
All patients were orally medicated with a tablet of alprazolam 0.25 mg the night before surgery and tablets of Ranitidine 150 mg, Emeset 4 mg, and Paracetamol 1,000 mg 1 hour before induction of anaesthesia. Bowel preparation using a proctoclysis enema was done the night before surgery, with no fluid and food intake for at least 8 hours prior to surgery. Routine induction was achieved with an injection of propofol 1.5 mg/kg and fentanyl 2 µg/kg, and muscle relaxation was achieved with an injection of atracurium 1 mg/kg to facilitate intubation. The latter drug was continued at rate of 0.4 mg/kg/hr and adjusted to maintain a post-tetanic count exceeding 8. All the patients were catheterised with an 18-F triple lumen Foley catheter. Parameters that were monitored included bladder pressure as an indicator of IAP, MAWP, peak AWP, blood loss, and vital haemodynamic parameters including like BP in terms of mean arterial pressure (MAP), heart rate, end tidal carbon dioxide (CO2), and electrocardiogram. All the variables were measured at baseline after induction with the patient positioned supine, in the prone position before skin incision, and in the prone position following surgery. When the blood loss exceeded the threshold for maximum allowable blood loss calculated with transfusion trigger at 9 gm%, transfusion with packed blood cells was given. Non-invasive BP monitoring was done using the right arm every 5 minutes. Normotensive status was the goal; noradrenaline or nitroglycerine was injected and continued as necessary to maintain MAP within 10% of the baseline BP.
3. IAP measurement
IAP was measured using a modification of a previously described protocol [7]. A side channel was used to drain urine with a straight channel containing a 10-cm pressure monitoring line connected to a pressure transducer with a three-way stop valve. Before each IAP reading, the drain channel was clamped and 25 mL of normal saline was instilled into the bladder. No movement or external pressure was applied. Measurements were continuous for 20 seconds. Three consecutive readings were taken, with the mean value expressed as mm Hg.
4. BP measurement
BP in mm Hg was measured by summing together as the suction bottle output minus the quantity of saline used for irrigation with the weight of blood-soaked gauze pieces or mops minus the dry weight of the absorbent materials.
Results
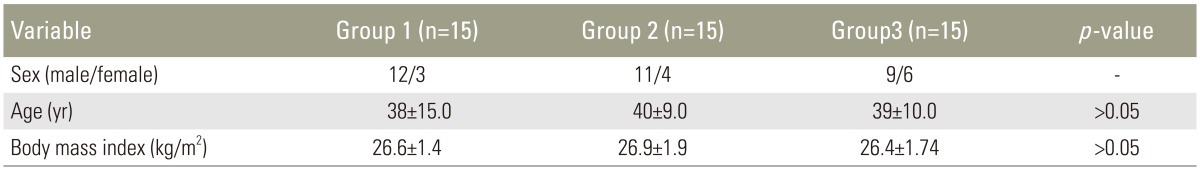
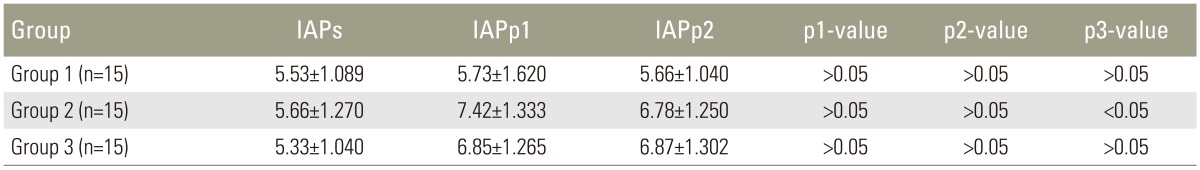
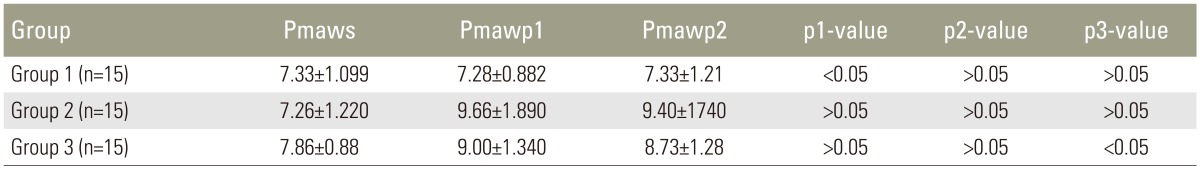
There were no significant differences between the groups in age, sex, weight, body mass index (BMI), duration of surgery, and duration of anaesthesia between the three groups (Table 1). IAP increased in all groups with a position change from supine to prone. The IAP change was more in group 2 from the baseline value of 5.66±1.27 to 7.42±1.333 mm Hg, followed by group 3 (5.33±1.040 to 6.85±1.265 mm Hg) and group 1 (5.53±1.089 to 5.73±1.620 mm Hg). The differences between the groups were not statistically significant. On prolonged positioning, the increase in IAP was statistically significant in group 2 (5.66±1.270 to 6.78±1.250 mm Hg) when compared with the supine position (Table 2). When the prone position was adopted, MAWP increased from 7.26±1.220 mm Hg at baseline to 9.66±1.890 mm Hg in group 2, and from 7.86±0.88 at baseline to 9.00±1.340 mm Hg in group 3. The increase was more substantial in group 2 immediately after adopting the prone position, with a statistically significant increase to 8.73.± 1.28 mm Hg evident in group 3 after a prolonged time in the prone position. In group 1, MAWP decreased from 7.33±1.099 mm Hg at baseline to 7.28±0.882 and 7.33±1.21 mm Hg in group 1, which was statistically significant (Table 3). The blood loss of 447.33±115.41 mL in group 1 was significantly less than in group 2 and 3 (506.00±95.37 and 506.00±95.37 mL, respectively). The durations of anaesthesia and surgical procedure were comparable (Table 4).
Discussion
The desired position for spine surgery should simultaneously provide adequate exposure of the tissues and minimise bleeding [3]. The prone position is ideal for spine surgery, providing adequate vision for the bony and neural structures.
The various positioning systems include frames, kneeling attachments, and special tables. Chest rolls and vacuum pillows are still used as effective and inexpensive methods to obtain a free abdomen. The kneeling position (Eckers position [7]) and the Mohammaden prayer position described over 50 years ago, and the knee chest position [1] described almost as long ago allow considerable flexion of the spine, but are associated with a high incidence of neural and vascular complications.
The Wilson's frame, spine table, and Maquet thermomodulated pad systems have become increasingly popular. Wilson's frame is an expandable radiolucent frame with a pad on each side. The pads can be adjusted laterally to suit the body type of the patient and flexion can be achieved as per the desired lordosis [89]. The spine table is an extension of the surgical table that enables spine surgery with C-arm and O-arm access. The patient is supported at the chest, hip, and head. The crescent-shaped chest pad can accommodate male and female body types. Flexion and extension can be modified intraoperatively. Maquet thermomodulated pads are a set of pads that can be adjusted according to the size of the patient. It is used more often for paediatric patients.
The Wilson's frame is used very frequently for prone positioning and has been extensively studied. In contrast, the other prone positioning systems have seldom been discussed in the literature. A comparison of the Wilson spinal frame and vacuum pillow reported that blood loss was significantly less with the vacuum pillow [10]. But, IAP was not measured.
Presently, we compared the Wilson's frame, spine table, and Maquet thermomodulated pad positioning systems with respect to their effect on IAP, MAWP, and blood loss. A prior comparison of IAP and blood loss of the Wilson's frame in the wide and narrow positions demonstrated significantly less blood loss when a wide frame was used [2]. A positive correlation of IAP and blood loss was also reported. In another study, BMI was reported to affect IAP in the prone position more than in the supine position during lumbar spinal surgery; as well, blood loss increased with IAP in the prone position and with increased BMI [5]. Obese patients were not included in the present study, so cannot comment on the effect of BMI.
Various methods have been described to measure IAP including a monitoring device, rectal pressure monitor, and Foley catheter-based system. The latter is a well-established, relatively simple, and reasonably reliable technique for intraoperative IAP monitoring. IAP monitoring done by connecting the pressure transducer by puncturing the sidewall of the Foley catheter has been described [11]. We modified this technique and used a trilumen Foley catheter. The transducer was attached to the side channel and the whole system was used as a closed assembly throughout the procedure. The amount of saline injected is a contentious issue, with volumes varying widely from 10 to 50 mL. We instilled a 20 mL volume before taking the measurement; this volume has been found acceptable in most studies.
Presently, IAP increased as patients were turned prone. The greater IAP increase in groups 2 and 3 likely reflected the large area of contact at the chest and abdominal area in the two systems. With prolonged positioning the change in IAP became more significant, probably due to the redistribution of blood flow and third space accumulations in the dependent areas of the body. Park while comparing the prior comparison of the narrow and wide Wilson's frame found that pads can compress the abdomen to increase the IAP [2]. The contact area of the Allen spine table was even less when compared to the Wilson's frame in its widest position. This probably resulted in lower IAP in this particular group.
The blood loss in group 1 was also less as compared to the other two groups. The decrease in MAWP was an interesting finding in group 1 and this probably contributed significantly to the reduced blood loss. The spinal table allows unobstructed movement of abdomen and reduces chest compression. The type and duration of surgery was comparable; surgery was less likely to have affected the blood loss. Also, the present study was done at a centre where only a particular set of surgeons perform the surgeries. So, surgeon-related variation in blood loss would not be expected. Also, the study's focus on patients undergoing two-level lumbar fixations further minimised bias and variations.
IAP measurements were taken when the surgeon was not actively performing critical steps. Fluctuations in IAP did occur during screw fixation but were not considered in the interpretation of the results. Since there were variations in IAP, for every reading an average of three readings taken 3 minutes apart was considered.
Active abdominal muscle contractions can result in spurious increase in IAP readings. Therefore, in muscle relaxation was optimised by a post-tetanic count exceeding 8 to avoid any false reading.
A prospective study that evaluated the relationship between airway pressure change due prone positioning [4] concluded that airway pressure increase may predict intraoperative blood loss. In other words, patients with greater increase in airway pressure are likely to bleed more.
Conclusions
The spine table attachment positioning system helps in reducing blood loss. Increases in IAP and MAWP that occur upon adoption of the prone position were reconfirmed. These increases directly predict the amount of perioperative blood loss. Careful patient positioning may eliminate the rise in MAWP secondary to the increase in IAP.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.