The Efficacy of Percutaneous Long-Segmental Posterior Fixation of Unstable Thoracolumbar Fracture with Partial Neurologic Deficit
Article information
Abstract
Study Design
Retrospective analysis.
Purpose
The aim of this study was to evaluate the clinical and radiological outcomes of patients with unstable thoracolumbar fracture (UTLF) who were treated by percutaneous long-segmental posterior fixation (PLSPF) by two vertebrae cranial to the fracture with two vertebrae caudal.
Overview of Literature
To the best of our knowledge, PLSPF for stabilization of UTLF has not been reported.
Methods
The study involved retrospective analysis and investigation from the results of 27 patients who had undergone PLSPF for stabilization of a UTLF with partial neurologic deficit, over a follow-up period of two years. Kyphotic angle (KA), anterior vertebral height percentage (AVHP) and cross-sectional ratio of the displaced fragment within the spinal canal were evaluated with simple radiographs and axial computed tomography scans preoperatively and two years postoperatively. The clinical outcome for pain was assessed by a visual analogue scale (VAS) and Denis' scale, and the degree of neurologic deficit was measured by modified Frankel classification.
Results
Five patients had minor complications. The KA, AVHP, and cross-sectional ratio of the displaced fragment improved significantly after surgery (p<0.001, p<0.001, p<0.003, respectively). Neurologic recovery of one or more for the Frankel grade was seen in 19 patients with an average improvement of 1.7. The VAS and Denis' score improved significantly at a two year follow-up (p=0.02, p=0.012, respectively).
Conclusions
The technique of PLSPF is useful for the treatment of UTLF with partial neurologic deficit, and produces decreased morbidity and fewer complications.
Introduction
The debate over the management regarding unstable thoracolumbar fracture (UTLF) continues, with controversy remaining as to whether non-operative or operative treatment is superior. Additionally, in operative patients, it is controversial whether a posterior or anterior approach is indicated in order to achieve the desired results [1-7]. There are two general methods to prevent the spine from collapsing into kyphotic deformity due to UTLF; direct decompression and instrumentation with fusion through an anterior approach, or indirect decompression by implantation of posterior instrumentation. However, each of these procedures requires extensive exposure of the spine, with prolonged operative times and increased blood loss.
Short-segment pedicle instrumentation (SSPI) is an attractive solution for fast stabilization of vertebral fractures [8-11]. This approach includes pedicle screw fixation at one vertebra above and one vertebra below the fractured vertebra, and can be done percutaneously. Unfortunately, controversy still exists over whether SSPI is a suitable method. Biomechanical and clinical studies pertaining to short segment posterior instrumentation have shown that many cases will eventually fail with weight bearing [12,13]. Recently, several articles reported the efficacy of segmental pedicle fixation two levels above and the one or two levels below the fractured vertebra for stabilization of UTLF, and performed this procedure using wider exposure, which resulted in a large skin incision and massive blood loss.
To the best of our knowledge, there has been no report concerning percutaneous long-segmental posterior fixation (PLSPF) by two vertebrae cranial to the fracture with two vertebrae caudal for stabilizing the UTLF with partial neurologic deficit. The authors would like to describe the outcome of patients with UTLF who were treated by PLSPF.
Materials and Methods
Between January 2008 and May 2010, we retrospectively reviewed the results of 27 consecutive patients who underwent PLSPF for UTLF. A minimum follow-up of 48 months was an essential criterion for inclusion in the study. The extent of the fractures was in the thoracolumbar junction between T11 and L2. Following a routine examination and X-ray of the spine, computed tomography (CT), and magnetic resolution images (MRI) were carried out. The inclusion criteria of this study were 1) intact or partial neurological injury caused by the fracture; 2) instability criteria of kyphotic deformity with radiological assessment of kyphotic deformity of more than 20 degrees and/or vertebral body height loss of more than 50% compared to the vertebral below; 3) cross-sectional ratio (CSR) of displaced vertebral fragment into the spinal canal less than 50%; 4) a minimum follow-up of 48 months. The exclusion criterion is the following: 1) complete neurologic deficit caused by the fracture; 2) CSR of displaced vertebral fragment into the spinal canal of more than 50%; 3) a follow-up period of less than 2 years.
The degree of neurologic injury was evaluated by the modified Frankel classification preoperatively, one month, six months, and two years postoperatively as well as a final follow-up period. The clinical results were obtained by a medical record review, and patient interviews using Frankel's grade system for assessment of neurological deficit [14]. Also, pain and work status at the latest follow-up were recorded based on the scale of Denis et al. [15]. This is a five-level scale ranging from no pain (P1) to constant, severe pain (P5), and from return to heavy labor (W1) to completely disabled (W5).
To assess the radiological results, kyphotic angle (KA) and anterior vertebral height percentage (AVHP) were evaluated with simple lateral radiographs both preoperatively and at a two year follow-up. KA was defined by the modified Cobb's method, which measures the angle between the upper endplate and the lower endplate of the fractured vertebra. AVHP was defined by the ratio method (the anterior height of the fractured vertebra/the mean anterior vertebral height of the adjacent upper and lower vertebra of the fractured vertebra). The CSR of the displaced fragment occupying the spinal canal was measured by an axial CT scan both preoperatively and at two years postoperatively, and the change of canal encroachment was evaluated. The reduction degree of the fractured fragment was defined as the difference of the displaced fragment between preoperative and two years postoperatively.
1. Surgical technique
The patient was placed in the prone position, lying flat on the table, and verification that adequate fluoroscopic images of the pedicles could be obtained in both anterior-posterior (AP) and lateral views was confirmed before proceeding. Following the induction of general anesthesia, the patient was in the prone position with cushions under the iliac crests and thorax in order to prevent pressure on the abdominal region. This was done so that the spine was in a hyperextended position. Postural reduction was then performed.
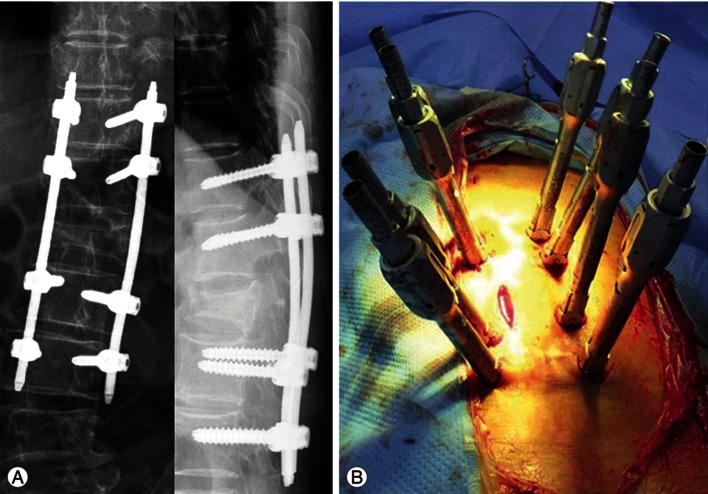
We used the CD Horizon Longitude system (Medtronic, Sofamor Danek, TN, USA). Fluoroscopic images were obtained in the AP and lateral planes to ensure that the pedicles could be adequately visualized. The entry points for the pedicle screws that were to be fitted with instrumentation were then chosen. An incision of approximately 15 mm was made at the skin entry point and extended into the underlying subcutaneous tissue. A guide wire was used to perforate the fascia, and a series of sequential dilators were then used to dilate the fascia in order to bluntly separate the underlying paraspinous muscles until the spine was exposed. The dilators were removed, and both a tracked awl and a pedicle probe were used to create a pedicle pilot hole under C-arm fluoroscopic guidance (Fig. 1). The chosen pedicles were then tapped and screws were placed. These angles were judged using preoperative CT or MRI of the thoracolumbar region. The axial angulation of the instrument was adjusted until the pedicle access kit needle was visualized within the boundaries of the pedicle on the AP view but lateral to the medial pedicle. After pedicle screws, together with their attached extenders, had been inserted, a longitude rod was placed by the rod placement system with distraction force. In this manner, bilateral pedicle screws were inserted into the two pedicles above, the pedicle of fracture site, and two below the fractured vertebra. All steps of pedicle fixation were performed under C-arm fluoroscopic image guidance. A postoperative plain film was obtained, which revealed satisfactory fixation in our study (Fig. 1). Any bleeding within the wound was controlled with bipolar forceps, and fascial and skin incisions were sutured. Of note, a drainage tube was not placed in the wound.
2. Postoperative care
An antibiotic drug was routinely used for five to seven days after the surgery. The glucocorticoid, dehydrating, and neurotrophy agents were properly used to relieve nerve edema and accelerate neurofunctional rehabilitation in neurodeficient patients during the first week postoperatively. Patients were encouraged to do some out-of-bed activities with a thoraco-lumbo-sacral orthosis brace beginning two or three days after operation and continuing to do so for three months postoperatively. Over-activity and weight loading should be avoided for six months after the operation. Furthermore, X-ray imaging should be taken regularly.
3. Statistical analysis
SPSS software package ver. 19.0 (SPSS Inc., Chicago, IL, USA) was used to perform the statistical analysis and the level of significance was set at a p-value <0.05. Continuous variables were compared using paired t-tests.
Results
1. Patient characteristics, surgical procedures, and general surgical outcomes
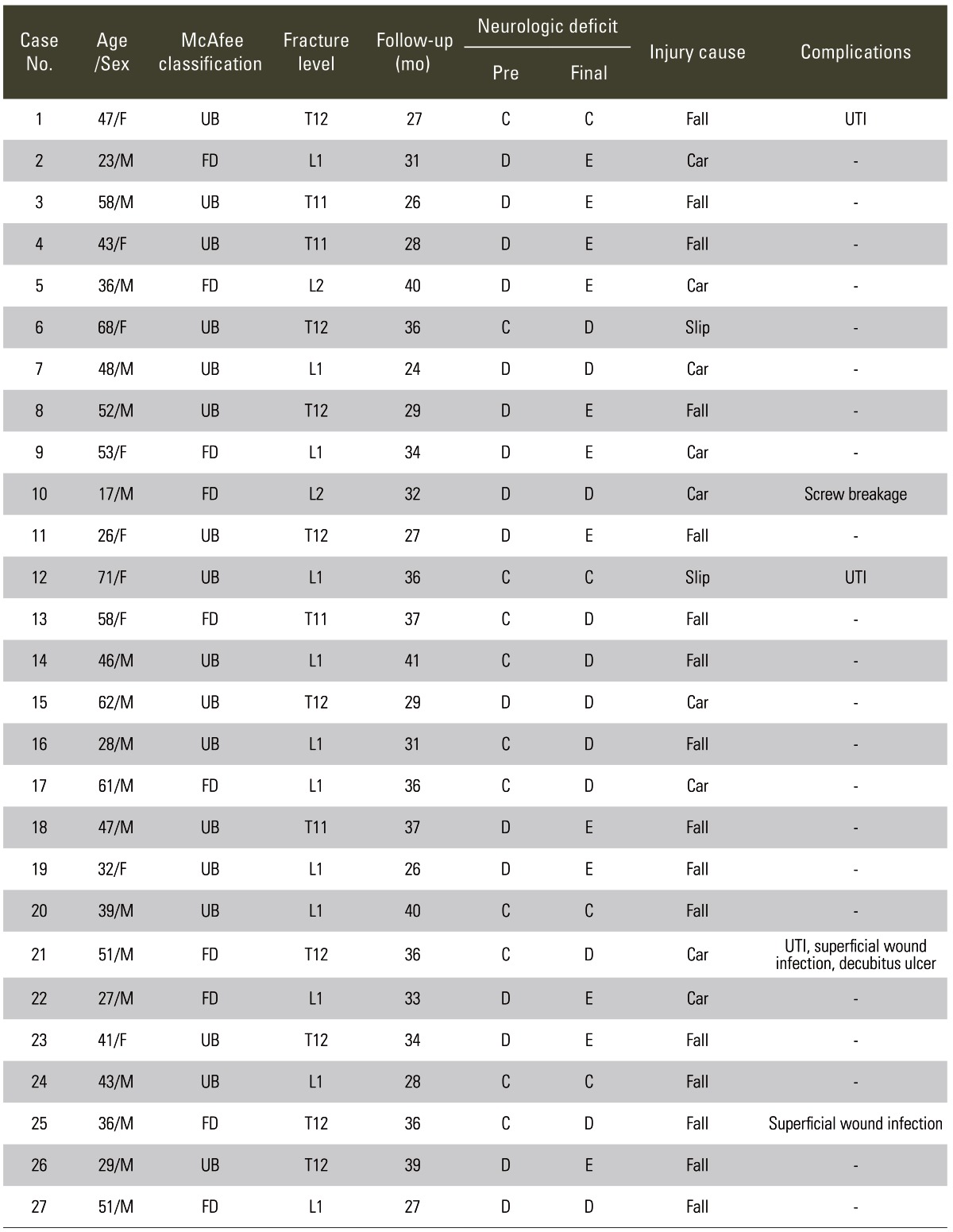
This study included 17 men and 10 women, with an average age of 42.3 years (range, 17-70 years). The patients were admitted to the hospital one to four days after injury (average, 1.6 days), and operations were performed between one and six days (average, 1.9 days) after the initial trauma. The mean duration of the follow-up was 32.1 months (range, 24-41 months). The causes of injury included: fall (16 patients), car accident (9 patients), and slip (2 patients). The levels of fractured vertebra were T11 (4 patients), T12 (9 patients), L1 (12 patients), and L2 (2 patients). McAfee's classification of the spinal fracture was used to classify the UTLF, which included 17 with unstable burst fractures and ten with flexion-distraction injuries. The mean operative time was 72.8 minutes (range, 50-110 minutes), and average blood loss during operation was 60 mL (range, 50-100 mL) (Table 1).
2. Radiological results
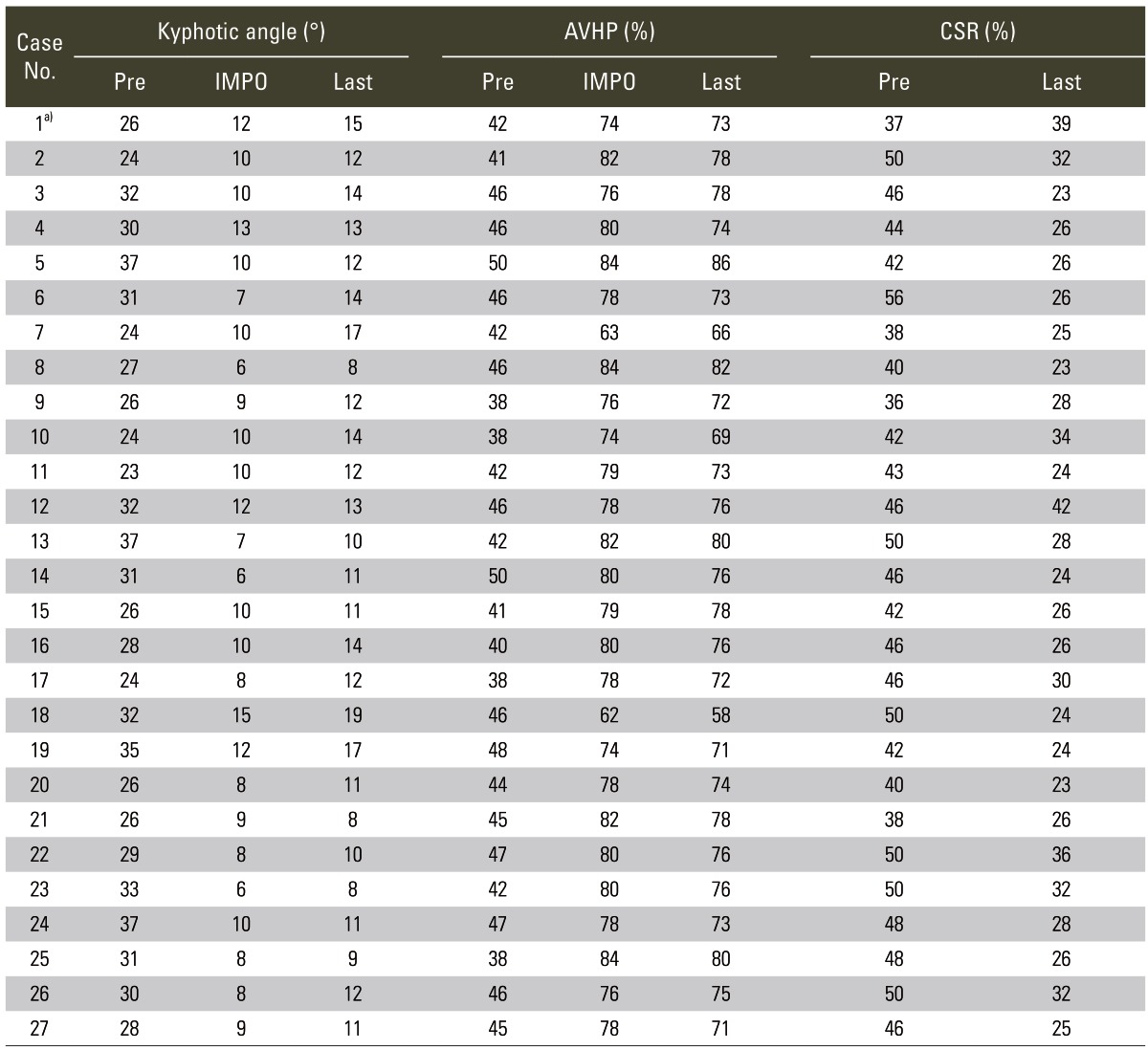
The mean KA was assessed as 28° (range, 23°-37°) preoperatively, compared to 9.3° (range, 6°-15°) one week postoperatively, and 13° (range, 7°-19°) two years postoperatively. Correction rate of KA was on average 75% (range, 63%-92%) one week postoperatively, and the mean loss rate of corrected KA during a two year follow-up was 12% (p<0.001, p<0.001, respectively). The mean AVHP was 46% (range, 38%-50%) preoperatively to 79% (range, 62%-86%) in the immediate postoperative period, and 73% (range, 58%-86%) at two years postoperatively (p=0.012, p=0.016, respectively). The mean correction rate of AVHP was 35% after surgery, and the mean loss of correction during a two year follow-up was 7%. The changes of KA and AVHP were statistically significant (p=0.002, p=0.0014, respectively).
The CSR of the displaced fragment in the axial CT scan was 48.8%±11% preoperatively to 34.4%±11.2% at two years postoperatively, and the change of ratio was statistically significant (p<0.001). In one case regarding a T12 unstable burst fracture with a mild neurologic deficit, the extent of the displaced fragment was increased from 37.1% preoperatively to 39.0% at two years postoperatively. However, neurologic deterioration had not occurred, and mild neurologic symptoms and signs were completely recovered after a one year follow-up (Table 2).
3. Clinical results
Neurologic recovery of a Frankel grade of one or more was seen in 19 patients with an average improvement of 1.7 (range, 0-3). Of the 22 patients exhibiting a partial neurological deficit, two grades of improvement were observed in ten patients and one grade of improvement was found in 12 patients. The mean Denis' pain scale was measured as 7.2 (range, 6.8-7.6) preoperatively to 3.4 (range, 3.2-3.7) at one week and 1.6 at two years postoperatively. Summarized data regarding clinical results is described in Table 1.
Based on the pain scale of Denis, 13 patients (48.1%) had no pain (P1); 12 patients (44.4%) had slight pain with no need for medication (P2); 1 patient (3.7%) had moderate pain with a need for medication but no interruption of work or major change in activities with regards to daily living (P3); and 1 patient (3.7%) had moderate-severe pain with a need for frequent medication and occasional absence from work or a major change in activities regarding daily living (P4). Postoperative work status was assessed as follows: return to previous activity (16 patients, 59.2%), return to less strenuous work (9 patients, 33.3%), disability after the injury (1 patient, 3.7%), and unemployed before the injury (1 patient, 3.7%). No patient had constant or severe incapacitating pain and a chronic need for medication.
4. Complications
Five patients had one or more complications. There was one case of hardware failure involving screw breakage; however, bone healing was achieved without other complications. After the fracture site healed, posterior instrumentation was removed. No neurological complication due to instrumentation was observed in any patient. Three patients with a preoperative neurological deficit had urinary tract infections and required antibiotics. Two patients with superficial wound infections responded to antibiotics and antiseptic dressings. One patient with decubitus ulcer required plastic surgery (Table 1).
Discussion
PLSPF is an appropriate method for achieving stable fixation of UTLF. This study shows that this technique is safe and offers improved construct stability in the treatment of UTLF.
SSPI is an attractive solution for fast stabilization of vertebral fractures. Transpedicular, short segment fixation became popular after the introduction of transpedicular screws by Roy-Camille et al. [10] and the internal fixator by Dick et al. [11]. This approach includes pedicle screw fixation at one vertebra above and one vertebral below the fracture, and it can be done percutaneously in less than 1.5 hours. It is also associated with minimal blood loss and early ambulation. Unfortunately, controversy still exists over whether SSPI is a suitable method. Biomechanical and clinical studies have shown that when there is loss of more than 50% of the vertebral body height or angulations of the thoracolumbar junction of more than 20°, acute spinal instability results. Subsequently, the spinal segment will eventually fail with weight bearing [2,16]. Biomechanical studies have also shown that spinal instability results when there is a failure of at least two of three columns. Krag [17] has suggested segmental pedicle fixation two levels above the kyphosis in order to prevent implant failure. Carl et al. [18] reported that segmental transpedicular fixation two levels above the kyphosis should be used at the thoracolumbar junction where compressive forces act more anteriorly and that no implant failure occurred with the use of the one above-one below construct. Also, posterior instrumentation by two vertebrae cranial to the fracture with one or two vertebra caudal is generally accepted [1-2,6,7,16,19,20]. In addition, several authors suggested that the placement of the pedicle screw into the fractured vertebral body generates a segmental construct, which demonstrated improved biomechanical stability compared with a non-segmental construct [21-23]. A biomechanical study in a cadaveric model also demonstrated that the axial torsion stability improved by two-folds, and there are trends toward increased stability in flexion-extension, as well as lateral bending [13]. However, some problems require long-segmental posterior fixation; 1) wider exposure, 2) increasing blood loss, and 3) higher morbidity. The authors thought that if long-segmental fixation is possible to be a percutaneous method, it is a safer and more effective method compared to conventional long-segmental fixation.
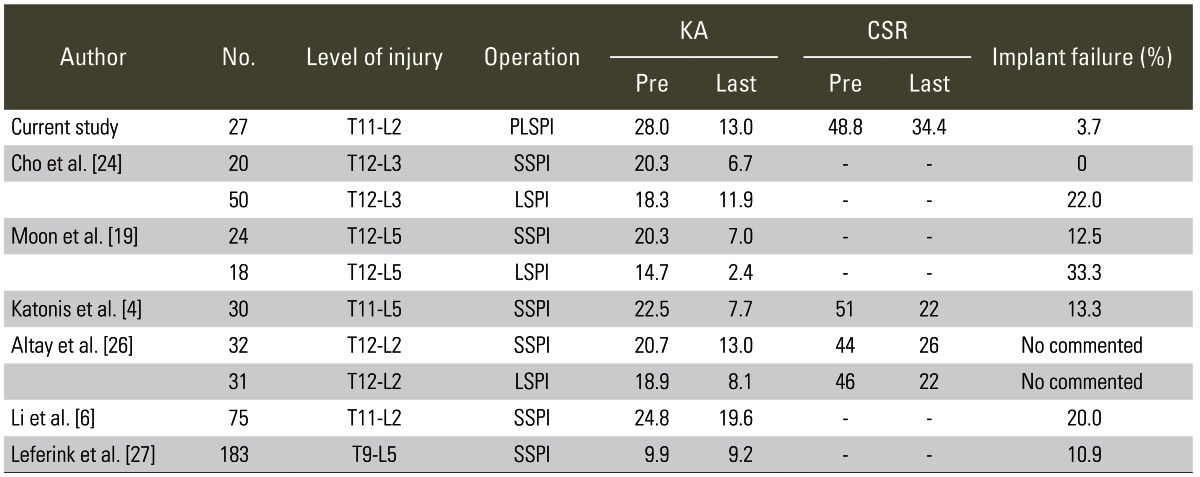
Radiologically, an average of 19° of kyphosis correction could be obtained using percutaneous 2-1 segmental fixation with the pedicle screwed into the fractured vertebra during the follow-up period of two years. This is likely better than traditional, non-segmental pedicle screw fixation [23]. Carl et al. [18] reported 7° of initial postoperative kyphosis correction, while Cho et al. [24] achieved 6° of correction. Similarly, McNamara et al. [25] reported a 9° loss of initial kyphosis correction using nonsegmental fixation techniques. In addition, this is likely better than short-segmental pedicle instrumentation. Mahar et al. [22] reported 15° of initial kyphosis correction. And, postoperative correction loss after posterior short-segmental fixation has been reported by many authors (Table 3). In our retrospective review of 27 patients, radiographs over a two year follow-up revealed an average loss of 4.7° regarding kyphosis correction, resulting in a kyphosis correction of 19° at two years postoperatively.
Published literature regarding short-segmental or long-segmental posterior fixation of unstable thoracolumbar fracture
The most important issue of posterior fixation with indirect reduction is that this technique does not create a sufficient reduction of the displaced fragment into the spinal canal and is not enough to make a satisfactory canal remodeling due to insufficient strength, especially in the case of SSPI [12-13]. However, in recent studies, objective opinions regarding this limitation whereby this posterior fixation with indirect reduction could make a sufficient reduction of the fragment have been raised, if more stable and powerful posterior fixation is possible (Table 3) [14,27-30]. In addition, McCormack et al. [28] described load-sharing classification to identify which UTLF are likely to have poor anterior load-bearing capabilities resulting in correction loss and implant failure. In those instances, they recommended either a long segment posterior fixation or two-stage anterior and posterior procedures. In this study, satisfactory canal clearance and remodeling was shown by our surgical technique of PLSPF. The authors thought that PLSPF could have better canal clearance and remodeling because our technique creates a more stable fixation with less progressive kyphotic change compared to SSPI.
The single known hardware failure in our study, screw breakage, was identified to be at one year postoperatively, but bony healing was achieved without other complications. Others studies regarding SSPI reported that 3% to 5% of cases have hardware failure, some of which result in improper healing of spinal structures and aggravated kyphotic deformity. Other complications, except superficial infection, did not occur. It is important to note that this surgery produced adequate stability for injured spine structures and fewer complications than SSPI or conventional instrumentation.
In general, in the case of neurologic deficit after burst fracture of the thoracolumbar area, anterior decompression and fixation is mainly performed. However, this procedure is very technically demanding with massive blood loss and high morbidity. The authors performed just the posterior instrumentation with reduction using ligamentotaxis, and the result of a 2 year follow-up showed an average reduction of 34% regarding CSR and improvement of neurologic deficit in 19 cases. Thus, the authors suggested that just PLSPF with ligamentotaxis is also a useful method for UTLF with partial neurologic deficit. Furthermore, we are going to bring out the comparative study of anterior decompression and fusion versus posterior long-segmental fixation in UTLF with partial neurologic deficit for some indications.
This study has two primary limitations. First, the number of patients available for follow-up is small. The research team is currently considering both increasing the patient sample size as well as the duration of the follow-up. The second is the lack of dual-energy X-ray absorptiometry scan information. Thus, it is unclear if osteoporosis had a significant effect on bony union and clinical or radiological results. The third limitation would be potential differences in patient positioning when the radiographs were taken. We acknowledge this, but state that the best attempts were made to position the patient in a consistent manner, both in the acute setting and follow-up visits. In addition, the measurements were made by the same spine fellowship-trained reviewer to reduce variability in the data.
Conclusions
To date, the results of patients surgically treated by PLSPF for UTLF with partial neurologic deficit have not been reported. The authors believe that this technique may be useful for treatment of UTLF with partial neurologic deficit, canal encroachment less than 50% of the spinal canal. Additionally, this technique has advantages such as decreased postoperative morbidity and fewer complications compared with conventional long-segmental posterior fixation or anterior instrumentation.
Notes
No potential conflict of interest relevant to this article was reported.