Lumbar Epidural Varix Mimicking Perineural Cyst
Article information
Abstract
Lumbar epidural varices are rare and usually mimick lumbar disc herniations. Back pain and radiculopathy are the main symptoms of lumbar epidural varices. Perineural cysts are radiologically different lesions and should not be confused with epidural varix. A 36-year-old male patient presented to us with right leg pain. The magnetic resonance imaging revealed a cystic lesion at S1 level that was compressing the right root, and was interpreted as a perineural cyst. The patient underwent surgery via right L5 and S1 hemilaminectomy, and the lesion was coagulated and removed. The histopathological diagnosis was epidural varix. The patient was clinically improved and the follow-up magnetic resonance imaging showed the absence of the lesion. Lumbar epidural varix should be kept in mind in the differential diagnosis of the cystic lesions which compress the spinal roots.
Introduction
Lumbar epidural varices are enlarged venous structures located around the dura mater of the spinal cord. They have been infrequently described in the literature and are rarely accepted as a primary pathophysiological entity [1]. These lesions usually mimick lumbar disc degenerations and herniations [2]. The possible mechanism is the obstruction of the anterior epidural venous flow leading to anterolateral caudal venous distention. Subsequent venous endothelial injury predisposes the patient to varying degrees of thrombosis [3]. Magnetic resonance (MR) imaging characteristics of the epidural varix depend upon the degree of thrombosis within this anomaly. A thrombosed varix is hyperintense on T1-weighted, proton-density, and T2-weighted images, whereas flowing blood is hypointense [4]. The variable hypointensity and hyperintensity on the T2-weighted MR imaging sequences correlates with a partially patent lumen within the varix. The treatment is decompression of partially thrombosed varices by discectomy or coagulation of the varices with bipolar cauter [1,2,5].
We reported a case of lumbar epidural varix presented with radiculopathy and mimicked a perineural cyst. The differential diagnosis of this lesion is discussed with a review of the literature.
Case Report
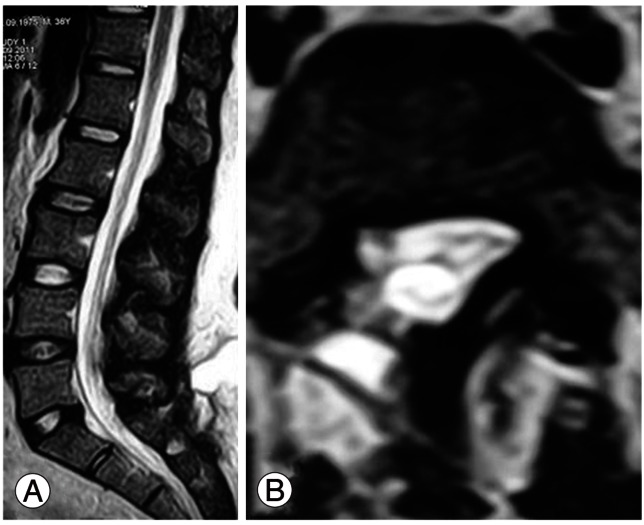
A 36-year-old male patient presented to our hospital with right leg pain. He was healthy otherwise. In his neurological examination, mild motor weakness was detected on the plantar flexion of the right foot, as well as absence of the achille reflex on the right side. The MR imaging revealed a hyperintense cystic lesion at the S1 level with compression on the right spinal root and dural sac (Fig. 1). The radiological diagnosis was perineural cyst. The patient underwent surgery and right L5-S1 hemilaminectomy was performed. A brown-soft mass lesion, which was in connection with the epidural venous plexus, was identified during surgery (Fig. 2A).
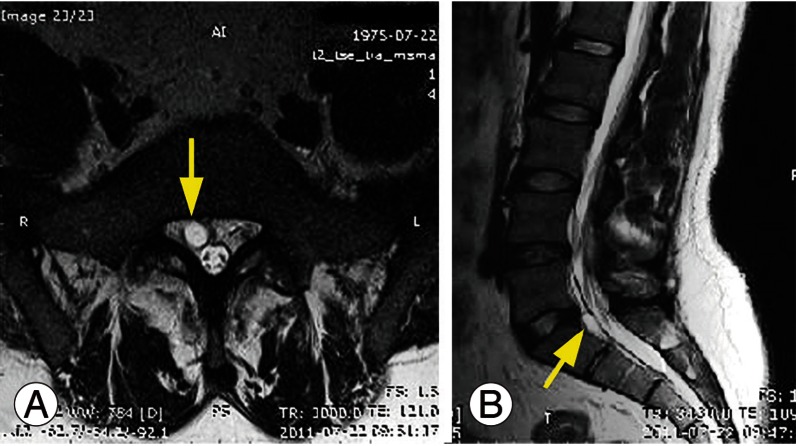
Preoperative T2-axial (A) and T2-sagittal (B) magnetic resonance imaging show hyperintense cystic lesions compressing the right spinal root. The yellow arrow shows the lesion.
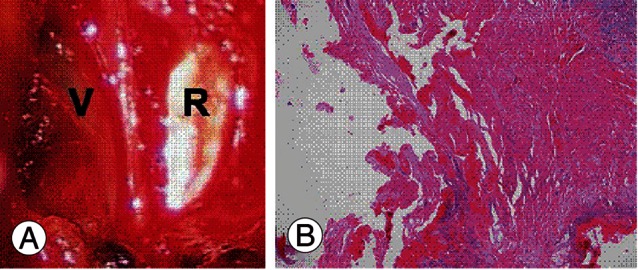
(A) Intraoperative view of the epidural varix (V), which compressed the spinal root (R) above the sacrum. (B) Large and tortuous vessels were seen in the histological examination (H&E, ×100).
This lesion became smaller after coagulation and was removed after cutting the connections with epidural plexus. No massive bleeding occured during the resection of the lesion. The spinal root and dural sac were decompressed. The histological examination of the lesion showed tortuous and dilated vessels that were consistent with the diagnosis of varix (Fig. 2B). The patient was clinically improved after surgery. The postoperative MR imaging at the third month after surgery showed the absence of the varix (Fig. 3).
Discussion
We report a case of lumbar epidural varix which cause radiculopathy and mimicks perineural cyst in MR examination. The patient was treated surgically and improved clinically in 3 months. Epidural varices in the lumbar spine are acquired lesions that are caused by dilation of the internal vertebral venous plexus [1,2]. They are often accompanied by dilation of intervertebral veins and external vertebral venous plexus. The pathophysiological basis of epidural varices is not well known, but there are some speculations [1-3]. A herniated disc material may occlude an epidural vein; subsequently venous dilatation can occur as a result of the valveless nature of the epidural venous plexus [5]. In addition, portocaval hypertension, thrombosis of the inferior vena cava and agenesis of infrarenal segment of inferior vena cava may be responsible for the development of lumbar epidural varix [5-7]. In our case, we performed MR-venography after the operation, but could not find any obstruction or agenesis in the inferior vena cava. There was no disc herniation in our case, which meant that the occlusion of epidural vein by a herniated disc material was impossible. Based on these observations, it seems that the varix was idiopathic in our case.
The varices in the epidural spaces or in the intervertebral foramina may cause irritation or compression on the thecal sac and spinal roots, which results in radiculopathy [1-3]. Clinical manifestations of epidural varices may be caused by two mechanisms: 1) compression of the thecal sac and the nerve roots by the dilated veins or irritation of the roots by the dilated veins; and 2) high pressure in the epidural veins that is transmitted to the perimedullary veins draining the spinal cord and the nerve roots [5]. In our patient, the varix compressed on the spinal root and caused radiculopathy. The patient improved after decompression of the root. MR imaging is a gold standard for the diagnosis. The epidural veins could not be visualized on MR studies under normal conditions. Routine MR techniques demonstrated epidural varices, in their maximum manifestation, as zones of a signal void, which repeated the contours of particular veins and the main epidural venous pathways (of anterior and, less often, posterior longitudinal veins, intervertebral veins, and conglomerates of veins). MR imaging seldom shows dilated intervertebral veins causing nerve root compression [5]. In our case, the lesion was hyperintense in T2- and hypointense in T1-weighted MR slices. There was no contrast enhancement on the lesion after intravenous gadolinum administration. This was related to very slow venous flow and thrombosis.
The differential diagnoses of lumbar epidural varices include herniated disc, abscess, tumor, hematoma, and synovial cyst [1,2,5-9]. The varices are sometimes indistinguishable from a sequestered disc fragment [2]. Perineural cysts have not previously been reported in the differential diagnosis of epidural varices. In our case, the MR imaging findings, however, are more consistent with perineural cysts than a thrombus and/or slow blood flow within the epidural varix. Hanley et al. [3] divided the epidural varices into 3 types. Type 1 is thrombosed dilated epidural vein, type 2 is epidural vein dilation due to activity and type 3 is submembraneous epidurally-contained hematoma. Our case was type 1 according to Hanley's classification.
Surgery is the main treatment of lumbar epidural varices. However, Tofuku et al. [10] reported a case of lumbar epidural varix at L3 level which was spontaneously regressed within 2 weeks. They did not perform surgical treatment. The choice of surgical method depends on the type of varix and clinical manifestations [5]. The aims of the surgical intervention are the decompression of the thecal sac and nerve roots, and elimination of the irritation. Complete interruption of the blood flow in the epidural veins should be avoided during surgery because these veins are the only channels of collateral blood flow [5]. In our case, we did not remove all of the epidural veins, but we disconnected the varix from the venous plexus and then removed it successfully after coagulation.
To conclude, lumbar epidural varix is a specific lesion of the spinal canal. The diagnosis is difficult, but the treatment is unique. Perineural cysts should be kept in mind in the differential diagnosis. A precise diagnostic workup and well-planned surgery will lead to a successful outcome.
Notes
No potential conflict of interest relevant to this article was reported.