Surgical Treatment of T1-2 Disc Herniation with T1 Radiculopathy: A Case Report with Review of the Literature
Article information
Abstract
The prevalence of intervertebral disc herniation (IDH) of the thoracic spine is rare compared to the cervical or lumbar spine. In particular, IDH of the upper thoracic spine is extremely rare. We report the case of T1-2 IDH and its treatment, with a literature review. A 37-year-old male patient visited our hospital due to radiating pain at the left upper extremity and weakness of grip power. In cervical spine magnetic resonance images, T1-2 disc space showed herniated disc material and compressed T1 root was identified. Laminoforaminotomy was performed with a posterior approach. The radiating pain and weakness of grip power improved immediately after the surgery. Of patients who show radiating pain or numbness at the medial aspect of forearm, or weakness of intrinsic muscle of hand, can be suspected to have T1 radiculopathy. A detailed physical examination and a radiologic evaluation including this area should be required for the T1 radiculopathy.
Introduction
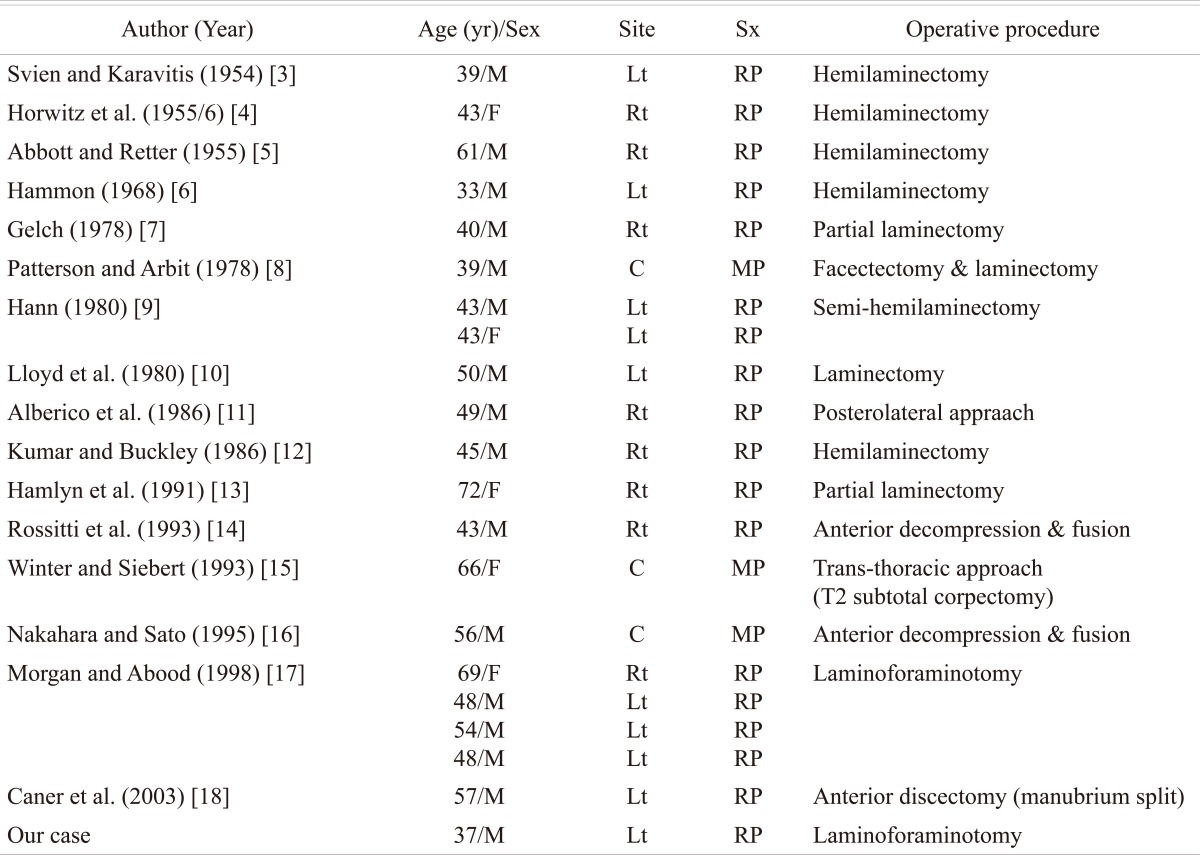
The prevalence of intervertebral disc herniation of the thoracic spine is rare compared to that of the cervical or lumbar spine. In particular, intervertebral disc herniation of the upper thoracic spine is extremely rare [1,2]. Since Svien and Karavitis [3] reported one case in 1954, 39 cases of T1-2 disc have been reported to date, of which 19 cases had no individual description as they were included with reports on thoracic disc herniation, and 20 cases had descriptions of each case and surgical treatment as they were case reports (Table 1) [3-18]. In some of the aforementioned cases, the diagnosis and treatment of the disease was delayed as patients were misdiagnosed with medical diseases or other spinal diseases in the early diagnosis. In the present report, the patient was also misdiagnosed with other level intervertebral disc herniation in the early diagnosis, but he was shown to have T1-2 herniated nucleus pulposus (HNP) during the treatment. Accordingly, the authors report this case with a literature review.
Case Report
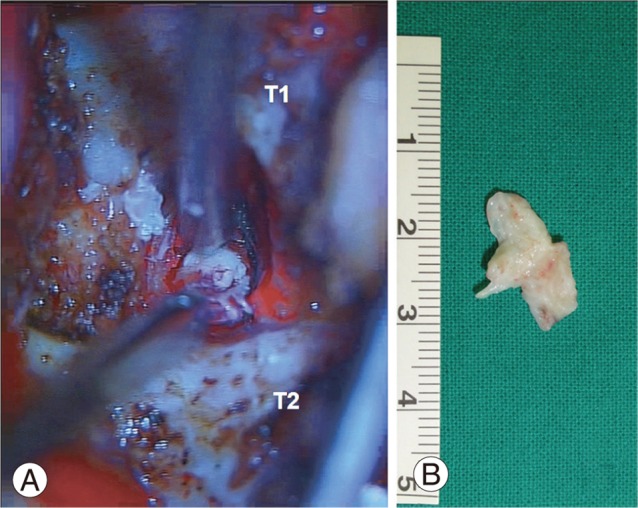
A 37-year-old male patient visited our hospital due to radiating pain at the left upper extremity and weakness of grip power. The symptoms of the patient occurred five days before the visit without particular trauma history. The patient underwent conservative management including medication at a local clinic, but the symptoms were aggravated. A physical examination showed pain at the left scapular area, radiating pain at the medial aspect of forearm and at the fourth and fifth fingers, approximately 70% of sensory loss compared to the unaffected side, decreased left hand grip power with motor grade IV, and positive Spurling sign. No myelopathic symptom and Horner's syndrome such as ptosis, enopthalmus, and anhydrosis were observed. No difference in biceps jerk and triceps jerk was found between the affected and unaffected sides. No pathologic reflex such as Hoffmann sign and inverted radial reflex was found. Cervical spine simple radiographs examination showed no particular finding except mild kyphosis. The patient was suspected to have disc herniation of the cervical spine, and underwent cervical spine magnetic resonance images (MRI). The MRI examination showed mild neural compression at the left C6-7 foramen. Subsequently, selective nerve root block on left C7 was performed for both diagnosis and treatment. After the selective nerve root block, the patient showed almost no improvement of the symptoms. After detailed review of the MR images, herniation of intervertebral disc on T1-2 level was suspected at the distal end of images. Rechecked MRI on this area showed intervertebral disc herniation that compressed T1 root (Fig. 1). As the patient suffered from severe radiating pain with weakness and numbness, a surgical treatment was planned. As the disc was extruded to the posterolateral side, and no compression of the spinal cord was found, decompression surgery via a posterior approach was planned. Laminoforaminotomy was performed with prone position and we could remove the subligamentous disc that compressed T1 root (Fig. 2). Most symptoms of radiating pain and weakness improved immediately after the surgery. The patient recovered without any complication for six months after the surgery.

Preoperative T2 sagittal (A, B) and thin section T1 and T2 axial (C, D) magnetic resonance images on T1-2 disc level show the ruptured disc fragment (arrows) with distal migration.
Discussion
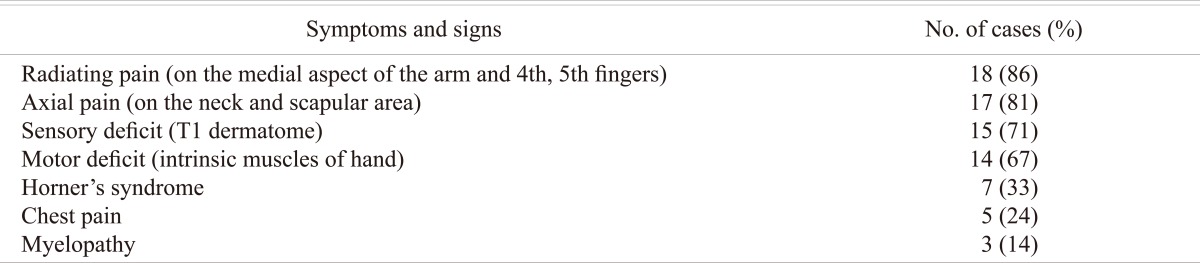
Herniation of intervertebral disc or stenosis rarely occurs at T1-2 level. This area is generally obscured by the shoulder in X-ray examination, and commonly located at the caudal end in computed tomography (CT) or MRI examination. Thus, it is difficult to observe this area carefully. Accordingly, when this area has a lesion, it is frequently misdiagnosed with medical diseases or other level herniation of intervertebral disc as shown in this case, and sometimes, it is identified during the treatment [11]. In the case of T1-2 disc herniation, spinal cord or T1 root compression occurs. T1 root is a root comprising the brachial plexus, and constitutes the ulnar nerve along with C8 root. Thus, T1 radiculopathy may accompany numbness of the fourth and fifth fingers, or weakness of intrinsic muscle of hand as similar to C8 radiculopathy. As symptoms similar to the aforementioned symptoms may be observed if the entrapment of the peripheral nerve, such as cubital tunnel syndrome or Guyon's tunnel syndrome, it is important to correctly identify the lesion location. According to previous reports, radiating pain at medial aspects of the forearm and at fourth and fifth fingers, and axial pain at the neck and periscapular area were reported to occur with a frequency of 86% and 81%, respectively, for T1-2 disc herniation (Table 2). T1 radiculopathy may accompany Horner's syndrome. In this case, level of neural compression can be more easily predicted, but diseases such as pancoast tumor and intrathoracic neoplasm should be ruled out [10]. Although upper thoracic disc herniation has been known to rarely occur, but relatively commonly occur at T1-2 level among the upper thoracic levels [17,19]. The literature review showed that a majority of patients had only radiculopathy, and underwent laminectomy or foraminotomy via a posterior approach, and achieved a good outcome [3,10,17,19]. Taken together, successful treatments were achieved using posterior laminotomy and/or foraminotomy in 17 (81%) out of 21 cases. Meanwhile, an anterior approach was applied in four cases (19%) showing myelopathy due to the compression of the spinal cord by central disc herniation. Some studies reported that successful treatments were achieved using Southwick-Robinson approach without sternotomy, but others reported that partial sternotomy was required [14,16,18]. Therefore, when a surgical treatment using an anterior approach is planned, the relationship between the sternum and T1-2 level should be considered before surgery, and an appropriate procedure should be prepared if sternotomy is required.
T1-2 level is a region that is not observed closely in cervical spinal radiographs or MRI. Of patients who show radiating pain or numbness at the medial aspect of the forearm, or weakness of the intrinsic muscle of the hand, those who have non-typical results in physical examination, or who had an effect less than expected after selective nerve root block on the lower cervical spine are suspected to have T1 radiculopathy. A delicate physical examination and a radiologic evaluation including this area and treatment plan are required for the aforementioned patients.