Introduction
Spinal epidural hematomas (SEHs) are rare but classic complications of lumbar disc surgery [1-4]. They are believed to originate from the venous plexus of the epidural space and are generally limited to the surgical site [5]. SEH must be suspected systematically in postoperative spine patients with acute symptoms of neurologic deterioration. An emergency surgical intervention is usually required. The most appropriate procedure, especially when the SEH extends beyond the initial surgical exposure, is not known. In such cases, a laminectomy extending as far as the SEH is generally performed [5]. We present a case of an extensive SEH from T11-L5 following a L3-L4 discectomy that presented with bilateral L4 radiculopathies at 8 hours postsurgery.
Case Report
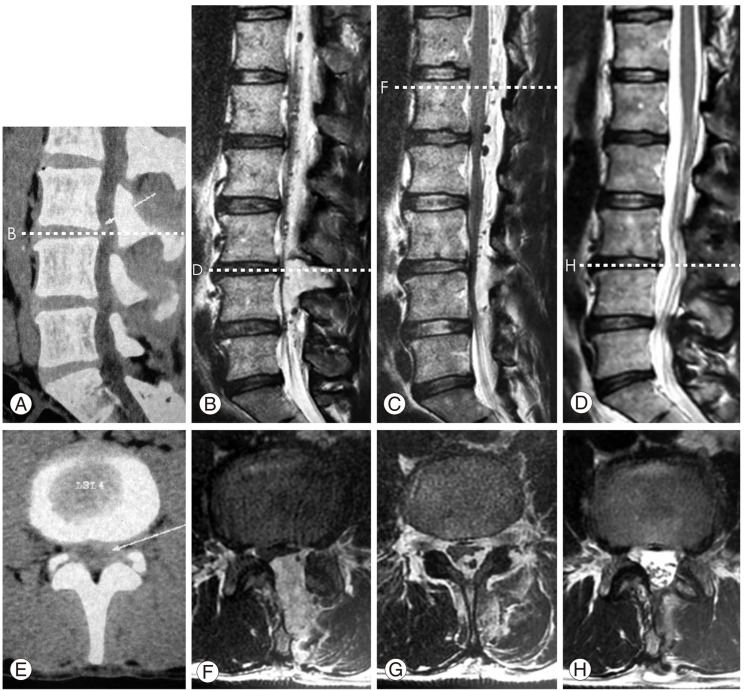
A 46-year-old man, employed as a bricklayer, presented with a chief complaint of progressive left lower limb radiculopathy (visual analog score, VAS; 6/10) of two months duration. The patient's past medical history was unremarkable, especially with no use of aspirin or anticoagulant drugs and no known comorbidities (hypertension, vascular problems, diabetes, or coagulopathy). On physical preoperative examination, he showed a mild hypoesthesia in the left L4 dermatome. There was no bladder or erectile dysfunctions, and motor examination was normal. Radiographs of the lumbar spine did not reveal any significant abnormalities. Computed tomography of the lumbar spine demonstrated a left L3-L4 paramedian disc herniation (Fig. 1A and 1B). Lumbar resonance magnetic imaging was not performed.
The patient underwent a L3-L4 conventional microdiscectomy associated with a left L4 foraminotomy using a left intermyolaminar approach combined with a left interlaminar window in the genupectoral position under general anaesthesia. There was minimal blood loss, and no cerebrospinal fluid (CSF) leak was noted during surgery. No drain was inserted. At 2 hours postsurgery, the patient noted a complete resolution of the left L4 radiculopathy (VAS 1/10). At 8 hours postoperative, the patient complained of sudden-onset, severe pain radiating to the L4 dermatome (VAS 8/10) accompanied by numbness on both L4 dermatomes. Motor deficits were not observed. There was no bladder/bowel dysfunction. The postoperative magnetic resonance imaging (MRI) demonstrated an epidural mass with an isointense signal on T1-weighted and a hypersignal on T2-weighted sequences; the mass extended from T11-L5, consistent with acute epidural haemorrhage and compression of the dural sac at the L3-L4 intervertebral disc level (Fig. 1C-1F). No signs of vascular malformations, including dural arteriovenous malformations, were shown on the MRI.
The patient underwent re-operation at 9 hours postsurgery. The patient was prepared for a laminectomy extending from T11 to L5 in a prone position under general anaesthesia. The surgical strategy began with a re-opening of the initial surgical site to allow a faster evacuation of the SEH. A limited L4 left hemi-laminectomy was additionally performed, allowing the spontaneous expulsion of a mature blood clot. The dural sac expanded completely within the vertebral canal, and no CSF leak was noted. In addition, an epidural drain ascending to the upper lumbar levels for 5 cm was blindly introduced.
At 2 hours postsurgery, the patient presented a complete resolution of the bilateral L4 radiculopathy and numbness. Motor deficits and no bladder/bowel dysfunction were noted. The drain, opened under gravity, drained 100 ml of hematic fluid and was removed 24 hours postsurgery. The postoperative coagulopathy work-up showed no clotting disorder. No postoperative imaging was performed. The patient was discharged two days post-surgery. At two months, the neurologic examination was normal, MRI demonstrated no residual SEH, and the coagulopathy work-up was normal (Fig. 1G and 1H).
Discussion
The reported incidence of postoperative SEH following spine surgery ranges from 0.1% to 0.2% [1-4]. They are generally asymptomatic and confined to the surgical site, and symptomatic extensive thoraco-lumbar SEH are rarely reported [2]. Several risk factors have been identified, such as inadequate haemostasis before closure, multilevel procedures, age older than 60 years, a history of surgery at the same level, preoperative coagulopathy, liver and autoimmune diseases, heparinization after surgery, and hypotension during closure [1,4,6-8]. Our patient presented none of these risk factors.
In most cases, neurologic deficits are exceptional and, if present, are limited to the operated levels [9]. A MRI should be performed in postoperative spine patients with acute symptoms of neurologic deterioration [4,7]. The sagittal MRI usually demonstrates the extent of the SEH in the epidural space. The MRI features are highly suggestive of an acute haemorrhage with an isointense signal on T1-weighted and a hypersignal on T2-weighted sequences, as in the present case [5]. Sometimes, a curvilinear band of hypersignal on a T1-weighted sequence that represents the epidural fat is observed between the SEH and the dural sac and may help in differentiating between disk protrusion and SEH [10].
Rapid surgical evacuation of the SEH is a determinant factor for a complete resolution of symptoms and a full neurologic recovery [2,5,7]. It has been shown that the time interval to evacuation of patients with a full recovery was shorter than in patients with an incomplete recovery [5]. In the present case, the SEH was evacuated at 9 hours post-surgery, i.e., 1 hour after its clinical revelation that allowed a full patient recovery, in accordance with previous reports. A neurologic improvement is classically observed after evacuation of postoperative SEH. However, overall functional outcomes are poorer as compared to patients without SEH [9]. Several factors may account for this: 1) the large surgical exposure during the second surgery may delay the patient's recovery, 2) the acute and transient nerve root compression may possibly prevent initial recovery of the nerve damage, and 3) the possible development of a postoperative fibrosis secondary to the SEH and to the surgical exposure, as demonstrated on postoperative imaging by an abnormal dural sac expansion. We suggest that a limited surgical exposure, whenever feasible, may reduce postoperative fibrosis, thus leading to a better outcome.