Introduction
An osteoblastoma is a rare, benign, bone neoplasm that represents approximately 1% of primary bone neoplasms [1,2]. An osteoblastoma has a male-to-female ratio of 2:1 and occurs primarily in the first 2 decades of life [1,2]. Osteoblastomas are similar to osteoid osteomas histologically and clinically, but some characteristic differences do exist. The nidus characteristics of osteoid osteomas and osteoblastomas are different; osteoblastomas tend to form less sclerotic, but more expansible masses [3]. Also, osteoblastomas are larger, have greater growth potential with the ability of malignant transformation, and tend to cause more neurologic symptoms when located to the spine [2-4].
Case Report
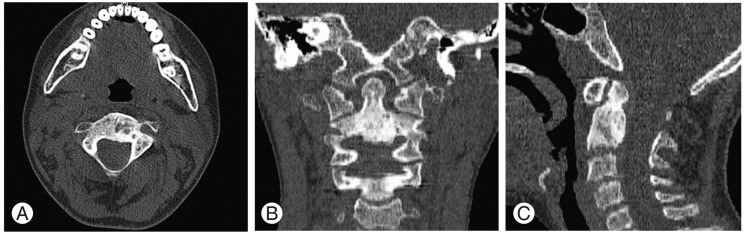
A 9-year-old boy was admitted with a 1-year history of neck pain. The pain was progressive, not relieved with medical treatment, and was causing restriction of neck movement for 2 months. The examination revealed a spasmodic torticollis which was present for 1 week. There was no history of trauma. The neurologic examination was normal. Cervical magnetic resonance imaging revealed a 13 Ă 12 Ă 15 mm mass causing erosion of the C2 corpus. The mass was slightly hypointense on T1- and isointense on T2-weighted images. Following intravenous gadolinium injection, the mass and anterior epidural soft tissue enhanced homogeneously (Fig. 1). Computerized tomography (CT) revealed a 15-mm lesion lytic in the corpus of C2 (Fig. 2).
The patient underwent surgery via an anterior approach. A 4-cm skin incision was made in the left submandibular area. After sharp dissection of the skin, subcutaneous tissues, and platysma muscle, the facial vein and marginal mandibular nerve were identified. The submandibular gland was retracted superiorly. The jugular vein, carotid artery, and vagus nerve were identified and retracted laterally. Medial to the nerve-vessel pack and below the hypoglossal nerve, the dissection was continued to the deep layer of the deep neck fascia. The deep neck fascia, prevertebral muscles, and prevertebral fascia were bluntly dissected and retracted. The C2 vertebral corpus was clearly visualized and wide enough to reach for a microsurgical approach. The cortex of C2 was removed using a high-speed bone drill. The mass was excised totally using curettes and forceps. Because bone drilling was limited and none of the structures contributing to the stability were damaged, a fusion was not performed.
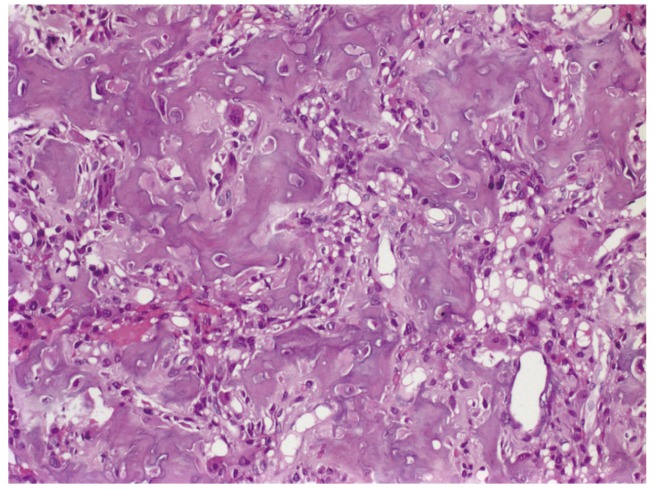
The postoperative period was uneventful and the cervical pain resolved immediately post-operatively. The histopathologic examination revealed an osteoblastoma with osteoblasts around osteoid anastomoses, giant cells, and vascular stroma (Fig. 3). The patient had radiologic assessments on a yearly basis. At the 4-year follow-up examination, the patient was symptom-free and the CT revealed sclerosis of the corpus of C2 (Fig. 4).
Discussion
An osteoblastoma is a vascular, osteoid, bone-forming lesion located mostly in the long bones and posterior elements of the spine. Corpus involvement is rare and extension is usually through the pedicles. Isolated corpus osteoblastomas are very rare.
Only two cases of osteoblastomas of the C2 corpus have been reported [7,8]. Two other reports of osteoblastomas of the C2 odontoid process have been reported, and a histologically-similar lesion (osteoid osteoma) has also been reported to occur in the C2 corpus in several case reports [5,6,9].
In the case reported by Camitta et al. [8], the surgical excision was incomplete, which inevitably led to a recurrence. The recurrent lesion was treated with chemotherapy consisting of methotrexate, doxorubicin, and cisplatin.
Local recurrences have been reported in 9.8% to 15% in other series of spinal osteoblastomas [3,4,7]. The main reason for this high rate of recurrence has been as attributed to incomplete resections. To avoid recurrences, meticulous and safe tumor curettage should be the primary goal of surgery. Considering the highly vascular nature of osteoblastomas, some authors have recommended pre-operative embolization to enhance visualization, while other authors obtain multiple biopsies to determine the exact extension of the tumor [2,5]. Another characteristic of osteoblastomas that can impair complete resection is the frequent association of epidural invasion with osteoblastomas, which causes a higher incidence of torticollis with cervical lesions, as reported by Raskas et al. [10]. Our case also had torticollis and epidural invasion was present, but we did not perform pre-operative embolization or obtain biopsies to determine the extent of the tumor. We suggest that visualization of the intraoperative surgical field is a determining factor for complete resection and the choice of surgical route is thus important.
We used an upward extension of the classical anterior cervical route for accessing the body of C2. This approach provided us with good surgical visualization and we achieved a complete resection. The transoral route is another way to reach C2, has been used by many authors, and has been reported to provide a good and safe approach to C1-C2 in experienced hands [5,9].
Osteoblastomas can be locally aggressive with a high tendency for recurrence and metastasis. Osteoblastomas can even undergo malignant transformation to osteosarcomas, although this is rare [3,8,9]. Radiotherapy and chemotherapy can be used for osteoblastomas, but the potential risk of post-radiation sarcomas must be kept in mind.