Introduction
Allodynia is caused by low intensity non-painful stimuli [1]. It usually occurs due to destructive lesions of the spinal cord or peripheral nerves, and patients usually sustain major neurologic deficits [2-4]. We herein report a case of allodynia caused by caudal lipoma surgery without associated spinal cord injury.
Case Report
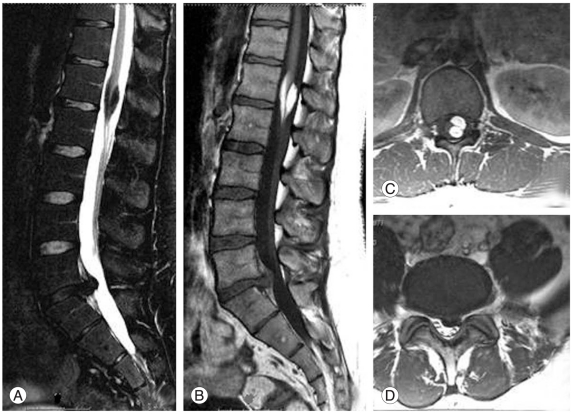
A 26-year-old man was admitted to our clinic with history of severe back and left leg pain. Neurological examination revealed mild plantar flexion deficit, absent Achilles reflex and positive Las├©gue sign on the left. Magnetic resonance imaging (MRI) showed an extruded discal herniation at the level of L5-S1 on the left, and an intradural caudal lipoma (Fig. 1). We performed microsurgical subtotal lipoma excision after L5-S1 discectomy in one session. The lipoma operation was uneventful, and surgical microscope was used throughout all excision steps. The lipoma was removed partially because of adhesion to the conus medullaris. During general anesthesia recovery, the patient complained of severe burning pain in his lower extremities that increased with painless stimuli. Pain was more prominent on the right and below the knees bilaterally. Also, the patient could not move both lower extremities due to induced pain. Analgesia did not relieve his symptoms. Eventually, high dose (250 mg/day) meperidine and gabapentine (400 mg/day t.d.s.) were given after Pain Clinic consultation. His symptoms resolved totally two weeks after the operation without neurological sequelae.
Discussion
Neuropathic pain, whether of peripheral or central origin, is characterized by neuronal hyperexcitability in the damaged areas of the nervous system. Sensory dysfunction may manifest itself as hypoesthesia or hyperesthesia. In the case of hyperesthesia, increased pain to painful stimuli is known as hyperalgesia and as allodynia to non-painful stimuli. Membrane stabilizing agents such as anticonvulsants, antiarrhythmics, corticosteroids, and agents that enhance dorsal horn inhibition such as anticonvulsants and antidepressants are used for the treatment of neuropathic pain [1].
Allodynia has been reported after spinal cord injury as a result of trauma [2], intrathecal morphine administration [3] and automated lumbar discectomy [4], but no case has been reported previously after intradural lipoma surgery [5]. In the existing reports, allodynia was always seen following spinal cord injury and associated with resultant neurological deficits [2-5]. We performed intradural lipoma operation microsurgically without incurring injury to spinal cord in our patient. Allodynia developed despite the absence of spinal cord injury and that is inconsistent with the reported cases in the literature. Also, because of the symptom free outcome without neurological sequelae, allodynia might have been secondary to chemical irritation of the conus medullaris or cauda equina with fat particles in our patient. Ectopic activity and Na++ and Ca++ channel opening may cause neuropathic pain [6]. High concentration of polyunsaturated free fatty acids in the cerebrospinal fluid obtained from patients on ketogenic diet has been shown to activate voltage gated K+ channels. Microtrauma to the cord may initiate neuropathic pain, and activation of K+ channels may prevent repolarization and sustain neuropathic pain for some time [7].
Allodynia may be seen following spinal intradural caudal lipoma surgery without associated spinal cord injury. Fat particle irritation may be the cause and the resultant symptom free recovery without neurological sequelae.