|
 |
- Search
| Asian Spine J > Volume 5(4); 2011 > Article |
Abstract
Surgical treatment for spinal tuberculosis is necessary in particular cases that a large amount of necrotic tissue is encountered and there is spinal cord compression. A spinal shortening osteotomy procedure has previously been described for the correction of the sagittal balance in a late kyphotic deformity, but there have been no reports on this as a surgical treatment in the acute stage. Thus, the aim of this report is to present the surgical techniques and clinical results of 3 patients who were treated with this procedure. Three patients with tuberculous spondylitis at the thoracic spine were surgically treated with this procedure. All the patients presented with severe progressive back pain, kyphotic deformity and neurological deficit. The patients recovered uneventfully from surgery without further neurological deterioration. Their pain was improved and the patients remained free of pain during the follow-up period. In conclusion, posterior spinal shortening osteotomy is an alternative method for the management of tuberculous spondylitis.
Spinal tuberculosis is most common form of extrapulmonary tuberculosis, and it comprises approximately 50% of all cases of skeletal tuberculosis. In general, antituberculous chemotherapy is considered the fundamental treatment of this condition, but surgery is still necessary for the particular cases in which here is a large amount of necrotic tissue and spinal cord compression is noted [1,2]. The principle of operative management for spinal tuberculosis is to decompressed the spinal cord by removing the necrotic tissue and draining of any abscess, and this is follow by immobilization. Yet the infected vertebrae are prone to collapse and they require mechanical support to prevent progressive deformity [3].
There is no standard method for the surgery of tuberculous spondylitis. Many procedures have been described and these consist of anterior debridement with anterior or posterior spinal fixation, posterior debridement and spinal reconstruction, as examples. These procedures require an interbody bone graft to restore the spinal alignment. Nevertheless, complications associated with interbody bone graft placement have been reported, such as graft failure and progressive collapse [1-3].
Spinal shortening osteotomy is an alternative method for treating spinal tuberculosis, and especially for the correction of the sagittal balance in a late kyphotic deformity [4,5]. This technique has several advantages such as an enhanced bony contact surface and no interbody graft placement with the intention of restoring the sagittal spinal alignment. We think these procedures should be superior to the former methods in order to reduce the complications associated with graft placement and to enhance bony healing. However, to the best of our knowledge, there is no report on spinal shortening ostotomy as a surgical treatment for the active disease stage of tuberculous spondylitis without a severe rigid angular kyphotic deformity. Thus, the aim of this report is to present our surgical techniques and the clinical and radiographic results of the patients treated with this procedure.
Under general anesthesia the patient was turned to prone position. The abdomen was allowed to hang free to prevent any compression to the vena cava. Due to our limitation of equipment, no intraoperative neuromonitoring was used during the operation. A straight vertical midline incision was made to extend two vertebrae above and below the affected vertebral segment. The paraspinal muscles were dissected and then retracted laterally. After identifying the pathological level with an image intensifier, pedicular screws were inserted into the pedicles of the 2 vertebrae above and below the pathological level. After that, the dissection was carried out more laterally to expose the costovertebral joints of the lower affected vertebra and then over the posterior surface of the ribs about 5 cm laterally. After complete exposure, the osteotomy procedure was initially performed from one side of the vertebral column. First, the rib was cut and subsequently, with gentle blunt dissection, the parietal pleuron was dissected out with gentle blunt dissection and the intercostal artery was identified and ligated. After that, the costovertebral joint was divided and the rib was dissected out from the intercostal muscles and removed. A total laminectomy at the pathological level was then performed to decompress the neural elements and subsequently, using a high speed drill, the pars interartricularis was cut laterally until reaching the lateral border of the vertebral body. The nerve root was then identified and sacrificed to gaining the exposure. The pedicle of the lower vertebral body of the affected segment was then identified and removed to expose the diseased vertebral level (Fig. 1). After that, the necrotic material within the disc and the vertebral bodies, beneath the dural sac, were removed using curettes and pituitary forceps. The paravertebral abscess was then identified and drained. After adequate debridement of all the infected material, the residual cortex of the posterior parts of the vertebral bodies attached to the posterior longitudinal ligament was removed. After completing one side, the spinal plate was then applied to the ipsilateral side of the vertebral column in order to prevent vertebral collapse and then the operation was performed in similar steps on the other side. However, in case 1, in addition to the procedure described above, the left transverse process of the T11 was also cut using a high speed drill to expose the lower part of a large extensive anterior paravertebral abscess for irrigation and drainage. After completing the debridement around the dural sac, the spinal plate was then applied and a vertebral column shortening maneuver was then performed by adjusting the posterior instruments to achieve bony contact (Fig. 2). The neural tissues were then checked again for any compression that might have occurred during the maneuver. Additionally, posteriorlateral fusion along the instrumented area beneath the spinal plates was then performed with local bone grafts.
Three patients with tuberculous spondylitis at the thoracic spine were surgically treated with this procedure. All the patients presented to our clinic with severe progressive back pain. The lesions were confined in the T11-T12, T10-T11 and T7 vertebral segments, and in addition, kyphotic deformity of the spinal column was detected in all the patients. A localized paravertebral abscess was observed on the magnetic resonance images (MRIs) in all the patients, but in 1 patient (case 1) the abscess had extensively spread along the anterior longitudinal ligament. Surgical intervention was indicated as neurological deficits were detected in all the patients. All the patients recovered from the surgery uneventfully without further neurological deterioration. The pathological diagnosis confirmed caseous granulomatous inflammation in all the cases. Antituberculous chemotherapy was prescribed for 12 months for all the patients. The treatment regimen was as follow: isoniazid 300 mg/day plus rifampicin 600 mg/day (for the patients who weighted more than 50 kg) or 450 mg/day (for the patients who weighted less than 50 kg) plus pyrazinamide 30 mg/kg/day and ethambutol 25 mg/kg/day for 2 months and this was followed by isoniazid plus rifampicin for the other 10 months. The patients' pain was dramatically improved after the operation and all the patients remained free of pain during the follow-up period.
A 39-year-old male was admitted to our clinic with the history of back pain for 3 years. The pain was located at the mid thoracic region. He had been diagnosed with tuberculous spondylitis and he had received antituberculous chemotherapy for 6 months, but his symptoms were not improved. Further, he had also been treated with local drainage of pus from his back twice in a 2 years period. The plain X-ray revealed 50% vertebral collapse at T7, which resulted in a slight kyphotic deformity (Fig. 3A). Unfortunately, 1 month later, his symptoms progressed and acute neurological deterioration was detected. The emergency MRI revealed T7 vertebral collapse with a retropulsed fragment compressing the dural sac. In addition, a extensive prevertebral abscess that extended from T6 down to T12 was also identified (Figs. 4 and 5). He underwent surgical decompression and fixation, using our presented technique, with the drainage of the large extensive abscess by partial transversectomy of T11. The patient recovered from the operation uneventfully and immediate improvement of his neurological status (ASIA score improvement from D to E) was observed.
A 35-year-old woman came to our clinic with progressive weakness of the lower extremities for 6 days. The motor weakness was detected only on her right leg, but a sensory deficit was observed on both legs below the knee. The initial X-ray revealed an erosion of the upper and lower vertebral endplates and destruction of the intervertebral disc of the T11-T12 vertebral segment that result in kyphotic deformity. MRI demonstrated inhomogeneous signal intensity and destructive lesion at the T11-T12 vertebral segment, which resulted in segmental kyphosis and caused dural sac compression at the T11 vertebral level (Fig. 6A). Formation of a paravertebral abscess was also detected (Fig. 6B). The patient was scheduled for emergency surgical decompression using our presented technique (Fig. 7). The post operative course was uneventful and neurological improvement (ASIA score improvement from C to E) was observed.
A 40-year-old woman was admitted to our clinic with back pain and progressive weakness of both legs. The X-ray revealed superior end plate erosion at T11 and destruction of the intervertebral disc space, which resulted in kyphotic angulations at this vertebral segment (Fig. 8A and 8B). MRI in this case demonstrated the destructive lesion of the T11 anterior endplate and abnormal signal intensity of the vertebral body with spinal canal compromise due to necrotic material, and MRI also demonstrated abnormally increased signal intensity of the T9 and T10 vertebrae. Vertebral shortening osteotomy was performed at the upper half of the T11 vertebral body using our presented technique (Fig. 9). The patient recovered from the operation uneventfully and improvement of her neurological status (ASIA score improvement from C to E) was observed during the follow-up
period.
Tuberculosis of the spine is an unstable lesion that tends to progress at least until bony union is accomplished. As a result, kyphotic deformity usually occurs and this may cause serious problems such as late paraplegia [1]. Anterior radical surgery and arthrodesis have been described and advocated in the past decade as a standard treatment for spinal tuberculosis. The advantage of this method is direct access to the lesion and the lesion can be eradicated by excision of the disease, there is rapid osseous healing and a decreased tendency for progressive collapse [3]. The complications associated with anterior surgery have also been reported such as progression of kyphotic deformity and graft failure [1,3]. However, with modern drug therapy, spontaneous fusion can occur after medical treatment and so aggressive debridement can be avoided [2]. Posterior instrumentation has been introduced to reconstruct the spinal stability and prevent such complications, and many good clinical results have been demonstrated and this all strongly supports the importance of spinal fixation in the surgical management of spinal tuberculosis in selected cases [6,7]. As was seen in our results, bony healing can be expected even though a small amount of bone is left after surgery, as was demonstrated in case 1 (Fig. 3B).
In this present study, we prefer a posterior approach because of our familiarity with it, the procedure's simplicity and the lower complication rate. Along with the posterior approach, we can also remove the infected material by using our modification of the costotransversectomy technique. In our modified technique, the exposure is wide enough to approach the lateral border of the infected vertebral segment for debridement and to drain a paravertebral abscess. Moreover, after removing the pedicles, it provides adequate exposure for debridement of the infected tissue beneath the dural sac (Fig. 1). Then with the spinal implant, and preferably a pedicular screws plate system, we shorten the vertebral column in order to achieve the bone to bone contact, and so an interbody graft is not necessary. In addition, with this technique, we can correct the kyphotic deformity and more importantly good bony healing should be expected because of the large area of bony contact and the rigid stabilization of the spinal fixation system. However, Rajasekaran et al. [5] reported on a disadvantage of the posterior shortening procedure as it will jeopardize the spinal cord by excessive kinking. In addition, deformation of the spinal cord due to the cord sliding and a decrease of blood flow have been reported as causes of neurological deficit after the shortening procedure [8,9]. Vertebral shortening osteotomy can be safely performed if the range of shortening does not exceed 20 mm [10] and additional laminectomy may be added to prevent the excessive deformation of the spinal cord [8]. With our technique, we performed wide laminectomy in addition to the shortening procedure to provide space for the indentation of the spinal cord and the shortening was limited into the safe range. Thus, we did not note any neurological deterioration after the surgery in our patients.
In conclusion, posterior spinal shortening osteotomy and fixation in combination with debridement is an alternative method for the management of tuberculous spondylitis. This procedure offers the advantages of an access to the infected vertebral segment for performing debridement and draining the paravertebral abscess and it provides adequate exposure for the removal of infected tissue beneath the spinal cord. In addition, a kyphotic deformity can be corrected and for which good bony healing can be expected.
References
1. Hsu LC, Cheng CL, Leong JC. Pott's paraplegia of late onset: the cause of compression and results after anterior decompression. J Bone Joint Surg Br 1988 70:534ŌĆō538. PMID: 3403593.



2. Chacko AG, Moorthy RK, Chandy MJ. The transpedicular approach in the management of thoracic spine tuberculosis: a short-term follow up study. Spine (Phila Pa 1976) 2004 29:E363ŌĆōE367. PMID: 15534398.


3. Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Joint Surg Am 1989 71:1314ŌĆō1323. PMID: 2793883.


4. Kawahara N, Tomita K, Baba H, Kobayashi T, Fujita T, Murakami H. Closing-opening wedge osteotomy to correct angular kyphotic deformity by a single posterior approach. Spine (Phila Pa 1976) 2001 26:391ŌĆō402. PMID: 11224887.


5. Rajasekaran S, Vijay K, Shetty AP. Single-stage closingopening wedge osteotomy of spine to correct severe posttubercular kyphotic deformities of the spine: a 3-year follow-up of 17 patients. Eur Spine J 2010 19:583ŌĆō592. PMID: 20013004.


6. Lee TC, Lu K, Yang LC, Huang HY, Liang CL. Transpedicular instrumentation as an adjunct in the treatment of thoracolumbar and lumbar spine tuberculosis with early stage bone destruction. J Neurosurg 1999 91(2 Suppl): 163ŌĆō169. PMID: 10505499.

7. Moon MS, Woo YK, Lee KS, Ha KY, Kim SS, Sun DH. Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine (Phila Pa 1976) 1995 20:1910ŌĆō1916. PMID: 8560340.


8. Alemdaro─¤lu KB, Atlihan D, Cimen O, Kilin├¦ CY, Iltar S. Morphometric effects of acute shortening of the spine: the kinking and the sliding of the cord, response of the spinal nerves. Eur Spine J 2007 16:1451ŌĆō1457. PMID: 17426990.



9. Kawahara N, Tomita K, Kobayashi T, Abdel-Wanis ME, Murakami H, Akamaru T. Influence of acute shortening on the spinal cord: an experimental study. Spine (Phila Pa 1976) 2005 30:613ŌĆō620. PMID: 15770174.


10. Hsieh PC, Stapleton CJ, Moldavskiy P, et al. Posterior vertebral column subtraction osteotomy for the treatment of tethered cord syndrome: review of the literature and clinical outcomes of all cases reported to date. Neurosurg Focus 2010 29:E6PMID: 20594004.

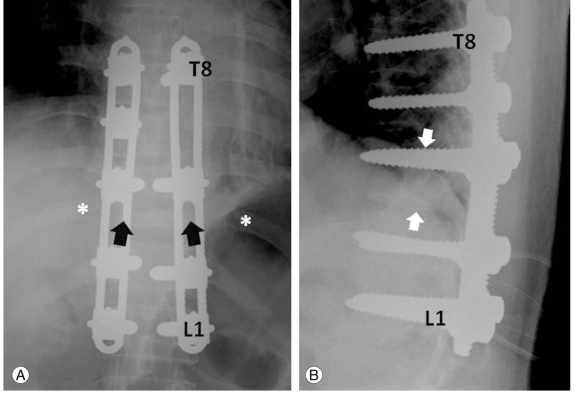
Fig.┬Ā1
Case 2. The illustrative figure of the vertebral shortening osteotomy operation. After resection of the left 12th rib, larminectomy of T11-T12 and the left T12 pedicle and pars resection were done. The exposure (between the white arrows) is wide enough for removal of the necrotic tissue and to drain the abscess. The infected material beneath the dural sac can be removed through the resected pedicle (*).

Fig.┬Ā2
Case 2. The illustrative figure shows the final step of the vertebral shortening osteotomy procedure. After complete removal of all the necrotic material, the dual spinal plates are applied and adjusted for the compression of the vertebral bodies (block white arrows). Kinking of the dural sac is also observed (white star).

Fig.┬Ā3
Case 1. The plain X-ray lateral view before the surgery (A) revealed 50% collapse of the T7 vertebra and this resulted in a slight kyphotic deformity. After surgery (B), shortening of the vertebral column was demonstrated and bony healing was observed (block white arrows).
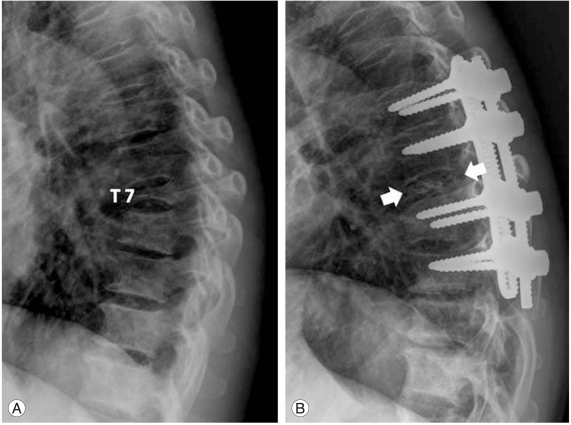
Fig.┬Ā4
Case 1. The magnetic resonance imaging sagittal view (A) revealed the increase signal intensity of the T7 vertebral body. Vertebral body collapse and a retropulsed fragment that compressed the dural sac were observed. A large extensive paravertebral abscess that extended from T6 down to T12 was demonstrated, as is indicated by the white arrows in (B).

Fig.┬Ā5
Case 1. The magnetic resonance imaging axial view at T7 showed the degree of dural sac compression by the retropulsed fragment and the necrotic materials (*). The white arrows indicate the large paravertebral abscess around the vertebral body and that extends down to T12.
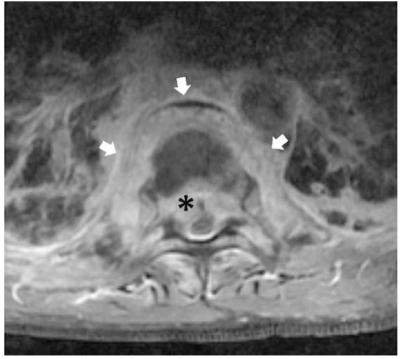
Fig.┬Ā6
Case 2 The magnetic resonance imaging (MRI) sagittal view (A) shows inhomogeneous signal intensity at the T11-T12 intervertebral disc level. The upper end plate of T12 was collapsed and this resulted in angulations of T11 and it caused dural sac compression (block white arrows in [A]). The MRI axial view at the pathological level (B) shows the degree of dural sac compromise by the necrotic material (white star) and the local paravertebral abscess (black arrows) is demonstrated.

Fig.┬Ā7
Case 2. Post operative X-ray anterior-posterior (A) and lateral (B) views after shortening osteotomy. Spinal instrumentation was applied from T9 to L2 with the compression of T11-T12 (white arrows in [A] and [B]), and the spinal alignment was restored.
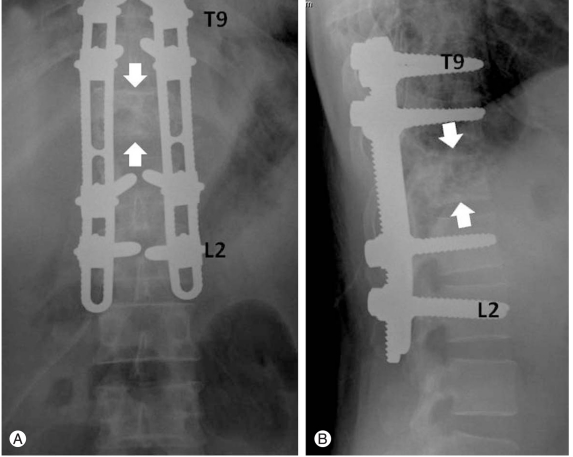
Fig.┬Ā8
Case 3. The preoperative X-rays (A) and (B) revealed superior end plate erosion at T11 (block white arrows in [B]) and this resulted in kyphotic angulations at this vertebral segment.

Fig.┬Ā9
Case 3. The postoperative X-ray after vertebral shortening osteotomy is shown in (A) and (B). The 11th ribs was cut (*) and the T11 pedicles were removed (block black arrows). Spinal instruments were applied from T8 to L1 and this compressed the T11 remaining body against T10 (block white arrows in [B]).