The Trajectory of Iliac Screw in the Axial Plane in 200 Korean Patients
Article information
Abstract
Study Design
A retrospective radiographic analysis.
Purpose
To estimate the accurate trajectory in the axial plane for iliac screw insertion in 200 Korean patients using radiographic images.
Overview of Literature
Several complications have been encountered after fusion to the lumbosacral junction, including pseudarthrosis, S1 screw loosening, and sacral fractures. Iliac screw fixation is considered an efficient method for augmenting sacral screw fixation but there are few reports on the trajectory of iliac screw insertion. The trajectory in the sagittal plane can be visualized by intraoperative fluoroscopy. However, there is no method to check the accuracy of the trajectory in the axial plane during surgery.
Methods
Between January 2007 and February 2009, 200 patients (107 men and 93 women) who underwent L-spine computed tomography were enrolled in this study. The mean age of the patients was 55.6 ± 18.3 years (range, 13 to 92 years). The spino-iliac angle (SIA) was measured on the axial image at the S1 level, which was defined as the angle between a vertical line through the center of the spinous process and an oblique line that passed through the center of the outer and inner cortices of the ilium.
Results
The group mean SIA was 30.1° ± 7.8°; 30.1° ± 7.7° for men and 29.9° ± 81.1° for women. There was no significant difference according to gender or age (p > 0.05).
Conclusions
The SIA for the axial trajectory of iliac screws is approximately 30° in Korean patients.
Introduction
Instrumented fusion of the lumbosacral (LS) joint is generally performed due to the unacceptably high rate of pesudoarthrosis with non-instrumented fusion [1]. The sacrum is often not strong enough to withstand the increased cantilever force produced by extended LS instrumented fusion, resulting in the failure of instrumentation, screw loosening, posterior pull-out, or sacral fracture [2].
Iliac screw fixation has been reported to increase the LS fusion rate, particularly for long-level spinal fusion including the LS joint, or for high-grade LS spondylolisthesis [3]. However, inaccurate placement of the iliac screws can cause buttock pain and weaken the screw purchase. Despite the reports of iliac screw fixation [3,4] the trajectory of the screw is largely decided by the surgeon, and to our knowledge, there are no reports describing the screw trajectory.
This study examined the axial trajectory of iliac screw insertion to provide a reference for surgeons performing an intracortical trajectory through the iliac bone.
Materials and Methods
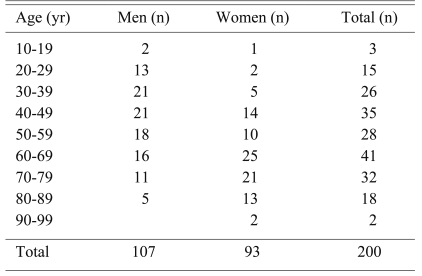
Between January 2007 and February 2009, 241 individuals underwent lumbar spine computed tomography (CT) radiography. Of those, 200 (107 men and 93 women) were enrolled this study (Table 1). The mean age of the patients was 55.6 ± 18.3 years (range, 13 to 92 years); 49.2 ± 17.6 years (range, 14 to 88 years) for men and 63.2 ± 16.6 years (range, 13 to 92 years) for women. The exclusion criterion was a variation in the morphology of the LS and iliac bones caused by a deformity, fracture, or previous surgery. The data from each patient were used only once in the study.
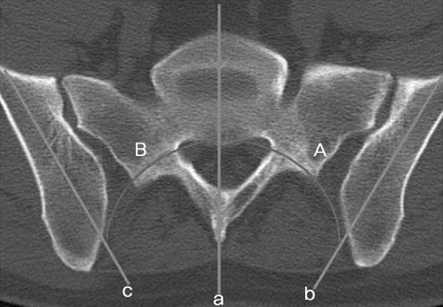
The lumbar spine CT taken with a Somatom sensation 64 (Siemens, Munich, Germany) was analyzed using a Picture Archiving and Communication System (PACS, Infinitt, Seoul, Korea). The axial image was selected at the S1 level to evaluate the axial trajectory of the iliac screw insertion angle, which we describe as the spino-iliac angle (SIA) (Fig. 1). A median line was drawn to connect the midpoint of the sacral spinous process with the anterior aspect of the sacral body. Two oblique lateral lines were drawn through the midline of the inner and outer cortex of both iliac wings. The angle, which means the SIA, was measured between the median sacral line and the oblique lateral iliac line on both sides. The measurements were performed twice by two orthopedic doctors and the mean was used. The results were analyzed using a Student's t-test or ANOVA on SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). A p-value of < 0.05 was considered significant.
Results
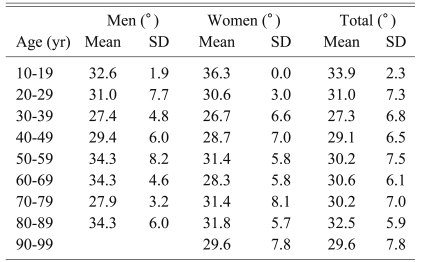
Table 2 lists the measured SIAs according to gender and age. The group mean of the SIA was 30.1° ± 7.8°; 30.1 ± 7.7° for males and 29.9° ± 8.1° for females. There was no significant difference in SIA between the males and females (Student's t-test, p = 0.964) (Fig. 2).
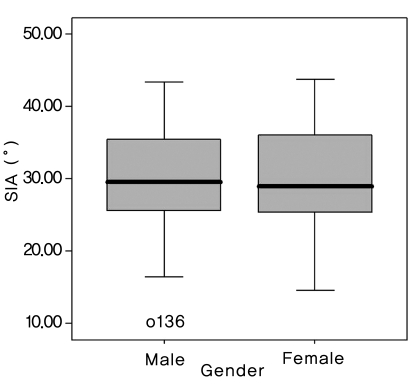
Box plot for the male and female group. There was no significant difference in spino-iliac angle (SIA) according to gender. Student's t-test, p = 0.964.
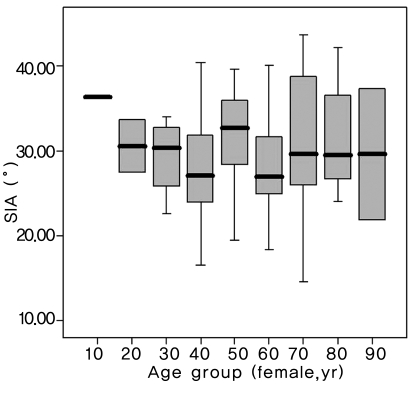
When a SIA comparison was performed according to age in decades, there was no significant difference between them (ANOVA, p = 0.484) (Table 2, Fig. 3). Although decade-age comparison in the male group data showed a less even distribution, there was no significant difference in the male (ANOVA, p = 0.067) (Fig. 4) or female groups (ANOVA, p = 0.716) (Fig. 5).

Spino-iliac angle (SIA) of the total group. There was no significant difference in SIA according to age. ANOVA, p = 0.484.
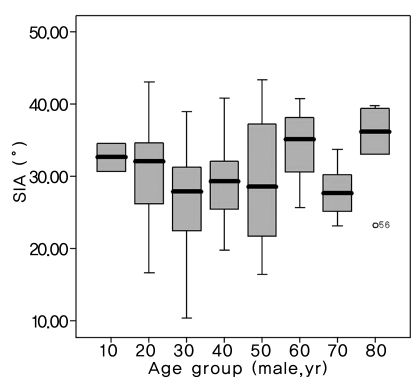
Spino-iliac angle (SIA) in the male group. There was no significant difference in SIA according to age. ANOVA, p = 0.067.
Discussion
Proper iliac screw fixation can prevent pelvic obliquity, pseudarthrosis, and posterior pull-out of the instrument. It helps stabilize the spine after a correction of coronal or sagittal imbalance and prevents recurrence of the deformity. Galveston instrumentation and iliac screw fixation are used widely to correct spinal deformities, and a comparison of the two methods in the treatment of neuromuscular scoliosis showed no significant difference in the coronal C7 plumb line, sagittal C7 plumb line, or the coronal Cobb angle correction [5]. In contrast, a pelvic obliquity correction was significantly better with iliac screw fixation than with the Galveston technique [5]. Segmental fixation of the sacral and lumbar vertebrae with additional fixation using iliac screws produced stronger LS fixation and improved the pelvic correction. Better stability at the LS joint helps increase the fusion rate.
The Galveston prosthesis was reported to allow fine movement of the ilium with few side effects [6]. Sacral fixation is weaker when osteoporosis is present and can cause an increase in the rate of sacrum failure due to cantilever overload. Secure fixation to the sacral screw will distribute the cantilever force and improve fixation. The iliac screw is oriented in the anteroinferior direction to provide stability in flexion-extension and rotational movement of the spine [6].
The first-generation iliac screw was unlocked and tended to protrude posteriorly. The second-generation was designed with a locking mechanism that improved stability. The third-generation iliac screw had a low-profile construct that decreased the level of discomfort arising from the posterior protrusion of the screw into the buttock [7].
Our surgical technique for iliac screw insertion involves a dissection to expose the posterior iliac spine, a resection of the posterior iliac spine to approximately 2×2 cm in size until it is flush with the sacrum. This prevents posterior protrusion of the screw head into the buttock. The probe is inserted into a point slightly proximal to the most posterior part of the posterior iliac spine, which has the widest cancellous bone surface. The sciatic notch is identified in the sagittal plane using an image intensifier located in the ortho position. The image is used to guide the iliac screw 1 cm above the sciatic notch where the cancellous bone is densest [5]. The gear-shift probe is inserted in the axial plane and the curved tip is aimed medially because the lateral cortex of the ilium is easier to perforate. The iliac screw is relatively thick (6.0-7.5 mm diameter) and long (60-70 mm), and causes pain when inserted in the buttock after perforating the lateral cortical wall of the iliac wing (Fig. 6) [3]. In our clinical experience, a screw with a divergent trajectory of 45° on the axial plane protruded the outer cortex of the ilium, while a screw with a divergent trajectory of 29°-30° remained intracortically (Figs. 6 and 7).

Iliac screw inserted 45° outward in the axial plane resulted in outer-wall protrusion of the iliac bone. In contrast, 30° outward in the axial plane caused it to remain in the intracortical trajectory.

Successful intracortical trajectory into the iliac bone. The axial plane measurements were 29° bilaterally.
It is believed that the axial trajectory referenced by the spinous process in the axial image is useful for finding the correct axial trajectory. In this study, the mean axial trajectory of the SIA was 30.1° ± 7.8°. No significant difference in SIA was found for gender (Student's t-test, p = 0.964) or age (ANOVA, p = 0.484). The low sample number due to data subgrouping of gender and age would have caused an uneven distribution of the means. The age comparison in the male group showed a p-value of 0.067, which is close to the level of significance. The comparison between the group in their 30's vs. those in their 60's and those in their 30's vs. those in their 80's made a contribution to an uneven distribution of the entire group data, but not to the level of significance (Fig. 4). This effect became unclear as the sample number was increased to the total group (Fig. 3). Preoperative confirmation of the SIA using CT or magnetic resonance imaging would further enhance the accuracy of the axial trajectory (Fig. 7). The use of a standardized sagittal trajectory, axial trajectory, screw insertion point and screw length would eliminate the controversy over the location of the screw placement.
A bone graft can be harvested from the ilium without affecting the stability of the iliac screw when the donor site is more than 1 cm away from the screw trajectory [3]. The surgeon should harvest the iliac bone 1-2 cm from the posterior iliac spine in a young patient so the iliac screw can be implanted easily in future revision surgery [3]. A follow-up is recommended to confirm that the iliac screw fixation has improved the LS stability, fusion rate and sagittal balance.
The iliac screw will occasionally loosen [7], caused in part by inserting the iliac screw without attempting to fuse the bone. Unless delivery is planned, decortication of the sacrum and the creation of a bone bridge along the posterior wall of the sacroiliac joint may improve the stability after iliac screw insertion.
The limitation of this study was that it was based on radiographic data and will need to be correlated with the clinical outcomes. This can be achieved in future studies using a larger cohort.
Conclusions
The axial trajectory for iliac screw insertion was found to be approximately 30°. This angle produces biomechanically stable distal fixation that can withstand the increasing cantilever force that occurs as the level of fusion is increased.