Postoperative Meningitis in Patients with Cervical Cord Tumor: A Case Report
Article information
Abstract
Postoperative meningitis after spinal surgery is a rare complication that can result in a life-threatening condition. Linezolid (LZD) is an oxazolidinone which has been approved in Japan for infections caused by methicillin-resistant Staphylococcus aureus. The authors encountered a case of postoperative meningitis with cerebrospinal fluid leakage (liquorrhoea) that occurred after resection of a cervical cord tumor. The infection was caused by methicillin-resistant Staphylococcus epidermidis(MRSE). Debridement and suture of the dura matter was carried out. LZD was given intravenously. The infection was cured without any sequelae. Based on this result, we concluded that LZD might be considered as one of the first choices for the treatment of postsurgical meningitis caused by MRSE.
Introduction
Postoperative spinal infection is an unfavorable complication, and superficial and deep wound infections are included in this category. In a survey of postoperative spinal infections that included more than 2000 cases of spinal operation, the overall infection rate was reported to be 1.9% [1]. Postoperative meningitis after spinal surgery is a rare complication that can result in a life-threatening condition. Several therapeutic methods have been employed for treating postoperative meningitis. Linezolid (LZD) is an oxazolidinone, which is a new class of antibiotics [2]. It has been approved in Japan for infections caused by methicillin-resistant Staphylococcus aureus. LZD has a higher rate of penetration rate into the cerebrospinal fluid (CSF) than vancomycin (VCM) [3]. Previous reports have described the efficacy of LZD for central nervous system infection, including postoperative meningitis after intracranial surgery [3-8]. We present here a case of postoperative meningitis with CSF leakage (liquorrhoea) that occurred after resection of a cervical cord tumor. The infection was caused by methicillin-resistant Staphylococcus epidermidis (MRSE). Debridement and suture of the dura matter was carried out. Subarachnoid drainage from the lumbar spine was also done and LZD was given intravenously. The infection was cured without any sequelae. These treatments were considered to be effective in this patient.
Case Report
A 39-year-old woman complained of neck pain and left scapular pain in January 2006. The symptoms gradually increased and she was eventually admitted to our hospital. Physical examination revealed deep tendon hyper-reflexia of the upper and lower extremities. Motor palsy was not evident and no sensory disturbance was found in the upper or lower extremities or in the trunk. The plain lateral radiography did not show any abnormality. The antero-posterior radiography showed enlargement of the left C3-4 foramen (Fig. 1). Cervical magnetic resonance imaging demonstrated a dumbbell type tumor compressing the spinal cord at the C3-4 levels (Fig. 2). The tumor was located on the left side of the spinal cord. The tumor showed low intensity on the T1-weighted image and iso-high or slightly high intensity on the T2-weighted image. Gadolinium enhancement was noted in the tumor (Fig. 2).

Anteroposterior radiograph of the cervical spine. Enlargement of the left C3-4 foramen was observed (arrows).
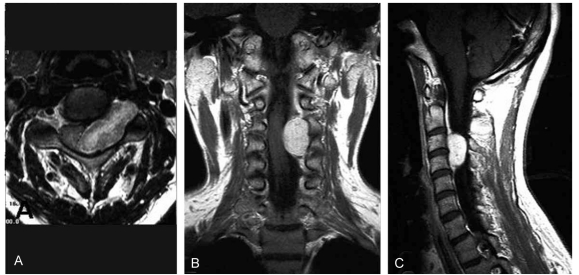
Preoperative magnetic resonance imaging of the cervical spine. The axial T2 image revealed a dumbbell type tumor compressing the spinal cord at the C3-4 levels (A). The gadolinium-enhanced frontal (B) and sagittal images (C) indicated that the tumor was markedly enhanced.
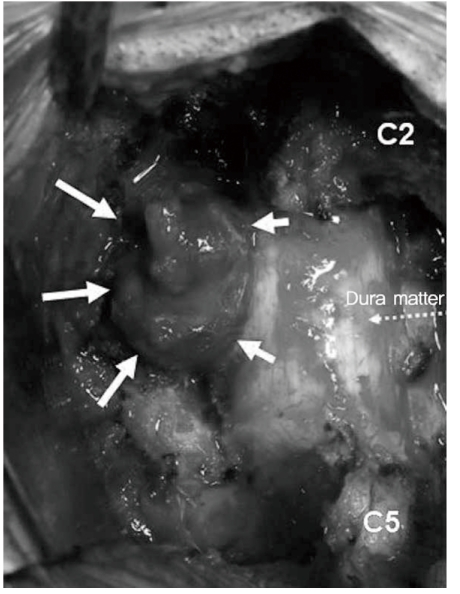
The patient underwent an operation in April 2006. Cervical laminectomy at C3-4 was carried out and total resection of the cervical tumor was performed. The tumor was encapsulated (Fig. 3) and it involved the posterior ramus of the C4 spinal nerve, and so the nerve was resected. The dura mater was opened to identify the presence of any intradural tumor invasion, but no intradural invasion was observed. Thereafter, the dura matter was tightly sutured. The round-shaped dark red tumor mass was covered by a thin membrane. The size of the tumor was 2.6 × 2.4 × 1.3 cm. The histological examination revealed a schwanoma with both Antoni type A and type B areas. No malignant characteristics were found for the pathology.
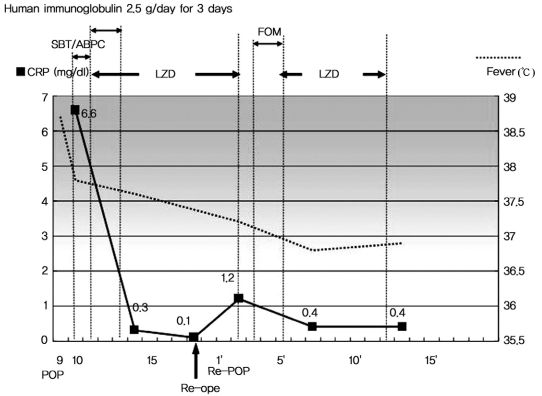
The surgical drain was removed 2 days after surgery. The patient had a slight fever. On the 9th postoperative day, she displayed a high grade fever (> 39.0℃) and vomiting. The Kernig sign was observed. She had fluctuation near the surgical wound, and so a spinal cord puncture was carried out; 25 ml of turbid CSF was obtained near the surgical wound. Culture of the CSF revealed MRSE. We diagnosed that she was suffering with postoperative meningitis. The patient also had liquorrhoea. Debridement was performed and the laceration of dura matter was sutured on the 18th day after the first surgery. The size of laceration was 1 mm in diameter at the site where the posterior ramus of the C4 spinal nerve was resected (Fig. 4). She had drainage from the lumbar spine for 1 week after the second surgery. As for chemotherapy, she received intravenous administration of 600 mg of LZD twice a day from the 11th day to the 20th day after the first surgery, and the same dose of LZD was given from the 5th day to the 12th day after the second surgery. These treatment methods, including the second surgery, spinal drainage and chemotherapy, were very effective. The patient did not have fever thereafter and the infection healed. She was discharged on the 18th day after second surgery (Fig. 5). Thereafter, she has had an excellent postoperative course and no recurrence of infection or tumor was observed for the following 3 years.
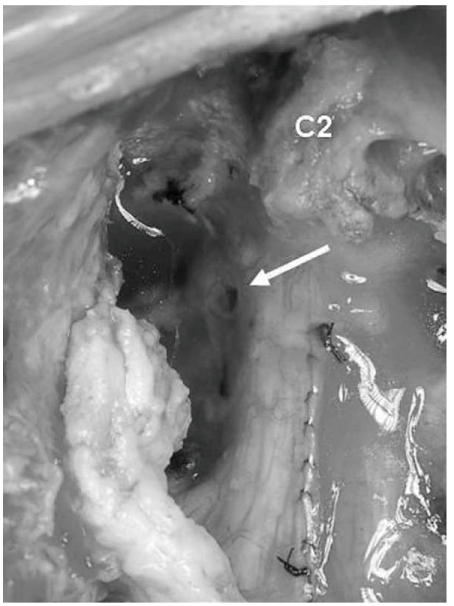
Intraoperative findings at the second surgery. The defect of the dura matter was found and liquorrhoea through the defect was observed (arrow). The defect was tightly sutured.
Discussion
We present here an unusual case of postoperative meningitis that was caused by MRSE following cervical cord tumor resection. Surgical infection is rarely encountered after spine surgery, yet therapeutic problems occur when it is encountered. Weinstein et al. [1] described that among 2391 operative procedures of the spine, 46 cases of wound infection were identified, yielding an overall infection rate of 1.9%. A multicenter study in the USA revealed that 11.9% of the patients with neuromuscular scoliosis had deep wound infection after surgery [9]. Although the incidence of postoperative meningitis after spine surgery is unknown, this infectious condition is thought to be very rare. Regarding the mechanism of postoperative meningitis in the present case, it is speculated that the infection occurred at the surgical site and it spread into the intradural space. We opened the dura matter because we anticipated the tumor had invaded to the intradural space. The opened region was then firmly sutured. Although there was no neural deficit after resection of the C4 nerve root, the liquorrhoea through the dural defect from the resection of the C4 spinal nerve and the dead space from the removal of the tumor might have been the background of the infection. Several papers have pointed out that liquorrhoea might cause the formation of a dural cutaneous fistula and this increases the risk of postoperative meningitis [10-12]. Those reports emphasized that repair of the injured dura matter and lumbar subarachnoid drainage should be carried out as a means of preventing meningitis or pseuromeningocele.
We used LZD as chemotherapy against the MRSE meningitis in the present case. It proved to be very effective for the treatment, based on the patient's favorable clinical and laboratory course after the occurrence of infection. LZD is an oxazolidinone, which is a new class of antibiotics. It has shown consistent inhibitory activity against multiresistant Staphylococci, Enterococci and Pneomococci [13]. LZD selectively binds to the 50S ribosomal subunit near the interface with the 30S subunit, which results in a distortion that inhibits the formation of the initiation complex [2]. Intravenous administration of VCM or teicoplanin (TEIC) is generally considered as first line treatment for methicillin-resistant gram positive cocci. However, intravenous administration of VCM and TEIC results in a low concentration of drug in the CSF. The ratios between the concentrations of antibiotic in the CSF and plasma have been reported as 18-40% for VCM [14] and less than 10% for TEIC [15]. On the other hand, the ratio is extremely high for the intravenous administration of LZD. It was reported to be 160% on average, and it ranged from 120% to 230% [3]. Thus, intravenous administration of LZD has an advantage for the treatment of meningitis induced by methicillin-resistant gram positive cocci. In fact, there have been two case reports that discussed the beneficial effect of LZD against the postneurosurgical meningitis caused by MRSE after cranial surgery [5,6] and where intravenous VCM failed to eradicate the infection. LZD might be considered as one of the first choices for the treatment of postsurgical meningitis caused by MRSE.