Simultaneous Anterior and Posterior Surgery in the Management of Tuberculous Spondylitis with Psoas Abscess in Patients with Neurological Deficits
Article information
Abstract
Study Design
This is a retrospective study.
Purpose
We wanted to evaluate the treatment outcomes of performing simultaneous anterior and posterior surgery for patients with tuberculous spondylitis and psoas abscess.
Overview of Literature
Although various treatment options have been used for spinal tuberculosis, there are only a few reports on the treatment of tuberculous spondylitis with psoas abscess.
Methods
Between March 1997 and February 2006, we performed operations on 14 cases of tuberculous spondylitis with psoas abscess. All the cases underwent anterior debridement with an interbody bone graft and posterior fusion with using pedicle screws.
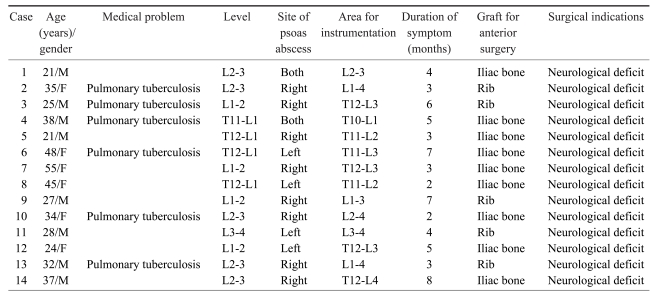
Results
Under the Frankel classification, 1 case improved by two grades, 10 cases improved by 1 grade and 3 cases demonstrated no change. The Kirkaldy-Willis functional outcomes were classified as excellent in 10 cases and good in 4. One year after surgery, bony union was confirmed in all 14 cases. The mean kyphotic angle of the spinal lesion was 12.4° and the mean lordotic angle at the final follow-up was 6.4°. Postoperative complications (superficial wound infections) were encountered in 2 cases.
Conclusions
Our results demonstrate that anterior debridement with interbody bone grafting and posterior instrumented fusion can provide satisfactory results for treating tuberculous spondylitis with psoas abscess in patients with neurological deficits.
Introduction
There has been an increased incidence of tuberculosis throughout the world. Tuberculous spondylitis is the most common form of skeletal tuberculosis and it is the most serious form of tuberculosis lesions in various bones and joints1,2. It is found in approximately 50% of all affected TB patients, and 75% of the cases are accompanied with paraspinal abscess3. Psoas abscesses of a tuberculous origin are seldom or rarely caused by digestive, urologic or genital tuberculosis4.
Antituberculous chemotherapy remains the mainstay of treatment for tuberculous spondylitis because the advent of diagnostic tools has allowed this malady to be detected early before the development of severe deformity and neurological deficit. However, this conservative approach cannot prevent the possible progression of a kyphotic deformity, and long-term rest is usually required to achieve relief from severe back pain5. The placement of a rigid stabilization system may prevent kyphosis and provide immediate relief of the pain that had been caused by spinal instability5-7.
Although various treatment options, including debridement with anterior spinal fusion, anterior spinal fusion with posterior spinal fusion, posterior spinal fusion alone and posterior spinal fusion followed by anterior spinal fusion, have been used for treating spinal tuberculosis2,8,9, there are few reports on the treatment of tuberculous spondylitis with psoas abscess by percutaneous drainage10,11. Moreover, there are no reports on the treatment of tuberculous spondylitis with psoas abscess by anterior and posterior surgery. The aims of our procedure are to remove the infected material and the psoas abscess by anterior surgery, to promote natural wound healing by firm fixation with pedicle screw instrumentation, and to facilitate early ambulation and rehabilitation. We report here on performing anterior and posterior surgery on patients with tuberculous spondylitis with a psoas abscess and we evaluated the treatment outcomes.
Materials and Methods
From March 1997 to February 2006, 22 cases of tuberculous spondylitis with psoas abscess were treated at one institution. Of these, 6 cases underwent percutaneous drainage, 2 underwent anterior surgery only and 14 underwent simultaneous anterior and posterior surgery. This study is a retrospective investigation of the 14 cases that were treated by one surgeon for tuberculous spondylitis with a psoas abscess (Table 1). The study was conducted through a review of the medical records and the patients' follow-up reports. Six cases were women and 8 were men. The mean age of the patients at the time of surgery was 33.6 years (range, 21 to 55), and the mean follow-up period was 34 months (range, 24 to 48). All the cases presented with constitutional symptoms such as weakness, malaise, night sweats and fever with weight loss. Seven cases presented with flank mass. Back pain appeared later in all the cases. The mean duration of the constitutional symptoms was 4.4 months (range, 2 to 8). All the patients demonstrated neurological deficits (Frankel C to D), including motor weakness, sensory changes, pain radiating to the lower extremities and voiding difficulty. Six cases had combined pulmonary tuberculosis. Tuberculous spondylitis was found in T11-L1 in 1 case, in T12-L1 in 3 cases, in L1-2 in 4 cases, in L2-3 in 5 cases and in L3-4 in 1 case. The mean number of levels that spinal fusion was performed was 2.7 (range, 1 to 4).
Surgery was indicated when the neurological symptoms were expressed as a result of granulation tissue, abscess, sequestrated bone or a disc fragment that compressed the dura.
A hematological examination, the Mantoux tuberculin skin test2, simple radiography, radionuclear imaging and magnetic resonance imaging (MRI; T1, T2 and the contrast-enhanced T1 images) were all done prior to surgery for all the cases. The hematological examination included the white blood cell (WBC) count (reference range, 4,000 to 11,000/mL), the erythrocyte sedimentation rate (ESR) (reference range, 0 to 15 mm/hr) and the C-reactive protein (CRP) level (reference range, 0 to 0.5 mg/dL) (Table 2). Preoperatively, a computed tomography (CT) guided fine needle biopsy of the infected disc space was performed in all the cases. The infected disc material and psoas abscess that were removed during anterior surgery were sent for culture and pathologic evaluation.
The simple and dynamic radiographs were obtained for all the patients at 3, 6 and 12 months after surgery and at the final follow-up to evaluate the spinal fusion and the lumbar lordotic angle. The assessment of the spinal fusion and the measurements of the lordotic angle were conducted by two surgeons. Fusion was assessed by the radiological findings, according to the criteria by Lee et al.12 In our study, the definitive and probable fusions were classified as spinal fusion. The kyphotic angle of the spinal lesion was measured from the upper end plate to the lower end plate of the spinal lesion preoperatively, postoperatively and at the final follow-up. The functional outcomes were evaluated according to the Frankel neurological classification13 and the Kirkaldy-Willis criteria14.
1. Operative technique
The patient was placed in the semi-lateral position on the operating table. Removal of the psoas abscess, curettage around the intervertebral disc and anterior interbody arthrodesis with using autogenous iliac bone or a rib graft was performed through the anterior approach. For 2 patients with psoas abscesses in both sides, the curettage was performed in each site. Following the anterior procedure, the patient was turned to a prone position. Posterior fusion with pedicle screw fixation was then performed. When fixing the pedicle screw, we tried not to insert the pedicle screws directly into the infected bodies. When the infection and destruction of the vertebral body was severe, we fixed one level above or below the infected segment. The obtained surgical specimens were sent for pathologic diagnosis and culture for determining the presence of tuberculous bacilli and their chemosensitivity.
2. Postoperative care
In addition to the antituberculous chemotherapy, intravenous antibiotics were given for 5 to 7 days to all the patients after surgery. Ambulation was allowed 3 days after surgery and the patients wore a thoraco-lumbo-sacral orthosis for 3 months. Antituberculous chemotherapy was started 1 week to 3 weeks before surgery for all the cases and this was continued for 12 to 18 months. The standard four-drug therapy with isoniazid (5 mg/kg), rifampicin (10 mg/kg), ethambutol (15 mg/kg), and pyrazinamide (25 mg/kg) was administered as a first-line treatment for 4 months, and this was followed by isoniazid, rifampicin and ethambutol for 12 to 18 months. This treatment was regularly supervised by a pulmonologist.
3. Statistics
Serial changes of the lordotic angle were assessed using Friedman's test along with Dunn's post multiple comparison test. Statistical significance was defined as p-values <0.05.
Results
1. Bony union and change of the kyphotic angle
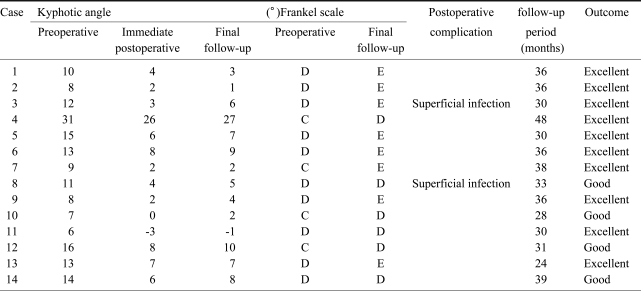
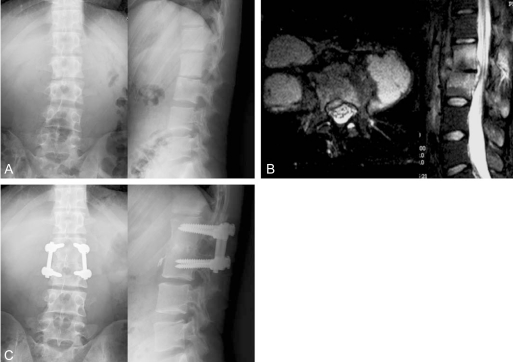
Bony union was observed after 1 year in 14 cases (Figs. 1 and 2). The mean kyphotic angle of the spinal lesion before the operation was 12.4 (range, 31 to 6) and this improved after the operation to 6.1 (range, 26 to -3). At the final follow-up, the mean kyphotic angle was 6.4° (range, 27 to -1) (Table 3). There were statistically significant differences between the preoperative and postoperative kyphotic angles (p<0.001), the postoperative and final kyphotic angles (p>0.05) and the preoperative and final kyphotic angles (p<0.01).
A 21 year-old man developed an L2-3 tuberculous spondylitis with psoas abscesses at both sides (case 1). This patient underwent anterior debridement of both sides and anterior interbody fusion with an autogenous iliac bone graft and posterior instrumentation. The preoperative anteroposterior and lateral radiographs demonstrate L2-3 disc interspace narrowing and irregular end plates (A). The T2-weighted axial and sagittal images reveal psoas abscesses at both sides and an epidural abscess (B). The anteroposterior and lateral radiographs taken 36 months after surgery demonstrate that bony union has been achieved (C).
A 38 year-old man developed T11-L1 tuberculous spondylitis with two psoas abscesses. This patient underwent anterior and posterior surgery (case 4). The preoperative anteroposterior and lateral radiographs demonstrate destruction of the T11-L1 vertebral bodies (A). The contrast-enhanced T1-weighted coronal and sagittal images reveal both psoas abscesses and destruction of the T11-L1 vertebral bodies (B). The anteroposterior and lateral radiographs taken 48 months after surgery demonstrate that bony union has been achieved (C).
2. Clinical courses
For 7 cases, the diagnosis was established by culturing acid-fast bacilli from the materials obtained from the spinal lesions, and for three others it was established by observing acid-fast bacilli on smears. The remaining four patients had negative findings on both the cultures and smears. The Mantoux test was positive for 12 cases. Six cases harbored active pulmonary tuberculosis in addition to their spinal lesions. Typical caseating granulomas were demonstrated histologically for all the cases.
Upon admission, the mean WBC count was 9,944/mL (range, 6,800 to 12,340), the mean ESR was 89 mm/hr (range, 27 to 123), and the mean CRP level was 7.06 mg/dl (range, 4.4 to 11.42). With the normal ESR being 30 mm/hr and the normal CRP level being 1.0 mg/dL, the preoperative ESR was increased in 13 cases (92.9%) and the CRP level was increased in 14 cases (100%). The ESR was decreased after surgery, and this returned to normal for 5 cases by 6 weeks, but not for 9 cases. The ESR returned to normal in 11 cases at the final follow-up. The CRP level was decreased by 6 weeks after surgery, and it returned to normal within 3 months after surgery for all the cases.
Postoperative complications were encountered in 2 cases. Superficial wound infection was observed in 2 cases, and this was successfully treated with dressing changes.
The clinical outcomes were assessed using the Frankel neurological classification13 and the Kirkaldy-Willis criteria14. According to the Frankel classification, 1 case improved by two grades (C to E) and 10 cases improved by 1 grade, while 3 cases demonstrated no changes. The functional outcomes, which were determined using the Kirkaldy-Willis criteria, were excellent for 10 cases and good for 4 cases.
Discussion
In patients with tuberculous spondylitis, a paraspinal abscess generally forms secondary to the destruction of the cortical bone and elevation of the periosteum. If an inflammatory mass penetrates the periosteum, then a psoas abscess may be formed and it may extend through the psoas sheath, following the muscle course to as far as the groin and thigh15. A subacute presentation along with nonspecific signs and symptoms makes the diagnosis of psoas abscess difficult16. Limping, a positive psoas sign, flexion deformity of the hip joint, fatigue, fever, sweating at night and weight loss may be seen17. Psoas abscess can be associated with disseminated tuberculous infection. In this study, there were 6 cases with accompanying pulmonary lesion.
Surgery for tuberculous spondylitis is recommended in the presence of spinal deformity, significant neurological dysfunction, failure of nonoperative management, persistent severe pain and neurological dysfunction that does not resolve or that develops when patients with tuberculous spondylitis undergo antituberculous medication18. In addition, older patients with Pott's disease-related paraplegia require decompressive surgery to avoid the hazards of prolonged immobilization19. Nussbaum et al.20 even recommended surgical treatment for the patients with mild neurological deficits because both epidural infection and bone destruction typically progress for a variable period after antituberculosis chemotherapy is started. In this study, we performed anterior debridement with interbody bone graft and posterior instrumented fusion in all 14 patients.
Various surgical methods have been used to treat spinal tuberculosis, yet there are only a few reports on the treatment of tuberculous spondylitis with psoas abscess10,11. Although percutaneous drainage has been used for the management of tuberculous psoas abscess10,15, it is not sufficient for treating a patient with tuberculous spondylitis and a psoas abscess and who displays a neurological deficit. Combined anterior radical debridement and internal fixation have some advantages over other procedures as the former can directly access and excise the focus of disease, rapid healing is promoted by osseous union and there is a decreased tendency for progressive collapse of the kyphotic angulation21. Although internal fixation for tuberculous spondylitis is safe22-26, the presence of an artificial implant in the inflammatory tissue can induce bacterial attachment and the formation of a biofilm22,27. Posterior fusion combined with rigid instrumentation has been shown to reduce the required amount of intraoperative anesthetic and XXXsurgical demandsXXX and it helps to avoid the possible intra- and postoperative complications that can be associated with the anterior approach28. Guzey et al.5, and Rath et al.29, reported good neurological results after performing posterior debridement and internal fixation in the patients with neurological impairment due to spondylitis. Their results were comparable with the best results obtained after anterior decompression, and this may be explained by the possibility that extended neural decompression is achieved through the posterior approach. However, it was difficult to remove a psoas abscess in Guzey et al.5, and Rath et al.29' patients with using the posterior approach.
In this article, we performed anterior debridement, anterior interbody fusion with an autogenous bone graft (iliac or rib) and posterior instrumentation with pedicle screws. The benefits of these procedures are adequate removal of the infected material, early ambulation because of the firm internal fixation and correction of spinal deformity.
The stability provided by posterior transpedicular fixation securely protects the vertebral correction, and the patients are able to return to activities of daily living within a short period of time. In general, transpedicular screws can be placed in the affected vertebrae if the upper part of the vertebral body is not destroyed by the infection6,8,29. Thus, the extent of spinal fixation can be minimalized. The results of our study demonstrated that tuberculous spondylitis and psoas abscess with neurological deficits could be successfully treated through the anterior and posterior approach by performing meticulous debridement of the necrotic bone and the infected disc and this was followed by a bone graft. Compared with anterior debridement and a strut bone graft, the disadvantage of anterior and posterior surgery is the fact that pedicle screw fixation might be needed on one or two more segments when the vertebral body destruction is severe. However, we thought that the influence of additional segment fixation would not be great because most of our patients returned rather quickly to an active stage of life.
Some potential limitations of this study should be considered. First, the number of patients included was relatively small. In order to reaffirm the utility of simultaneous anterior and posterior surgery in patients who have tuberculous spondylitis with psoas abscess, studies with a larger number of patients should be performed. Secondly, we could not compare the outcome between a single anterior or posterior approach and a simultaneous anterior and posterior approach. Although we performed anterior debridement with an interbody bone grafting and posterior instrumented fusion in this study, further studies concerned with the outcome of a single anterior or posterior approach should be performed.
Conclusions
Our results indicate that anterior debridement with an interbody bone graft and posterior instrumented fusion for treating tuberculous spondylitis with psoas abscess can provide satisfactory results for patients with neurological deficits. This procedure offers the advantage of direct access and excision of the focus of disease, it prevents loss of the normal vertebral alignment and it facilitates early mobilization of the patients. We suggest that anterior debridement with an interbody bone graft and posterior instrumented fusion can be a valuable treatment option for patients who suffer from tuberculous spondylitis with psoas abscess and who also display neurological deficits.