|
 |
- Search
| Asian Spine J > Volume 11(6); 2017 > Article |
|
Abstract
Purpose
Overview of Literature
Methods
Results
Conclusions
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
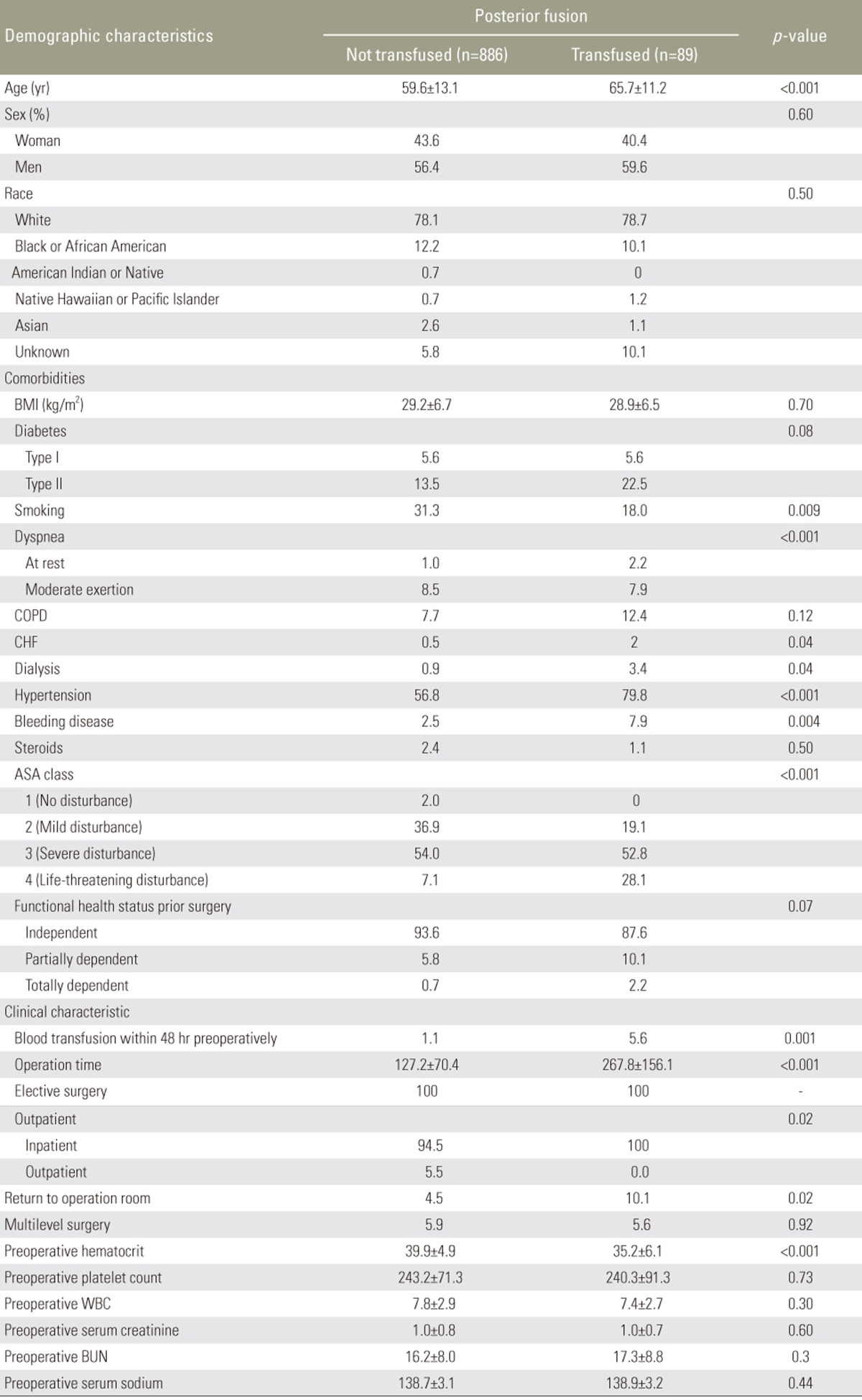
Table┬Ā1
All cervical fusion patients

Values are presented as mean+standard deviation or percentage.
BMI, body mass index; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; ASA, American Society of Anaesthesiologist; ACDF, anterior cervical discectomy and fusion; WBC, white blood cell; BUN, blood urea nitrogen.
Table┬Ā2
Association of blood transfusion with adverse outcomes for all cervical fusion patients
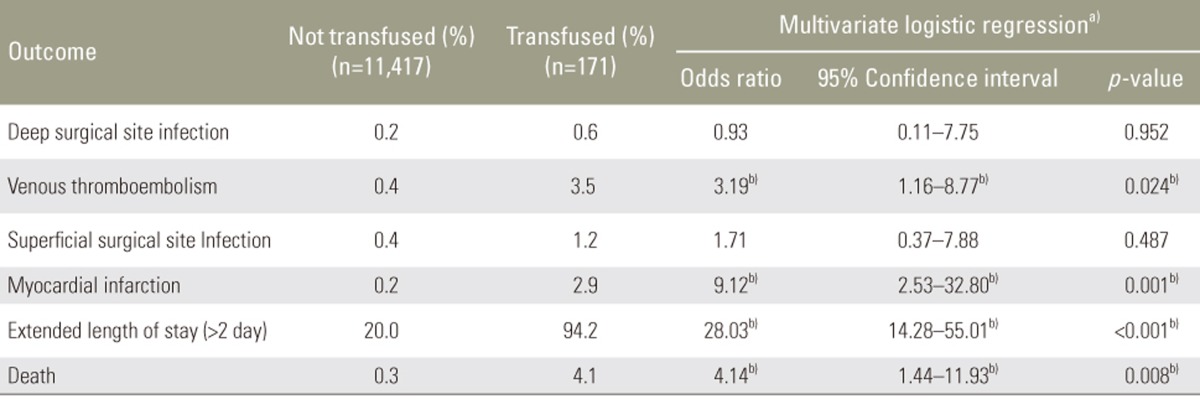
a)Each line represent a separate multivariate logistic regression analysis for each variable and adjusted odds ratio and p-value by controlling for multilevel surgery and surgical approach, as well as all demographics and comorbidities found in Table 1; b)Statistical significance (p<0.05).
Table┬Ā3
Association of blood transfusion with adverse outcomes for all single level cervical fusion patients
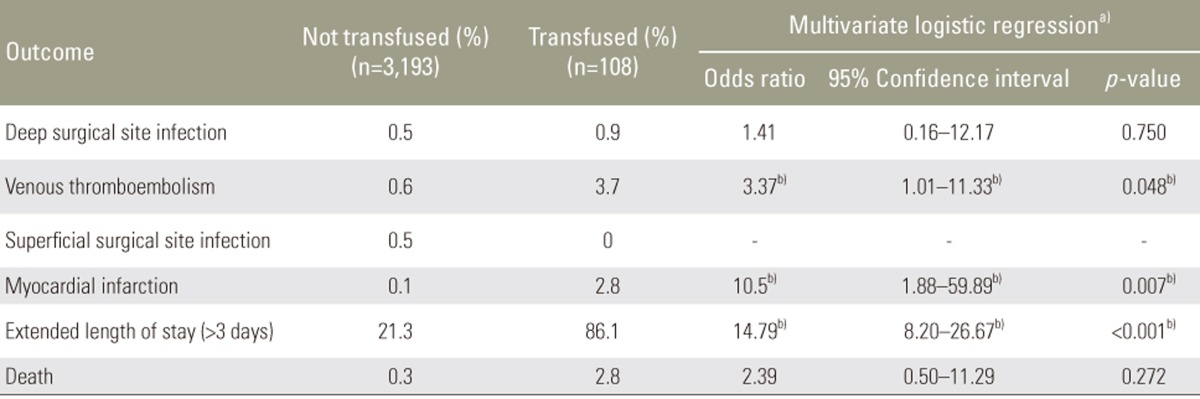
a)Each line represent a separate multivariate logistic regression analysis for each variable and adjusted odds ratio and p-value by controlling for all demographics and comorbidities found in Table 1; b)Statistical significance (p<0.05).
Table┬Ā4
Association of blood transfusion with adverse outcomes for all multi-level cervical fusion patients

a)Each line represent a separate multivariate logistic regression analysis for each variable and adjusted odds ratio and p-value by controlling for all demographics and comorbidities found in Table 1; b)Statistical significance (p<0.05).
Table┬Ā6
Association of blood transfusion with adverse outcomes for all ACDF patients
ACDF, anterior cervical discectomy and fusion; CI, confidence interval.
a)Each line represent a separate multivariate logistic regression analysis for each variable and adjusted odds ratio and p-value by controlling for all demographics and comorbidities found in Table 1; b)Statistical significance (p<0.05).
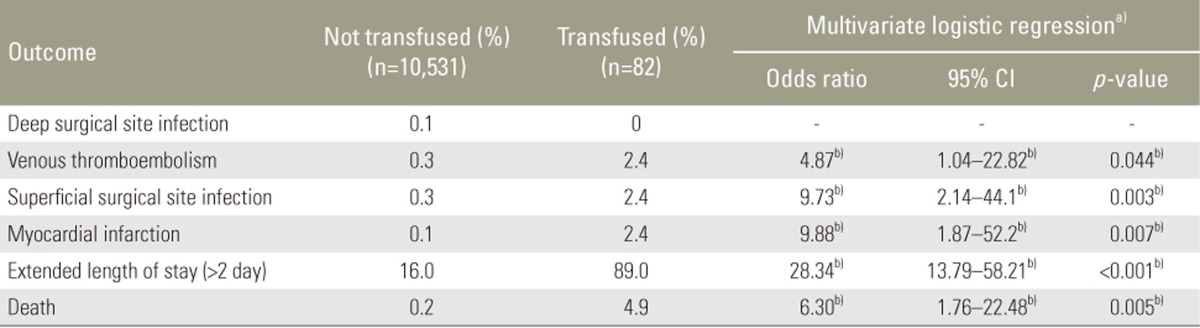
Table┬Ā8
Association of blood transfusion with adverse outcomes for all posterior cervical fusion patients.

a)Each line represent a separate multivariate logistic regression analysis for each variable and adjusted odds ratio and p-value by controlling for all demographics and comorbidities found in Table 1; b)Values in boldface indicate statistical significance (p<0.05).