 |
 |
- Search
| Asian Spine J > Volume 11(4); 2017 > Article |
|
Abstract
Purpose
Overview of Literature
Methods
Results
Conclusions
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
Fig.┬Ā1
Effect of body mass index (BMI), gender and selective serotonin reuptake inhibitor (SSRI) on predicted blood loss based on linear regression analysis. Predicted blood loss was calculated for a fictive patient using linear regression. All other variables were held constant at a mean age of 50 years, mean surgery time of 210 minutes, mean preoperative hematocrit of 42 mg/dL and mean platelet count of 280├Ś103/┬ĄL.
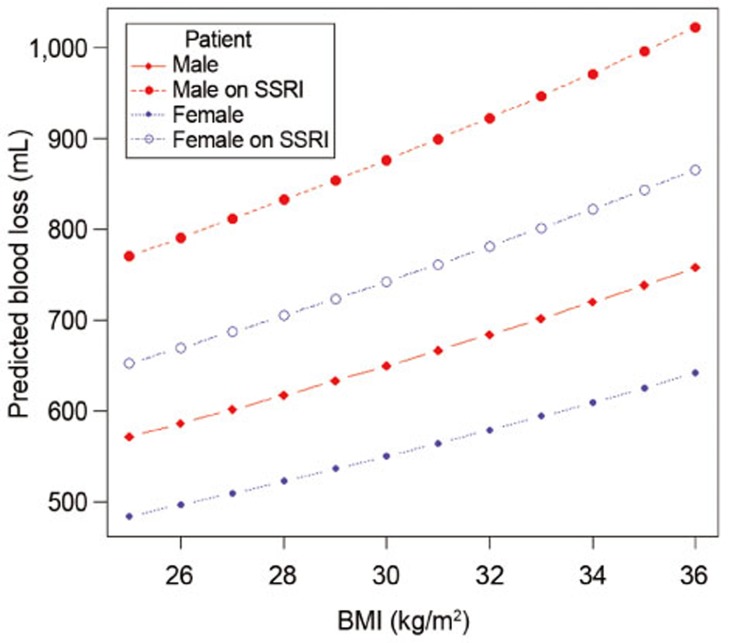
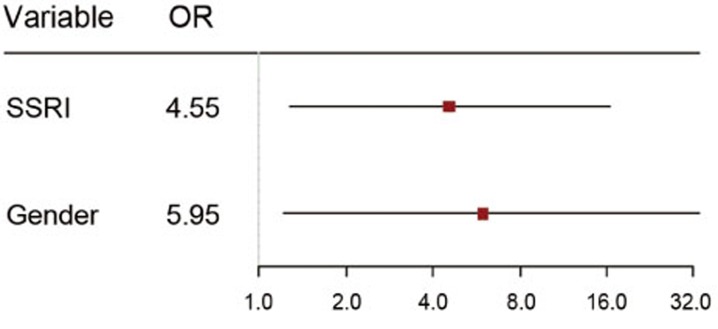
Fig.┬Ā2
Results of weighted logistic regression. The model was weighted using the propensity scores for treatment with selective serotonin reuptake inhibitors (SSRI) based on age, gender, body mass index, hematocrit, and platelet count. The final model was adjusted for gender due to imbalance after weighting. OR, odds ratio.
Table┬Ā1
Characteristics of all patients included in this study (n=235)
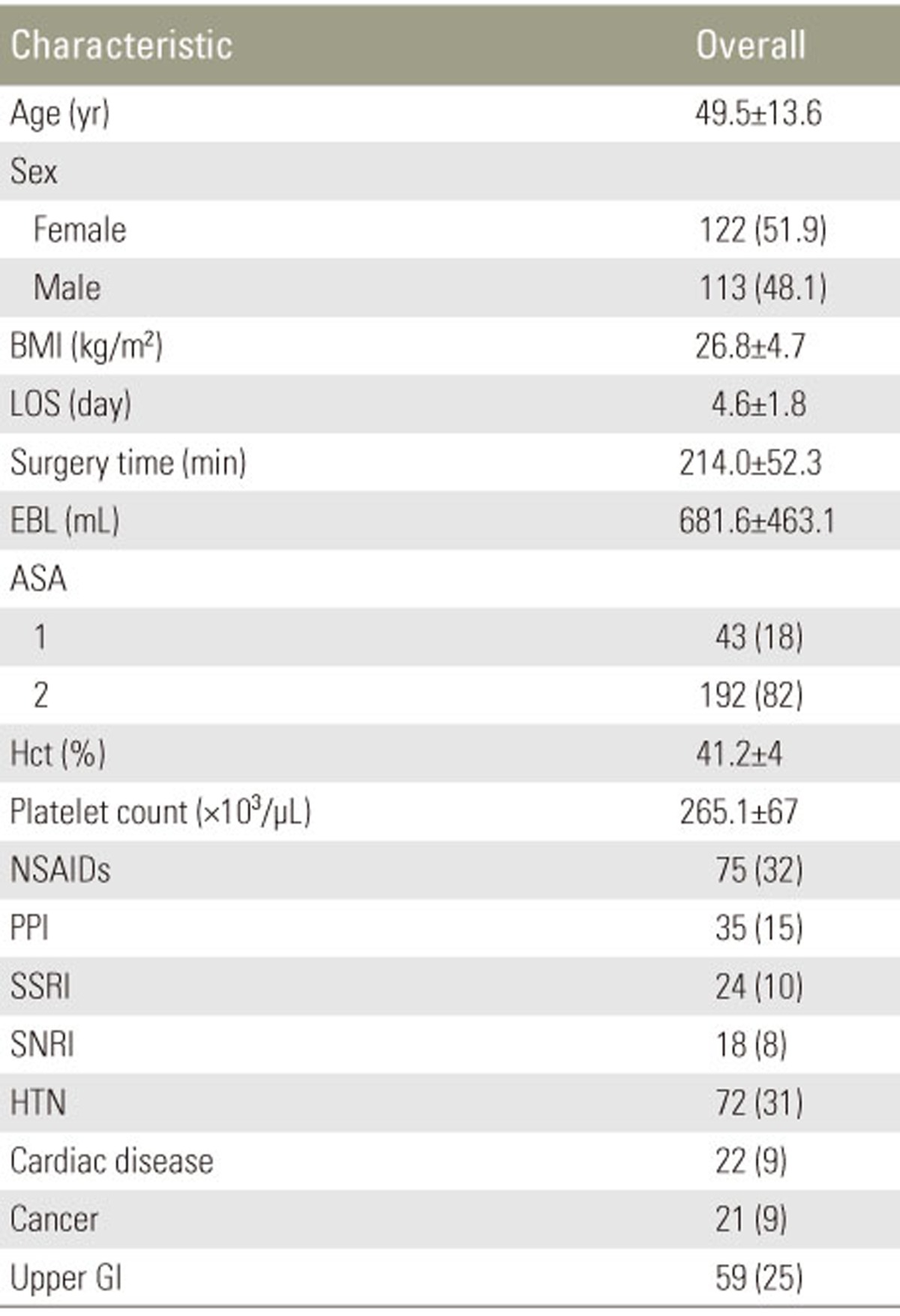
Values are presented as mean┬▒standard deviation or number (%).
BMI, body mass index; LOS, length of stay; EBL, estimated blood loss; ASA, American Society of Anesthesiologists Physical Status Classifications; Hct, preoperative hematocrit in %; NSAIDs: non-steroidal anti-inflammatory drugs; PPI, proton pump inhibitors; SSRI, selective serotonin reuptake inhibitors; SNRI, serotonin norepinephrine reuptake inhibitors; HTN, hypertension; Upper GI, disease of the upper gastrointestinal tract.
Table┬Ā2
Predictor variables for estimated blood loss determined by linear regression analysis
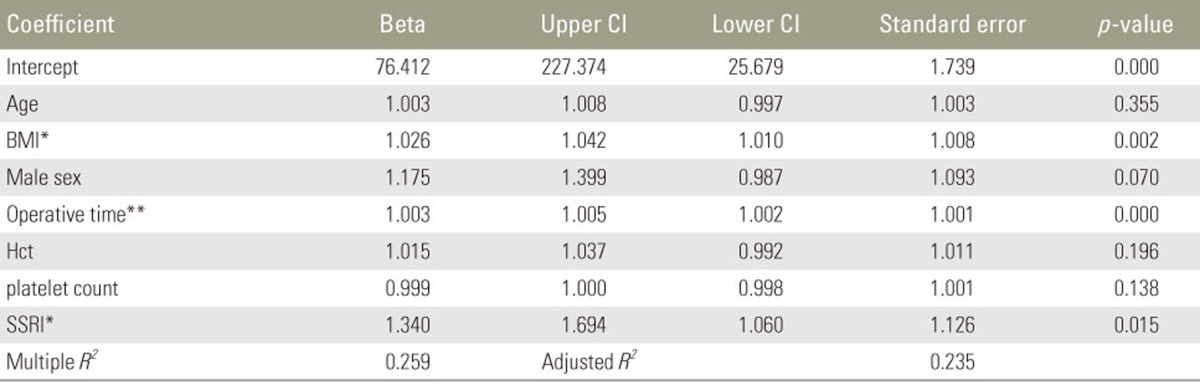
Due to log transformation, exponentiated regression coefficients (beta coefficients) represent the percentage change in blood loss for one unit change in the predictor variable. For example, an increase in 1 unit of body mass index, results in a 2.6% increase in blood loss, while the intake of SSRI is associated with a 34% increase in blood loss. A coefficient greater than 1 indicates an increase, while a value smaller than 1 indicates a decrease.
CI, confidence interval; BMI, body mass index; Hct, preoperative hematocrit; SSRI, selective serotonin reuptake inhibitors.
*p <0.05, **p <0.01.
Table┬Ā3
Characteristics of cases who received an allogenic blood transfusion (n=17) in comparison to controls (n=218)

Values are presented as mean┬▒standard deviation or number (%).
BMI, body mass index; LOS, length of stay; EBL, estimated blood loss; ASA, American Society of Anesthesiologists Physical Status Classifications; Hct, preoperative hematocrit; SSRI, selective serotonin reuptake inhibitors; SNRI, serotonin norepinephrine reuptake inhibitors; PPI, proton pump inhibitors; HTN, hypertension; Upper GI, disease of the upper gastrointestinal tract.
*p <0.05, **p <0.01.
Table┬Ā4
Results of propensity score weighting
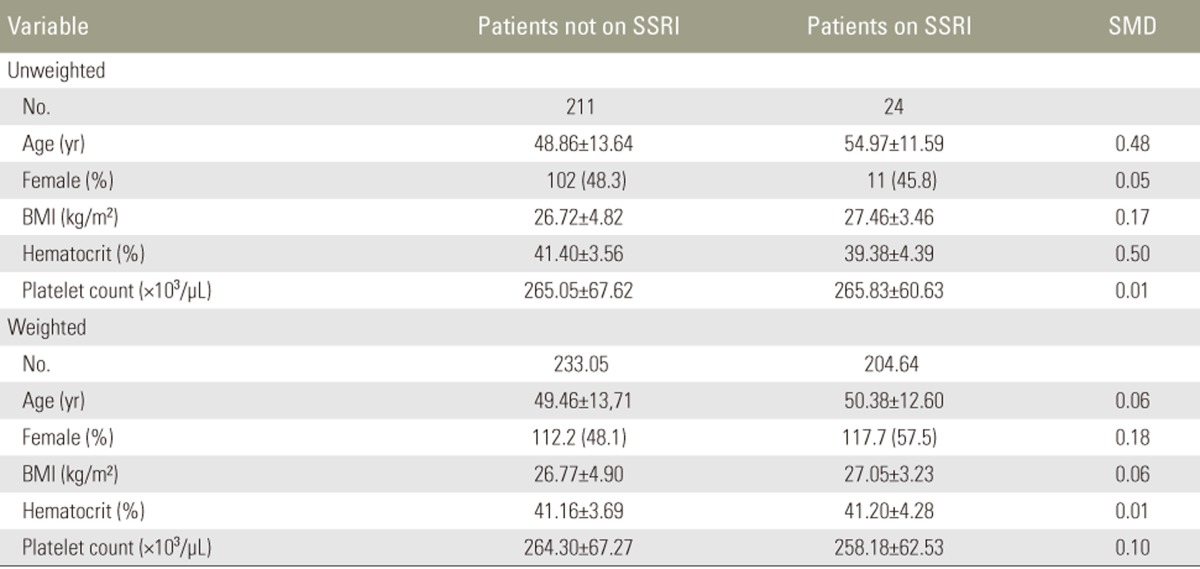
A standardized mean difference of greater than 0.1 indicates imbalance. The variable gender was found to be imbalanced and thus included in the final regression model to adjust for residual confounding.
SSRI, selective serotonin reuptake inhibitors; SMD, standardized mean difference; BMI, body mass index.
Table┬Ā5
Predictive variables for the need of allogeneic blood transfusion determined by logistic regression analysis

The model was weighted for the propensity scores for treatment with selective serotonin reuptake inhibitors based on age, gender, body mass index, hematocrit and platelet count. The final model was adjusted for gender due to imbalance after weighting. An odds ratio greater than 1 means there is an increased risk of transfusion, while values less than 1 indicate a decrease in risk.
OR, odds ratio; CI, confidence interval; SSRI, selective serotonin reuptake inhibitors.
*p -value less than 0.05; **p -value less than 0.01.






