Traumatic Spinal Cord Injury: Long-Term Motor, Sensory, and Urinary Outcomes
Article information
Abstract
Study Design
Retrospective study.
Purpose
To evaluate how motor, sensory, and urinary outcomes of spinal cord injury (SCI) patients were influenced in the long term.
Overview of Literature
SCI is a potentially disabling and devastating neurological outcome that can occur because of spinal column fractures. Most studies have not evaluated or have failed to show the influence of different surgical approaches and other parameters on neurological recovery.
Methods
A thorough history regarding sensory, motor, and urinary complaints was taken from 103 patients with SCI due to vertebral fracture; patients were followed by a thorough neurological examination. Subsequently, all medical records of patients, including neurological state after trauma, trauma mechanism, treatment protocol, surgical protocol, and imaging findings, were evaluated.
Results
Of the 103 patients, 73.8% were survivors of a major earthquake and 26.2% were victims of vehicle accidents; 92.2% patients were surgically treated, while 7.8% underwent conservative management. The mean follow-up duration was 10.3 years. In follow-up visits, 67.0%, 12.6%, 13.6%, and 6.8% patients showed no, partial, substantial, and complete motor improvement, respectively; 68.0%, 26.2%, and 5.8% showed no, mild, and substantial sensory improvement, respectively; and 73.8%, 17.5%, and 8.7% showed no, substantial, and complete urinary improvement, respectively. Logistic regression analysis showed that sex, age at injury time, follow-up duration, trauma mechanism, and stem cell therapy had no effect on motor, sensory, and urinary improvement. Higher initial scores on the American Spinal Injury Association (ASIA) classification, lumbar fracture level, and performance of laminectomy improved motor outcome; higher initial ASIA scores improved urinary and sensory outcomes.
Conclusions
The initial ASIA score is the most important factor for prognosticating motor, sensory, and urinary improvement in SCI patients. Lumbar (L3–L5) and thoracic (T1–T10) fractures have the best and worst prognosis, respectively, in terms of motor recovery. Laminectomy during surgery improves motor function.
Introduction
Spinal cord injury (SCI) is a potentially disabling and devastating neurological outcome that can occur as a result of spinal column fractures. Car accidents, falls, gunshot wounds, and natural disasters are the most common causes of SCI. The treatment of choice for vertebral fractures with SCI, whether complete or incomplete, is surgical reconstruction and instrumented fusion with or without decompression [12].
In the long term, SCI is associated with multiple medical (pressure ulcers, pneumonia, atelectasis, and others), urinary (autonomic dysreflexia, neurogenic bladder, and others), and neurological complications in addition to pain. The chances of neurological recovery and improvement are different in different patients and depend on various factors, including primary neurological state, trauma mechanism, vertebral fracture type and location, and age. Complete SCI, older age, thoracic fractures, and fractures accompanied by dislocations generally follow a more dismal prognosis [34567]. Among all these factors, the extent of neurological deficits (mostly based on the American Spinal Injury Association [ASIA] classification [8]) has been considered the most important predictive factor for functional outcome and prognosis [4]. Of patients with complete SCI early after injury, 5%–20% will experience improvement to some extent [3]; the figure is higher in incomplete lesions, albeit possibly over a very prolonged period after injury [6].
Although it has been shown that there is a better chance of neurological recovery in SCI patients undergoing surgery for vertebral fractures, compared with conservative management [5], most studies have not evaluated or have failed to show the influence of different surgical approaches and other parameters on neurological recovery. Here, we conducted a retrospective analysis of patients suffering from SCI (and cauda equine injury in patients with mid to lower lumbar fractures) after vertebral fracture and assessed their recent urinary and neurological state. The majority of these patients were survivors of a major earthquake in December 2003. The objective of this study was to evaluate how the motor, sensory, and urinary outcomes of these patients had been influenced in the long term by treatment type, surgical procedure, and other factors.
Materials and Methods
The study was conducted in a retrospective cohort design to evaluate the predictor effects of multiple past risk factors on the motor, sensory, or urinary outcomes of patients with SCI. Patients with documented medical records indicating spinal cord or cauda equine injury due to vertebral fracture were visited in July 2014. All the patients were registered in the Welfare Organization of Bam, Iran, an organization with a record of patients with disabilities, including those with SCI. A thorough history regarding sensory, motor, and urinary complaints was taken. The patients then underwent a thorough neurological examination (including motor, sensory, and urinary status) prior to reviewing the medical records. Finally, all medical records of the patients, including their neurological state after trauma, trauma mechanism, treatment protocol, surgical protocol (if performed), and imaging findings were evaluated. Patients with an intact neurological state after trauma, no evidence of vertebral fracture, or missing data were excluded from the study. In patients with multiple contiguous vertebral fractures, the level with the highest imaging indicators of instability that was also consistent with the motor and sensory deficit level was considered as the level of fracture to be incorporated in statistical analysis. Age, sex, trauma mechanism, preoperative and follow-up ASIA scores, preoperative and follow-up urinary status, preoperative and follow-up sensory examinations, level of fractures, and surgical procedure performed were then recorded in a computerized database. The primary outcome measure was the change in motor force, sensory examination, and urinary function. The reexamination, final follow-up evaluations, and data analysis were performed by a neurosurgeon (R.M.L.) who was not involved in the treatment of any of the patients. To reduce any potential bias, data analysis was also performed by the other author (H.S.) who was not involved in any patient examination.
All analyses were performed with PASW ver. 18 package (SPSS Inc., Chicago, IL, USA). Univariate analysis of data was performed by t-test for quantitative measures and chi-square test for qualitative measures. Logistic regression was used for multivariate analysis of the effect of studied parameters on outcome. For all analyses, p-values less than 0.05 were considered statistically significant.
All the patients had provided their consent to participate in the study. The study design was approved by the Ethical Committee of Medical University, and the study was performed with adherence to the statements of the Declaration of Helsinki and regulations of Institutional Review Board.
Results
1. Patient data
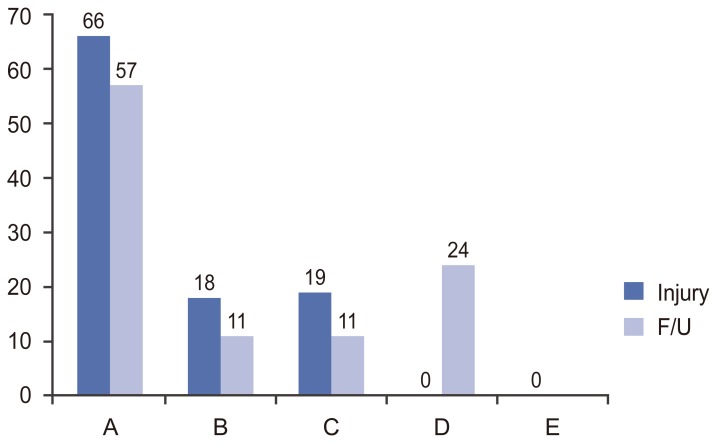
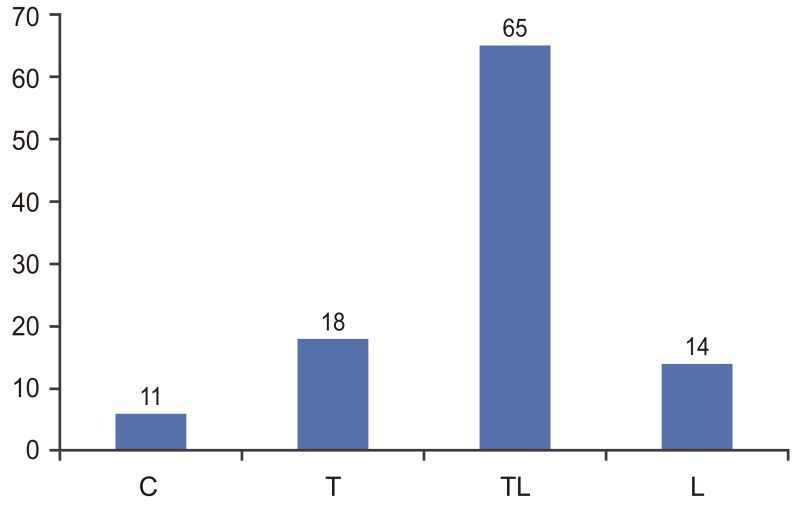
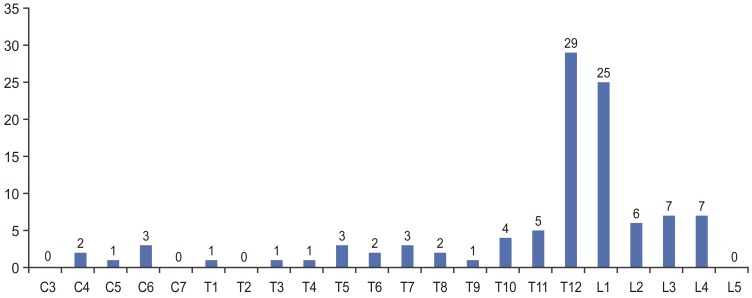
In total, 103 patients were enrolled in the present study. There were 57 females and 46 males, with the mean±standard deviation age at the time of trauma being 28.3±10.5 years (range, 11–55 years). The mean and median time passed since trauma (the follow-up period) was 10.3±2.7 and 11 years, respectively (range, 2–19 years). Most patients (76, 73.8%) were survivors of a major earthquake that had devastated the region in December 2003, while the other 27 (26.2%) were victims of motor vehicle accidents (MVA). The median ASIA score at the time of injury was A (Fig. 1). Fig. 2 displays the fracture levels, the most common being T12 and L1 (29 and 25 patients, respectively), comprising more than half of the patients (52.4%). Although L2, L3, and L4 fractures were observed in six, seven, and seven patients, respectively, there were no L5 fractures. For the ease of statistical analysis, C1–C7, T1–T10, T11–L2, and L3–L5 fractures were classified as cervical (C), thoracic (T), thoracolumbar (TL), and lumbar (L), respectively, and specified as such in the analysis (Fig. 3).
2. Treatment data
After the trauma, all the patients were transferred or referred to other cities due to the lack of surgical facilities in the primary earthquake town at the time of trauma; 95 patients (92.2%) were surgically treated and eight (7.8%) underwent conservative management (including complete bed rest for at least 1 month and immobilization with orthoses). Surgery was performed in eight surrounding cities, all with major academic referral centers. No surgery was performed within the 48 h after the trauma. All the patients underwent multiple sessions of limb physical therapy, as recorded in their medical records.
The surgical procedures included posterior spinal fusion with pedicular screws (PS) in 75 patients and Harrington rods (HR) in 14 and anterior cervical fusion with a cage and plate in six. Of patients with T, TL, and L fractures who underwent PS or HR, 36 (34.02%; all in the PS group) underwent laminectomy in these levels with canal compromise, while 53 did not. Only two patients (1.9%) underwent a neural stem cell transplantation (NSCT) procedure.
3. Follow-up visit data
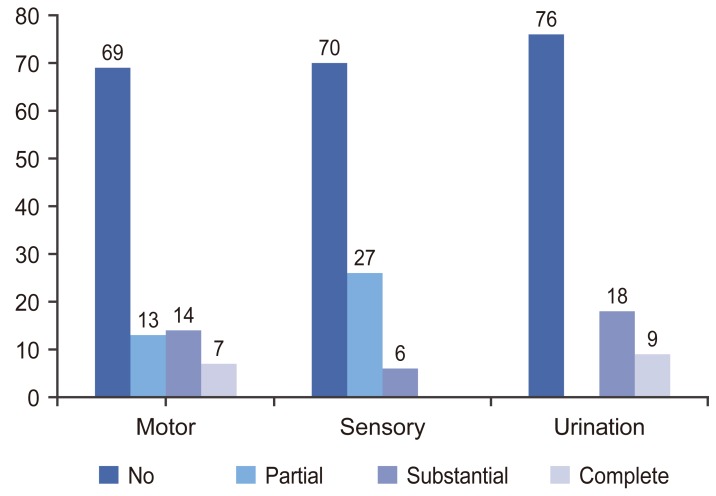
In the follow-up visits, 69 patients (67.0%) showed no change in their motor force, 13 (12.6%) showed partial recovery (less than 5/5 muscle force) in both proximal and distal muscle groups (defined here as partial improvement), 14 (13.6%) showed complete (5/5) proximal but partial distal recovery (substantial improvement), and seven (6.8%) showed complete recovery (complete improvement) in all the muscle groups. In terms of sensory improvement, 70 patients (68.0%) showed no change 27 (26.2%) showed a 1–3-level decrease in the sensory level (partial improvement), and six (5.8%) showed substantial improvement. There were 76 patients (73.8%) with no change in urinary function (no urinary sensation and completely or intermittently dependent on catheterization), 18 (17.5%) showed improved urinary function (defined as substantial improvement), and nine (8.7%) showed complete recovery (normal urination, no need for catheterization, and multiple records of normal urinary ultrasonography) (Fig. 4). The median ASIA score at the time of follow-up visits was still A; however, it had significantly improved from the time of injury (p<0.001) (Fig. 1). The percentage of patients with any degree of motor, sensory, and urinary improvement within each ASIA grade is shown in Fig. 5; there was a significant prognostic effect of the ASIA grade on each function improvement (p<0.001 for all three comparisons). Further analysis showed that in terms of the occurrence and extent of motor recovery, there was an ordinally significant difference between all three ASIA grades (C>B>A) (p<0.001 for all comparisons). However, in terms of sensory and urinary recovery, only grade C was superior to both the groups (p<0.001) and there was no significant difference between A and B (p>0.99).
4. Effect of study variables on motor outcome
Logistic regression analysis showed that sex, age at injury time, follow-up time duration, trauma mechanism, and NSCT had no effect on motor improvement (p=0.99, p=0.99, p=0.58, p=0.74, and p=0.23, respectively), while better postinjury ASIA grades, fracture level, and performance of laminectomy were significantly linked to improved motor outcome (p<0.001, p=0.005, p=0.04, and p=0.04, respectively). The highest influence (odds ratio) was observed in case of the initial ASIA score, followed by fracture level and laminectomy. Among fracture levels, the best outcome was observed in L, followed by C and TL, while the worst outcome was observed in T.
5. Effect of study variables on sensory outcome
Similar to the influence on motor outcome, this analysis showed that sex, age at injury time, follow-up duration, and trauma mechanism had no effect on sensory improvement (p=0.35, p=0.56, p=0.92, and p=0.97, respectively); in addition, fracture level, performance of laminectomy, and NSCT had no effect (p=0.82, p=0.69, and p=0.99, respectively). Only better postinjury ASIA scores significantly improved sensory outcome (p<0.001).
6. Effect of study variables on urinary outcome
Sex, age at injury time, follow-up time duration, trauma mechanism, fracture level, performance of laminectomy, and NSCT had no effect on urinary improvement (p=0.51, p=0.70, p=0.64, p=0.26, p=0.63, p=0.28, and p=0.83, respectively). However, both preinjury and postinjury ASIA scores were related to improved urinary outcome, with the initial ASIA score showing A greater influence (p<0.001 and p=0.005, respectively).
Discussion
SCI is a potentially disabling and devastating neurological outcome of spinal column fractures that is associated with a high social and economic burden for the patient, family, and healthcare system. Moreover, it most often involves the patients in their most productive period of life. The burden of the disease is highly related to the extension (number of limbs involved), severity (partial vs. complete), and total duration of paralysis.
Different values have been reported for the recovery rate, and the extent of recovery has been shown to differ depending on each patient's condition. The most important factors predicting the extent of recovery are the primary neurological state, location of injury within the spinal cord, trauma mechanism, vertebral fracture type and location, and patient age [34567].
The ASIA score early after trauma is reported to be the most important factor predicting the chance of motor recovery [4]. It is one of the most accepted and used classifications for the extent of neurological deficits after SCI and classifies patients from A (complete motor and sensory injury) to E (normal neurological state) [8]. In general, the rate of neurological recovery in patients with grade A impairment has been reported to be around 25%–45%, while the value has been reported to be as high as 65%–75% for patients with incomplete injuries (grade C and D) [349].
This study included 103 patients with spinal fractures complicated by different grades of SCI (ASIA A to C). None of the patients belonged to grade D (relatively mild SCI) or E (neurologically intact) groups. The mean follow-up duration of the patients was more than 10 years, one of the longest periods for SCI patients reported in the literature. None of the patients with grade A impairments after trauma showed motor improvement, while all patients with grade B and C impairments showed improvement by atleast one grade. In addition, the extent of motor improvement was greater in grade C patients. In contrast, patients with grade A and B impairments had an identical poor prognosis in terms of sensory and urinary improvement, patients with grade C impairments showed a much more positive outcome (more than 85% chance of improvement). This was supported by the finding that the postinjury ASIA score, in other words, the neurological state after trauma, is the most important prognostic factor for motor, sensory, and urinary outcomes, a finding showing clear agreement with previous results.
Performing laminectomy at the time of surgery was another factor positively influencing motor improvement. Although it has been shown that in SCI patients with vertebral fractures, there is a better chance of neurological recovery in those undergoing surgery than in those receiving conservative management [510], most studies have not evaluated or have failed to show the influence of different surgical approaches and other parameters on neurological recovery. The role of decompression at the time of surgery also remains controversial. For instance, in a series of 23 patients with SCI after TL fractures who did not undergo decompression at the time of fusion, Miyashita et al. showed imaging evidence of canal remodeling in all the patients. However, their series lacked a control group with decompression to compare the results [11]. In contrast, some other studies have favored a role of laminectomy in fusion procedures in patients with different degrees of SCI [212]. The latter studies also include case series without nondecompression control groups. The results of the present study, however, have provided evidence of better long-term motor outcomes with laminectomy or “decompression.”
Another factor that influenced long-term motor outcome but not sensory and urinary outcomes in this study was fracture and injury locations. The best outcome was observed for lumbar (L3 and below) fractures, and the worst outcome was observed for thoracic fractures (T1–T10). Moreover, none of the patients had a L5 fracture, which may indicate a low potential for neurological compromise at this level. These results are in accordance with those of previous studies showing worse outcomes for thoracic fractures. Thoracic spine injuries (excluding T11 and T12 levels as these are considered to have a more favorable outcome) have even shown a lesser potential for neurological recovery [4] than cervical injuries that have a better outcome [9]. This may be justified by the absence of a spinal cord in the lumbar vertebra, leading to a better chance of recovery.
The present study has some limitations. First, it is retrospective, making the interpretations less exact. However, a prospective design with such a long follow-up period is extremely difficult, if not impossible, to complete. This retrospective design, however, has the advantage of providing at least 10 years of follow-up time for evaluating the influence of variables.
Second, the patients' exact neurological state in the time of injury are less reliable because the initial examinations were performed by different examiners in different patients in different cities. In contrast, the follow-up examination of each patient was performed by one physician only.
Third, different centers with probably non-unified treatment protocols were involved in the treatment of the patients. Fourth, and perhaps the most important limitation is that none of surgical procedures was performed in the early post-trauma period; 92.2% of the studied patients were surgically treated after transfer or referral to other medical centers. Many authors favor the role of early surgery for improved motor outcomes, particularly within 24 hours [1314].
The reason for the latter two limitations was that the majority of the study population (approximately three quarters) consisted of survivors of a major earthquake occurring in the city (Bam, Iran) in December 26, 2003, resulting in more than 25,000 mortalities and 30,000 morbidities. The survivors, spending many hours or even days under collapse, were then transferred to eight other cities as the medical infrastructures of the city had been destroyed. For the same reason, the other group of subsequent patients, the MVA victims, had also been transferred to other cities over many years because of the lack of high-standard neurosurgical facilities in the city. Thus, none of the studied patients underwent surgery within 48 hour following trauma and the role of time-to-surgery on functional outcome could not be evaluated. Moreover, delayed surgeries may obfuscate the results and affect the studied variables.
Conclusions
In conclusion, the results of our study indicate that the initial ASIA score is the most important factor prognosticating motor, sensory, and urinary improvement in SCI patients. Performing laminectomy during surgery also favorably influences motor improvement in these patients. Lumbar (L3–L5) fractures show the best prognosis and thoracic fractures (T1–T10) show the worst prognosis in terms of motor recovery.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.