One-Stage Anterolateral Debridement, Bone Grafting, and Internal Fixation for Treating Lumbosacral Tuberculosis
Article information
Abstract
Study Design
Retrospective case series.
Purpose
To investigate the clinical efficacy and feasibility of one-stage anterolateral debridement, bone grafting, and internal fixation for treating lumbosacral tuberculosis.
Overview of Literature
There has been no consensus regarding the optimal means of treating lumbosacral tuberculosis. The one-stage anterolateral extraperitoneal approach for radical debridement, bone grafting, and internal fixation for treating lumbosacral tuberculosis is rare in literature.
Methods
Twenty-one patients with lumbosacral tuberculosis were retrospectively analyzed. All patients underwent the surgery of anterolateral debridement after regularly antituberculous drugs therapy. We evaluated the erythrocyte sedimentation rate, C-reactive protein, radiography, computed tomography, magnetic resonance imaging, visual analogue score, and Oswestry disability index before and after surgery.
Results
All patients completed a follow-up survey 9–48 months after surgery. All patients' wounds healed well without chronic infection or sinus formation, and all patients with low-back pain reported relief after surgery. All cases had no tuberculosis recurrence. Solid bony fusion was achieved within 6–12 months. At final follow-up, evaluated the erythrocyte sedimentation rate decreased from 38.1±12.5 to 11.3±7.1 mm/hr, C-reactive protein decreased from 6.2±4.2 to 1.6±1.3 mg/dL, the visual analog scale score decreased from 4.6±1.1 to 1.4±1.0, the Oswestry disability index score decreased from 50.2%±11.9% to 13.0%±6.6%, and the lumbosacral angle increased from 20.0°±4.8° to 29.0°±3.9° (p<0.05).
Conclusions
One-stage anterolateral debridement, bone grafting, and internal instrument fixation for treating lumbosacral tuberculosis is safe and effective.
Introduction
Spinal tuberculosis (TB) is one of the most common forms of extrapulmonary TB, accounting for approximately 50% cases of musculoskeletal TB [12]. However, lumbosacral segment TB is rare and only accounts for 2%–4% cases of spinal TB [34]. TB spondylitis of the lumbosacral region has rarely been documented in the literature. The treatment of lumbosacral segment TB is difficult, and each patient needs individual consideration [56]. To date, there is a lack of consensus regarding the optimal therapeutic modality for treatment of lumbosacral segment TB.
Antituberculous treatment remains the cornerstone of therapy for spinal TB [7]. However, surgery may be required in selected cases, such as those with large abscesses, severe kyphosis, progressive neurological deficit, or lack of response to medical treatment. Various surgical approaches have been suggested for treating spinal TB, including debridement with anterior spinal fusion, anterior spinal fusion with posterior spinal fusion, posterior spinal fusion alone, and posterior spinal fusion followed by anterior spinal fusion [89]. Despite this, there was still controversy regarding the optimal surgical approach for treating lumbosacral segment TB. Anterior radical resection and bone grafting is a very important technique because it allows direct access to the affected vertebral segments and allows the surgeon to perform radical surgical debridement of the infected tissues [1011]. Anterior approaches for lumbosacral TB include the extraperitoneal and transperitoneal approaches. The effective surgical approaches and methods for lumbosacral TB are controversial. Because the anatomy of lumbosacral segment is unique, the anatomy of the structures surrounding the lumbosacral segment is complicated and performing procedures in this area is difficult. One-stage anterolateral extraperitoneal approach for radical debridement, bone grafting, and internal instrument fixation for treating lumbosacral segment TB is rare in literature. Hence, the purpose of this clinical study was to evaluate the clinical efficacy and feasibility of the anterolateral extraperitoneal approach for treating lumbosacral TB.
Materials and Methods
1. Clinical data
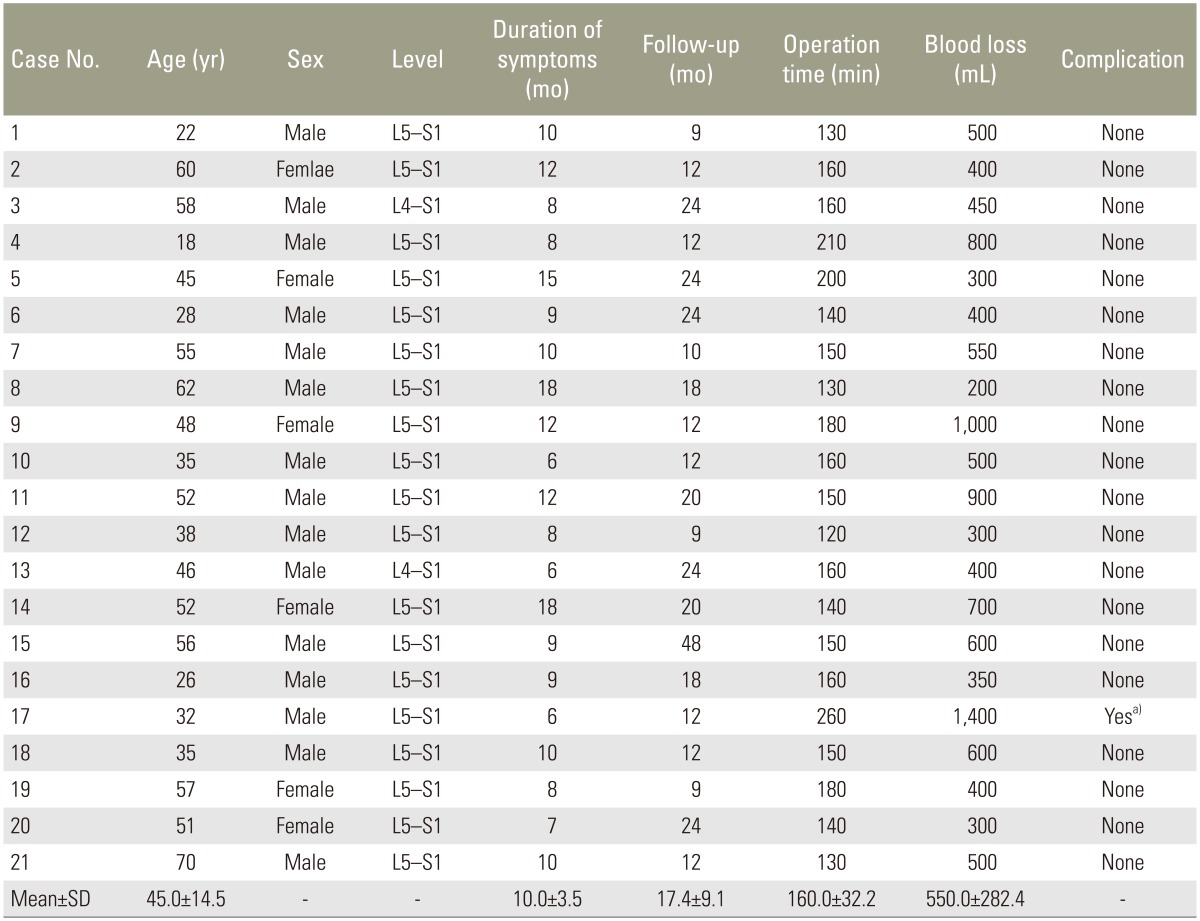
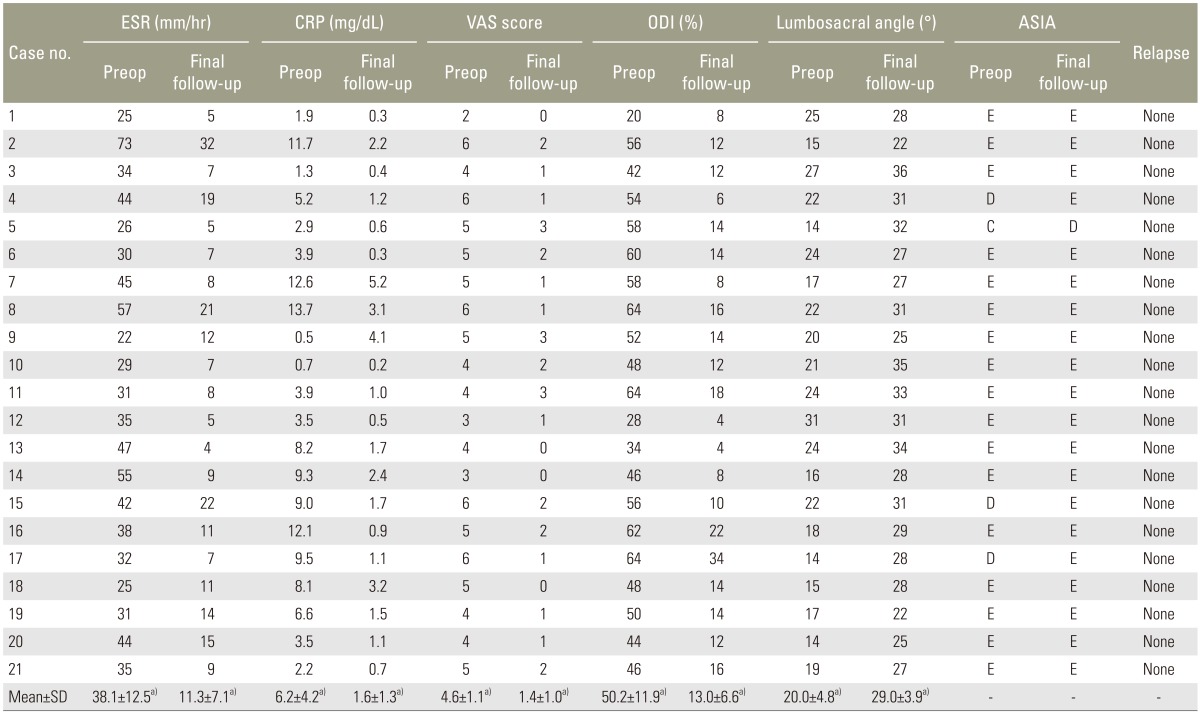
Between May 2008 and May 2013, 21 patients with lumbosacral segment TB were treated in our hospital by the same surgeon. The subjects consisted of 15 men and six women with a mean age 45.0±14.5 years (range, 18–70 years). The duration of clinical symptoms ranged from 6 to 18 months (average, 10.0±3.5 months) (Table 1).
All patients had different degrees of low-back pain as the primary symptom. Fourteen patients presented with clinical signs of TB infection, including low-grade fever, night sweats, loss of weight, and asthenia. Four patients had concurrent neurological disabilities. The American Spinal Injury Association (ASIA) impairment scale was used to evaluate neurological dysfunction. One patient grade-C dysfunction and three had grade-D dysfunction.
All patients underwent plain radiography, computed tomography (CT), magnetic resonance imaging along with measurements of the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Imaging revealed osteolysis in the L4–S1 region (Fig. 1). The lumbosacral angle ranged from 14° to 31° (average, 20.0°±4.8°). ESR ranged from 22 to 73 mm/hr (average, 38.1±12.5 mm/hr) and CRP ranged from 0.5 to 13.7 mg/dL (average, 6.2±4.2 mg/dL). The visual analogue score (VAS) and Oswestry disability index (ODI) were used to evaluate low-back pain and spinal disability. The VAS score ranged from 2 to 6 (average, 4.6±1.1) and ODI score ranged from 20% to 64% (average, 50.2%±11.9%) (Table 2).
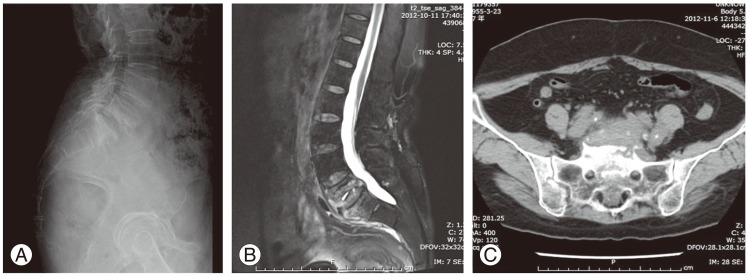
(A) Lateral plain radiographs of the lumbosacral region shows destruction of L5, S1 vertebral bodies. (B) Magnetic resonance imaging shows tuberculosis at L5–S1 segment and paravertebral abscess formation. (C) Computed tomography shows the osteolysis in the L5 and S1 vertebrae.
2. Preoperative preparation
All patients were given antituberculous drugs, including isoniazid (300 mg/day), rifampicin (450 mg/day), pyrazinamide (1,500 mg/day), and ethambutol (750 mg/day) for 3–4 weeks before surgery. ESR and CRP levels were measured to monitor antituberculous efficacy. In addition, a comprehensive assessment of the heart and pulmonary function was performed, and hypoalbuminemia was treated before operation.
3. Operative procedure
The patients were placed in the lateral position after general endotracheal anesthesia. All patients underwent surgery through an anterolateral extraperitoneal approach to the spine. Generally, the incision was made from the side where the vertebral bodies were severely damaged or the side of obvious abscess formation. Peritoneum that was protected by wet gauze was pushed forward in front of the iliacus muscle. The TB foci in L4–S1 and the vessels around lumbosacral vertebral bodies were exposed. Under C-arm fluoroscopy guidance, the damaged vertebrae were located. Iliolumbar vein and ascending vein were ligated to avoid tearing of iliac veins through excessive retraction. Subperiosteal dissection was executed to protect the common iliac vein and paravertebral soft tissue. After exposure, curettes and rongeurs were used to remove lesions, including sequestrae, abscesses, caseous material, and granulation tissue until the normal bleeding bone was exposed. The spinal canal was decompressed if there was any space-occupying lesion. The abscesses were drained and necrotic tissue was curetted as thoroughly as possible. The operative field was then washed with copious amounts of saline until the washing liquid was clear. A part of iliac crest was resected for autologous bone strut grafting and to facilitate the installation of internal fixation. The screws were inserted through the lateral aspects of the vertebral bodies to the bony cortex of the other side. Correction of spinal deformity was accomplished by installing the internal instrument with appropriate distraction. The spinal defect was then measured and the gap was repaired with a suitable length of autologous bone graft harvested from the ilium. The rods were applied lateral to the vertebral bodies and the bone graft was immobilized with appropriate compression. After careful hemostasis, 500 mg of isoniazid and 1,000 mg of streptomycin were placed in the operative area, and a drainage tube was inserted before suturing the incision.
4. Postoperative treatment
The drainage tube was left in place for 48–96 hours. The drainage tube was removed when the volume of drainage was <50 mL over a 24-hour period. Passive movements and functional limb exercises were carried out as early as possible. Conventional antituberculous pharmacotherapy was administered with isoniazid (300 mg/day), rifampicin (450 mg/day), pyrazinamide (1,500 mg/day), and ethambutol (750 mg/day) for 3 months after surgery, which was followed by isoniazid (300 mg/day), rifampicin (450 mg/day), and ethambutol (750 mg/day) for another 9–15 months. Patients were instructed to undergo routine blood examination to monitor ESR and CRP levels as well as liver and kidney functions. Patients were advised bed rest for a minimum of 6 weeks. Active and actively assisted exercises were advised. Complete extension exercises of abdominal, sacrospinal, iliopsoas, gluteus maximus, gluteus minimus, hamstring, quadriceps muscles as well as specific and resistive exercises of oblique abdominal muscles were prescribed. Exercises for augmenting respiratory capacity were also given. Mobilization was started after 6 weeks under external brace support. All patients wore braces for 6 months.
5. Follow-up assessment
We surveyed the wound healing rate and the recurrence rate of spinal TB. VAS and ODI scores were used to assess pain and spinal disability before and after surgery. ESR and CRP tests were used to monitor the antituberculous therapeutic efficacy and therapeutic reaction. Lumbar plain radiographs and/or CT examinations were performed to assess the lumbosacral angle correction and bony fusion. Achievement of union was determined by the formation of continuous bony trabeculae between the graft and host bone [12]. Neurological function was assessed using the ASIA classification before and after surgery. Evaluations of VAS, ODI, ESR, CRP, plain radiographs, and ASIA score were performed at 3, 6, 9, and 12 months after surgery. CT scans were performed at 6, 9 or 12 months after surgery.
6. Statistical analysis
A paired t-test was used to analyze ESR, CRP, VAS score, ODI score, and lumbosacral angle between preoperative and final follow-up values. p<0.05 indicated statistical significance. We used SPSS ver. 17.0 for Windows (SPSS Inc., Chicago, IL, USA) for all statistical calculations.
Results
The mean duration of surgery was 160.0±32.2 minutes (range, 120–260 minutes) and the mean volume of blood loss was 550.0±282.4 mL (range, 200–1,400 mL) (Table 1). One patient had the complication of iliac vein tear during surgery. The rest of patients had no complications, neural disabilities, or ureteral injuries. All males were free of complications of erectile dysfunction and retrograde ejaculation. All patients' wounds healed well without chronic infection or sinus formation, and all symptoms of low-back pain were relieved after surgery. Patients complied with the follow-up survey for 9–48 months. All cases were cured, and no relapses were documented during the follow-up period. All patients obtained bony fusion within 6–12 months after surgery (average, 7.6±2.0 months) (Fig. 2). Four patients had evidence of neurological impairment before the operation. At the final follow-up assessment, the neurological status of the four patients with preoperative neurological deficit was: one with grade C recovered to grade D, three with grade D recovered to grade E.

(A) Anteroposterior and lateral plain radiographs after surgery reveals that the fixation is in a good position. (B) Anteroposterior and lateral plain radiographs reveal bony union 9 months after surgery. phics and operation information
The average ESR was 38.1±12.5 mm/hr preoperatively, which dropped to 11.3±7.1 mm/hr (p<0.05). The average CRP was 6.2±4.2 mg/dL preoperatively, which declined to 1.6±1.3 mg/dL (p<0.05). The VAS and ODI scores before surgery were 4.6±1.1 and 50.2%±11.9%, respectively, which decreased to 1.4±1.0 and 13.0%±6.6% (p<0.05). The average lumbosacral angle was 20.0°±4.8° preoperatively, and this increased to 29.0°±3.9° (p<0.05) (Table 2).
Discussion
Although spinal TB is a medical disease and antituberculous pharmacotherapy has a main role in the recovery of patients, surgical procedures need to be performed when patients develop large soft-tissue abscesses, cord or radicular compression, highly destructive lesions producing spinal bone instability, or severe pain without relief under medical treatment. Surgical treatment of spinal TB can result in spinal stabilization and early mobilization. Surgery can also facilitate the success of chemotherapy, because the abscess cavity provides an avascular environment that protects TB bacilli from systemic antibiotics, and local sclerotic bone prevents permeation of antibiotics [131415]. Thus, we propose that surgical intervention should be performed for treating lumbosacral TB with abscess formation, severe vertebral destruction, neural dysfunction, or unsuccessful conservative treatment. All the necrotic tissue should be debrided, the abscess cavity should be destroyed, and the sclerotic bone should be removed during surgery. Consequently, the risk of spinal TB relapse will be low, and the effect of antituberculous pharmacotherapy will be enhanced. In the end, all the patients in our study who underwent radical debridement were cured and no relapse has been reported.
The conventional surgical approach to lumbar and sacral vertebral TB is posterior instrumented fixation and deformity correction followed by anterior debridement and fusion with bone grafting. However, spinal TB mainly affects the anterior and middle vertebral columns, leading to vertebral bone defects, collapse, compression, and kyphosis. Anterior-column and middle-column damage accounts for 98% cases of spinal TB, while the posterior-column structure usually remains intact [16]. Biedemann [17] found that in an intact vertebral column, 80% load is transmitted through the anterior column and 20% through the posterior column. Therefore, we suggest that the anterior approach is the preferred solution for lumbosacral TB.
Because anterior debridement and arthrodesis for treating spinal TB was reported by Hodgson and Stock [18], several surgeons have advocated this procedure and emphasized its advantages as reaching the focal point of the disease directly, enabling effective debridement of the lesion, and decompression of the spinal cord. However, radical debridement can produce spinal instability. Therefore, anterior strut grafting and instrumentation should be preferred in cases with spinal instability [9]. The anterolateral approach is our surgeons' preferred method as well, although different approaches have their own advantages and disadvantages [192021222324]. In our study, all patients underwent one-stage anterolateral extraperitoneal approach for radical debridement, lateral autologous strut grafting, and single screw–rod instrumentation for lumbosacral TB. The anterolateral approach can achieve direct visualization of the TB focus and facilitate direct debridement and bone grafting. In addition, the lumbosacral debridement using this approach is more complete. Although the recurrence rate for skeletal TB is approximately 2% [7], there was no relapse in the light of complete debridement and multidrug therapy in our study. The extraperitoneal approach can prevent the development of intra-abdominal TB infections and decrease the impact on abdominal organs. In this study, there were several patients with temporary abdominal distension and constipation after surgery. All postoperative complications were relieved after symptomatic treatment. With the anterolateral extraperitoneal approach for lumbosacral TB, the surgeon can achieve debridement, bone grafting, and internal fixation at the same time. There was no need to change the patients' position during surgery, shortening the operative duration and decreasing blood loss. Anterolateral instrument and strut grafting can preferably correct the lumbosacral deformity and at the same time immobilize the bone autograft. The average lumbosacral angle was (20.0°±4.8°) before surgery, and this improved to (29.0°±3.9°) at follow-up. Studies have shown a direct correlation between a decrease in normal lordosis of the lower lumbar and lumbosacral spine with the severity of low-back pain. In this paper, the low-back pain was ameliorated immediately after the patients' lumbosacral angle was increased to its optimal state; all patients' low-back pain improved after correction of the lumbosacral angles that would alleviate shear stress in the juncturae lumbosacralis. There was no migration of the bone autograft after anterolateral internal fixation, and there was no looseness or fracture of the internal instruments during the follow-up period. We conclude, therefore, that one-stage anterolateral debridement, bone grafting, and internal fixation for treating lumbosacral TB is safe and feasible.
Of note, all postoperative patients need to stay in bed for a minimum of 6 weeks. Following that, patients need to be on an external brace for 6 months. Early ambulation is not conducive to spinal stability. However, there are many complications of prolonged bed rest, such as hypostatic pneumonia and thrombus formation in the lower-extremity veins. All patients, wearing an external brace, should stare exercises 6 weeks after surgery. The potential benefits of wearing the brace include limiting spinal range of motion, correcting posture and deformity, preventing gross trunk motion, decreasing force exerted by trunk muscles, providing soft-tissue massage and heat, and improving spinal proprioception [25]. Moreover, bracing is helpful for treating low-back pain. Calmels et al. [26] proposed bracing for the short-term management of subacute low-back pain. Although there is no evidence regarding the effect of lumbar bracing on the rate of lumbar spinal fusion or functional outcome, several authors have advocated the use of brace therapy following lumbar fusion surgery [27].
Our experience with the anterolateral extraperitoneal approach for lumbosacral TB is as follows: (1) patients are placed in the lateral position and the lower extremity of the operational side is flexed to avoid stretch injury to the lumbar nerve root. (2) The iliolumbar vein and ascending vein are ligated before debridement to avoid iliac vein tears and massive hemorrhage. (3) Surgeons should avoid excessive pulling of soft tissue around the anterolateral vertebral bodies; otherwise, this will cause iliac vein or sympathetic trunk injury. (4) The iliac wing needs to be resected to facilitate the installation of internal instruments before embedding the vertebral screws.
The anterolateral extraperitoneal approach for lumbosacral TB has many advantages, but this approach also has a few limitations that should be considered. First, it is much more difficult to expose the lumbosacral TB focus in an overweight or obese patient. Second, the sacral screw is difficult to adequately fix to the S1 vertebral body when the S1 is severely damaged. When the S1 is severely destroyed, a simultaneous posterior approach of internal fixation may be needed with anterior debridement. Furthermore, the anterolateral approach is not appropriate for every surgical facility. The surgeons' experience of the anterolateral approach is vital for the success of the surgery. Otherwise, there will have difficulties and risks during surgery if the surgeon is not familiar with the anatomic structure of the lumbosacral segment. Further studies
Conclusions
Lumbosacral TB is not the common form of TB spondylitis. However, it also can cause severe clinical consequences and become a serious social and economic burden; hence, early diagnosis and treatment are vital. Our study showed that surgical treatment of lumbosacral TB using one-stage anterolateral extraperitoneal debridement, bone grafting, and internal fixation achieved satisfactory clinical outcomes and achieved good results in spinal stability reconstruction. On the basis of the reported literature and the positive therapeutic effect in our patient population, we propose that lumbosacral TB can be efficiently treated with one-stage anterolateral extraperitoneal debridement, bone grafting and internal instrument fixation.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.