Introduction
Autologous iliac crest bone grafting, local bone, ceramics, demineralized bone matrix, and bone morphogenetic proteins (BMPs) are all methods used for lumbar fusion [1]. The use of BMPs increased significantly from 2004 to 2009 and 33% of the bone fusions performed in the United States in 2009 involved the use of BMPs [2]. Several authors have reported complications with autologous iliac crest bone grafting, such as donor site pain and fractures. BMPs have also been associated with disadvantages such as ectopic bone formation, vertebral osteolysis, and postoperative radiculitis in the lumbar spine [3].
Parathyroid hormone (PTH) has been recently used to increase vertebral bone mineral density (BMD) in osteoporotic patients [45]. Moreover, the efficacy of PTH for lumbar posterolateral fusion (PLF) has been reported using animal models [678]. Compared with an autograft only group, animal model experiments showed that the bone fusion rate after PTH treatment was significantly higher [678]. The efficacy of recombinant human PTH (1–34) (teriparatide) for fracture healing in the cervical spine was shown in a case report [9]. Further, delayed unions of type III odontoid fractures in three patients showed complete fusion after PTH treatment [9]. We previously reported that for instrumented PLF in the osteoporotic spine, daily subcutaneous injections of teriparatide with local bone grafting were more effective than local bone grafting alone [10]. Furthermore, the incidence of pedicle screw (PS) loosening in the teriparatide group was significantly lower than in the local bone grafting alone group in the osteoporotic spine [11]. In several Asian countries including Japan, BMPs are not approved for clinical use; thus, teriparatide is rapidly becoming the gold-standard treatment for bone fusion in osteoporotic spine surgery.
In a clinical setting, the use of PTH is limited to 2 years, and there is a possibility that the fusion mass will decrease or disappear once teriparatide is discontinued. However, no study has shown that cessation of teriparatide treatment will change the volume of the bone fusion mass after lumbar PLF in women with postmenopausal osteoporosis. Therefore, the purpose of the current study was to determine whether discontinuing teriparatide treatment, and replacing it with bisphosphonate treatment, maintains the bone volume of the fusion mass after PLF in women with postmenopausal osteoporosis.
Materials and Methods
1. Patients
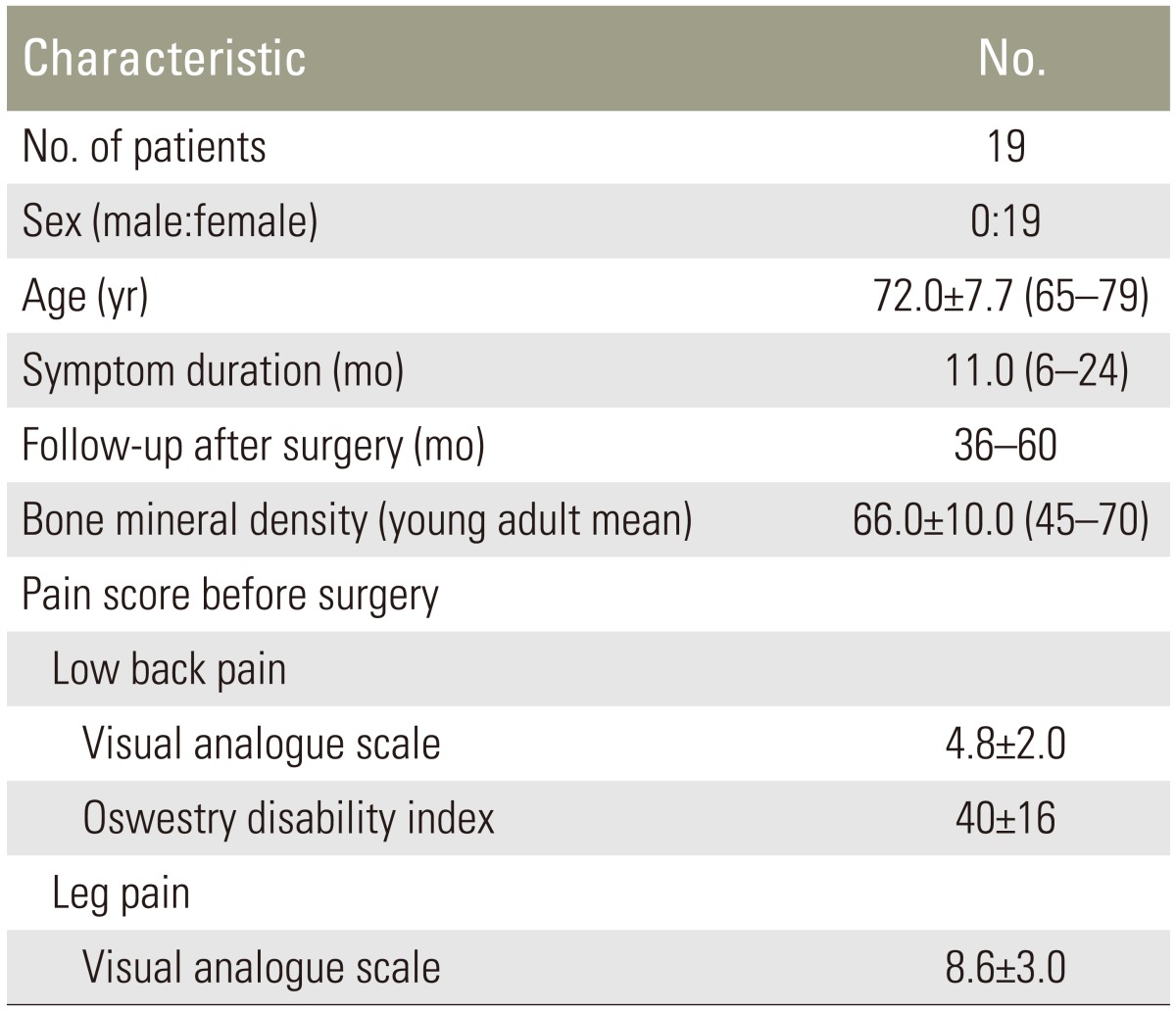
Between January 2010 and January 2016, we retrospectively evaluated 19 patients treated at our university hospital. Patients were 65 to 79 years of age (mean±standard deviation [SD], 72.0±7.7 years). The main complaint was low back and leg pain, or leg pain only. All patients had lumbar degenerative spondylolisthesis (slipping of L3 or L4). Some patients showed intermittent claudication within 50 to 100 m. Patients were diagnosed with one-level L3 or L4 degenerative spondylolisthesis, and spinal stenosis on radiographs, dynamic radiographs, and magnetic resonance imaging. Exclusion criteria were past lumbar surgery, spinal tumors, infections, or acute vertebral fractures of the lumbar spine. Diagnosis of spondylolisthesis and inclusion criteria for fusion surgery were (1) more than 5% slip of the vertebra in a neutral position; or (2) translation greater than 3 mm between flexion and extension positions on radiographic evaluation. Informed consent was obtained from each of the participants. All of them were diagnosed as having osteoporosis based on the Japanese criteria [12]. BMD of the lumbar spine was measured before surgery. We evaluated pain according to the visual analog scale (VAS) score (0, no pain; 10, worst pain) for low back pain and leg pain, and recorded Oswestry disability index for low back pain. Details of the patient background characteristics are shown in Table 1.
All patients underwent decompression and PLF at the level of the spondylolisthesis. One-level PLF was performed using PSs and a local bone graft. Bilateral facet fusion was performed in all patients. The local bone consisted of the lamina from the decompression site and spinous process. We did not use other osteoconductive products for spinal fusion.
2. Administration of teriparatide and risedronate
Patients were administered teriparatide 2 months prior to surgery and more than 8 months after surgery, with average treatment duration of 11.5±2.5 months (teriparatide 20 mg by daily subcutaneous injection, Eli Lilly, Tokyo, Japan). We have previously reported that a longer period of teriparatide treatment (>6 months before and after surgery) for bone union was more effective than a shorter period of treatment [13]. Thus, we used teriparatide 2 months before surgery and more than 8 months after surgery. Twelve patients used bisphosphonate (risedronate) (weekly oral administration of risedronate 17.5 mg, Eisai, Tokyo, Japan) for an average of 6.5±2.7 months (range, 3–12 months) before using teriparatide. Seven patients did not use bisphosphonate before using teriparatide. After treatment with teriparatide, all patients used risedronate during the follow-up period (average, 30.6±15 months; range, 26–40 months).
3. Radiographic evaluation
Radiographs were used to evaluate bone union. Profile views of radiographic images in flexion and extension before and 1, 2, and 3 years after surgery were evaluated. We classified bone union or failure to fuse at the surgical level. We defined bone union as less than 1.5° of instability between the flexion and extension positions, or continuous fusion between transverse processes (Fig. 1). Evaluation of bone union was blinded and performed by three surgeons independently. Fusion was considered to have occurred if at least two of the observers agreed on this assessment. Sites that did not fused in 1 year were excluded from the follow-up examination.
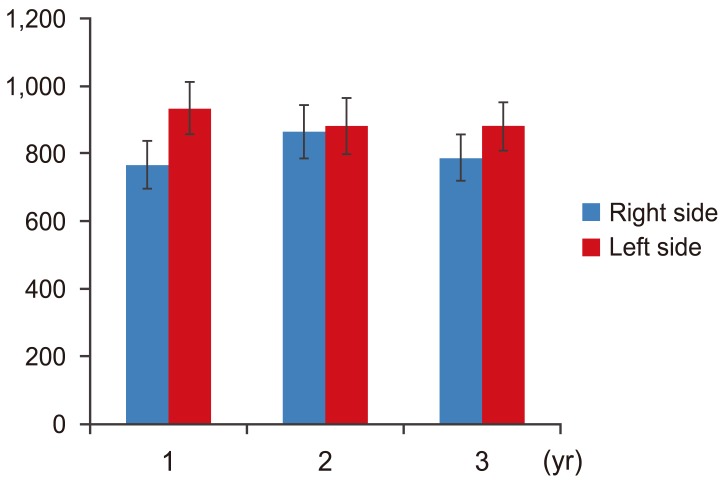
Antero-posterior radiographic views were also evaluated at 1, 2, and 3 years after surgery in all patients. The area of the bone fusion between transverse processes on each side was measured using a computer-linked digitizer. Three observers measured the bone volume, and the data were averaged.
Results
Table 1 shows the demographic characteristics of the patients before surgery. Fusion rates were 84%, 95%, and 95% at 1, 2, and 3 years after surgery (Table 2). One patient showed absence of fusion bilaterally 3 years after surgery. We evaluated the change of bone volume of the fusion mass in 32 segments of 16 patients who had evidence of fusion at 1 year after surgery.
Fig. 2 shows the average area of the bone fusion mass on the right and left sides. There was no significant difference in the average area of the bone fusion mass between sides. The average area of bone fusion was not significantly different after surgery for either side (p>0.05) (right side at 1 year, 765.1±70.8 mm2; 2 years, 865.1±80.4 mm2; and 3 years, 787.2±69.8 mm2; left side at 1 year, 933.2±78.2 mm2; 2 years, 880.6±84.3 mm2; and 3 years: 880.5±72.0 mm2).
Discussion
The current study showed that discontinuing teriparatide treatment did not reduce the volume of the bone fusion mass after PLF in women with postmenopausal osteoporosis within 3 years after surgery when a bisphosphonate was administered following teriparatide discontinuation.
In several Asian countries including Japan, BMPs are not available for spinal fusion. Thus, other agents are needed for spinal fusion in patients with osteoporosis. Bisphosphonates are a potential class of therapeutic agents for osteoporosis. Several animal studies have investigated the effects of bisphosphonates on spinal fusion. Fusion masses in alendronate-treated rats undergoing an intertransverse fusion using an autograft appeared radiographically larger and denser than those in control rats despite lower fusion rates [14]. Conversely, rabbits undergoing an inter-transverse process fusion with zoledronic acid treatment achieved increased fusion mass size and bone mineral content with increased fusion rate [15]. Only one prospective randomized trial has evaluated alendronate for lumbar interbody fusion [16]. Forty patients with osteoporosis, who were candidates for one-level posterior lumbar interbody fusion, were randomly assigned to an alendronate-treated group or a control group. A solid fusion was achieved in 95% of the patients in the alendronate-treated group compared with 65% of those in the control group [16].
Recently, subcutaneous injections of teriparatide (20 µg/day) have been used effectively for a maximum of 24 months to increase BMD in patients with osteoporosis. Compliance data from 1,671 patients showed that 71.9% of patients remained on teriparatide treatment after 12 months [17]. Bone formation biomarkers rapidly increased within 1 month of the initiation of teriparatide treatment, with smaller increases in resorption markers. After 12 months of teriparatide treatment, there was an increase in BMD at the lumbar spine, femoral neck, and total hip, and a decrease in the VAS score for back pain [17].
We previously reported on the efficacy of teriparatide for spinal fusion. Fifty-seven women with osteoporosis diagnosed with degenerative spondylolisthesis were divided into two treatment groups, a teriparatide group (n=29, daily subcutaneous injection of 20 µg of teriparatide) and a bisphosphonate group (n=28, weekly oral administration of 17.5 mg of risedronate) [10]. All patients underwent decompression and PLF with a local bone graft. Daily injection of teriparatide for bone union was more effective than oral administration of bisphosphonate [10]. Furthermore, a longer period of teriparatide treatment for bone union was more effective than a shorter period of treatment [1013].
Teriparatide effectively increases BMD, but its period of use is limited to 2 years. It is difficult to maintain the BMD gains achieved by teriparatide if the patients do not use bisphosphonates after discontinuing teriparatide [1819]. Both hormone replacement therapy and bisphosphonates have been shown to maintain or increase BMD at the lumbar spine and hip after discontinuation of teriparatide treatment [1819]. Muschitz et al. [20] demonstrated that the addition of alendronate 9 months after the initiation of teriparatide treatment resulted in an augmented increase in BMD both in the lumbar spine and hip region. In the alendronate combination group, with the exception of areal BMD and the trabecular component of femoral neck BMD, the increase in BMD was significantly greater compared with the teriparatide monotherapy group [20]. These results indicate that the use of bisphosphonate after discontinuation of teriparatide is necessary to maintain BMD. In the current study, after treatment with teriparatide, all patients used risedronate during the follow-up period, which prevented a reduction in the volume of the bone fusion mass 3 years after PLF in women with postmenopausal osteoporosis.
The current study has some limitations. First, it is a retrospective study based on a small sample. Second, we examined BMD in the lumbar spine before surgery, but we did not examine BMD after surgery. It would have been better to examine BMD after surgery, but were unable to so as we experienced instrumentation problems and could not get accurate BMD data. Third, we did not evaluate serum bone biomarkers. Fourth, we used risedronate after successful spinal fusion in all patents, but did not examine a control group without the use of risedronate. Fifth, we used radiography to evaluate bone union; however, we did not evaluate bone fusion using computed tomography.