Effectiveness and safety of preoperative distraction using modified halo-pelvic Ilizarov distraction assembly in patients with severe kyphoscoliosis
Article information
Abstract
Study Design
A 2-year follow-up study.
Purpose
To evaluate the effectiveness of modified halo-pelvic Ilizarov distraction assembly in the management of patients with severe kyphoscoliosis.
Overview of Literature
Severe and rigid scoliosis curves are always a challenge for operating surgeons. Preoperative correction through halo-pelvic devices successfully minimizes the severity of the curve; however, cumbersome complications are also reported with its use. Modified assembly could be safe for these cases.
Methods
Patients with severe kyphoscoliosis having coronal Cobb angle >90° were applied with modified halo-pelvic Ilizarov distraction assembly preoperatively. The modified assembly consisted of a pelvic component and halo ring, and distraction was given at the rate of 2–3 mm/day for 6–12 weeks. Complete clinical assessments along with pulmonary function tests were performed, and scoliosis series X-ray images were assessed for coronal and sagittal Cobb angle and other spinopelvic parameters before applying the assembly and during 2 years of follow-up.
Results
Thirty-four patients (age, 9–27 years; male/female ratio of 18:16) were included. The coronal and sagittal Cobb angles were 116°±16.2° and 84°±28.3°, respectively. Correction rates obtained through modified halo-pelvic assembly were nearly 52% (p<0.001) in coronal and 40% (p<0.001) in sagittal Cobb angles, with improvement in height (p<0.001). Apical vertebral translation and coronal balance were also improved significantly (p<0.001). Further improvements in all the parameters were obtained after definitive surgery, with improvements in the forced expiratory volume in 1 second (p=0.002) and forced vital capacity (p=0.001).
Conclusions
Our modified halo-pelvic Ilizarov distraction assembly can achieve good correction in severe spinal deformities without significant risk to neurology, has fewer complications, and promotes good patient compliance.
Introduction
Despite the fast development in modern techniques and instrumentation, the management of severe kyphoscoliosis remains challenging. It even becomes more crucial if the curve angle is >100° with significant kyphosis and/or a history of intraspinal pathology is present [1]. Kyphoscoliosis can involve the thoracic region, lumbar region, or both, and it may occur alone or as a manifestation of any neuromuscular disease. Severe and rigid deformities are much more complicated to address even with surgery.
Patients with severe spine deformities typically undergo surgery using anterior, posterior, and combined anterior–posterior approaches. However, complication risks are higher if the deformity becomes rigid and severe. These difficult curves require prolonged surgeries with complex osteotomies and are usually accompanied by tissue releases that may cause several problems. Literature indicates that complication rates range from 18% to 74% in spinal deformity surgeries, particularly when the preoperative curve angle is >60°. Pulmonary complications are most common, followed by implant-related issues, infections, neurological complications, and pseudoarthrosis [2–5]. These patients require extensive medical care and prolonged hospital stays [6]. Given the potentially life-threatening nature of complications, interventions before corrective surgeries are essential to minimize risks.
Methods such as preoperative halo-femoral, halo-tibial, and halo-gravity traction offer significant corrective forces; however, hitches such as extended periods of bed rest and hospital stay, difficulty in performing daily living activities, and discomfort have been reported. Literature suggests that improving and modifying the traction devices, particularly halo-pelvic devices, can effectively manage kyphoscoliotic deformities before corrective surgery. Accordingly, our team developed a modified halo-pelvic distraction device using a standard Ilizarov ring fixator set. This innovation has shown promising results in reducing perioperative and postoperative complications. Unlike traditional and other versions of halo-pelvic devices, patients responded well to our modified version [7]. Thus, this study aimed to analyze comprehensively the outcome of 34 patients with severe kyphoscoliotic deformity managed using our modified halo-pelvic Ilizarov distraction device.
Materials and Methods
Patients with kyphoscoliosis who presented with a coronal Cobb angle of >90° and had no radiological evidence of osseous fusion along ≥3 vertebrae between January 2021 and September 2021 were recruited after obtaining ethical approval and informed consent. Patients with a history of blood dyscrasias, any psychiatric illness, or cerebral palsy were not included. The project was approved by the Ethical Review Committee of Ghurki Trust Teaching Hospital Lahore Pakistan (IRB approval no., 2020/11/R-20).
The complete demographic and clinical profiles were obtained along with standing radiographs. Patients were evaluated for upper and lower limb neurology, cranial nerves, bladder and bowel reflexes, and pulmonary function tests including forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1). Anteroposterior and lateral standing radiographs of the whole spine were obtained to assess the magnitude of the coronal and sagittal deformities by measuring the coronal and sagittal Cobb angles, apical vertebral translation (AVT), and coronal and sagittal balance. In addition, right and left bending and traction views were taken to assess curve flexibility.
Whole spine computed tomography and magnetic resonance were also obtained to rule out any vertebral column and spinal cord anomaly, respectively. The patients were evaluated using the Scoliosis Research Society-30 Questionnaire (SRS-30) before the application of the assembly and 3 months after surgery [8].
Description of the modified halo-pelvic Ilizarov distraction assembly and its application
A modified halo-pelvic Ilizarov distraction assembly was constructed using several modifications described in our earlier report [7]. Briefly, two lateral Ilizarov femoral arches were used instead of a pelvic ring that allowed the patient to lie supine on the bed. To give a strong and stable pelvic construct, two Ilizarov half-pins were inserted in the supracetabular area of the pelvis and two in the ileum. Two anterolateral and two posterolateral threaded rods were used to provide the distraction force (refer to Supplement 1).
Pelvic component
The pelvic component consisted of two standard femoral arches from a standard Ilizarov fixator instrument set. Each femoral arch was connected to the hemi-pelvis by two Ilizarov tapered half-pins. Moreover, 6- and 5-mm half-pins were used in adults and children, respectively. One half-pin was inserted in the anteromedial direction in the supra-acetabular area just below the anterior inferior iliac spine (Fig. 1). The entry was made by a sharp-tipped bone awl, a track was then made using a blunt bone awl, and a threaded channel was created by bone tap. A half-pin was inserted manually with the help of a T-handle. The second half-pin was passed anterior in the iliac crest perpendicular to the axis between the two tables 10–12 cm posterior to the anterior superior iliac spine, and a half-pin was inserted in a similar manner as described above. Half-pins were connected to the femoral arch using Wrencho cubes and male posts. Both femoral arches were connected anteriorly using a telescopic threaded rod. The “pelvic construct” should be in line with the position of the pelvis.
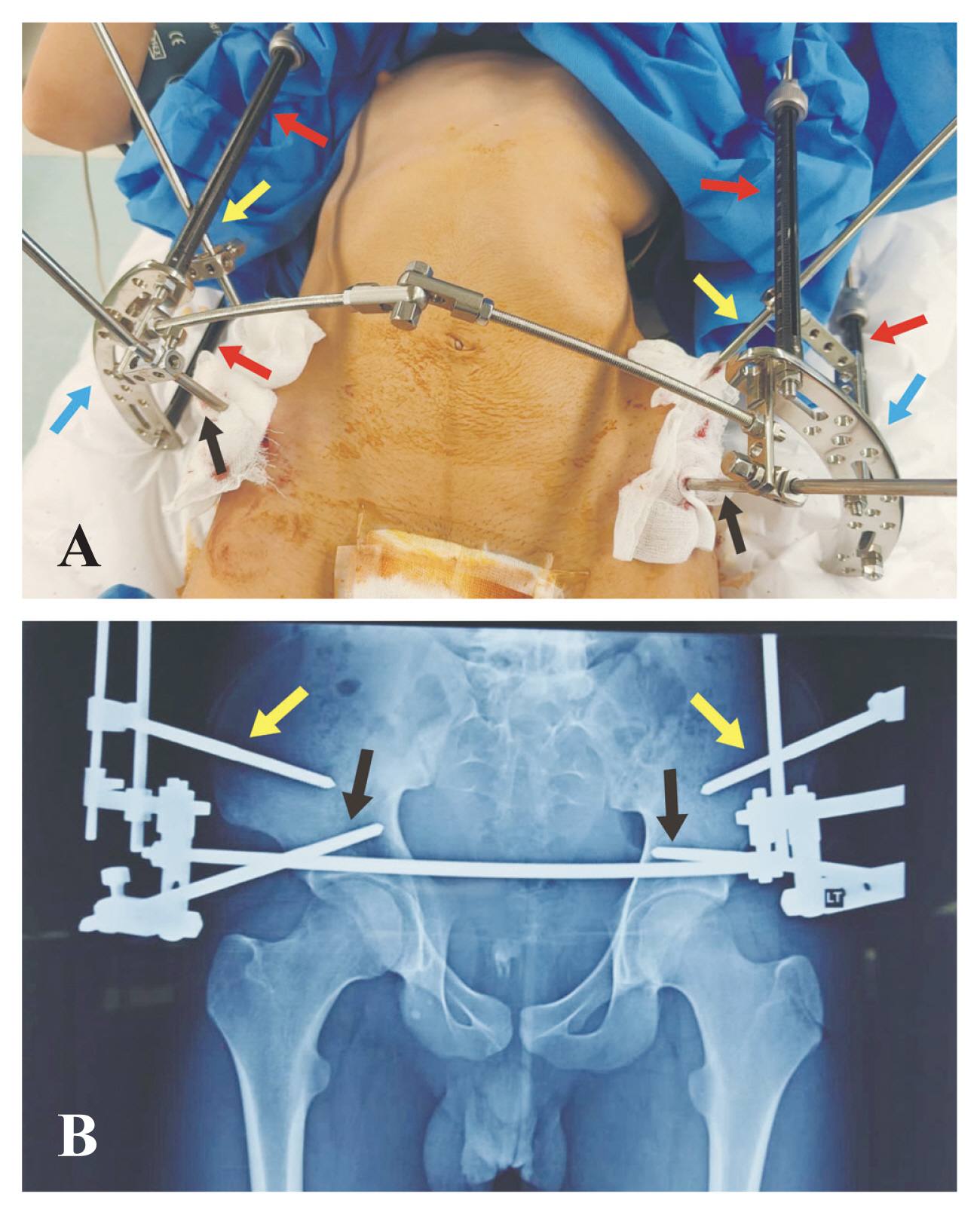
(A, B) Pelvic component of modified halo-pelvic Ilizarov distraction assembly applied on a 14-year-old male along with an anteroposterior radiograph of his pelvis. Blue arrows indicate femoral Ilizarov arches, yellow arrows showing half pins in ilium while black arrows demonstrate half pins in the supracetabular area, telescopic threaded rods are shown by red arrows. Written informed consent for the publication of this image was obtained from the patient.
Halo component
The halo component consisted of a standard halo ring made of aluminum. An appropriately sized halo ring was anchored to the skull using six sharp-tipped pins just abutting the outer table of the skull in the safe zones.
Formation of assembly
The halo- and pelvic components were connected using four threaded rods. Two were anterolaterally placed, whereas the other two were placed posterolaterally. These rods were positioned in such a way that the patient could easily lie supine on the bed. Distraction was given using these connecting rods.
Protocols during the distraction phase
During the distraction phase, patients remained hospitalized to monitor the distraction rate and associated complications. The distraction was started at 2 mm/day (1 mm twice a day) while closely monitoring for any neurological deterioration. If this rate was tolerated well by the patient, it was increased to 3 mm/day (1 mm 3 times a day). If neurological symptoms are present, the distraction was reversed by 10 mm acutely to relax the spinal cord. After symptom resolution, which usually took 3–7 days, distraction was started again at 1/2 mm bid. The distraction period varied from 6 to 12 weeks until the desired correction was achieved. During the distraction period, patients were closely monitored for pin tract infection, and anteroposterior and lateral radiographs of the whole spine were obtained weekly to evaluate the degree of correction and any sign of pin tract loosening.
Removal of the halo-pelvic Ilizarov distraction assembly and corrective surgery
Once the desired correction was achieved using the halo-pelvic Ilizarov distraction assembly, segmental spinal instrumentation was performed by a consultant spine surgeon (second author) through a posterior midline approach. After the surgery, the assembly was removed before the patient was extubated.
Follow-up after corrective surgery
After spinal fusion surgery, patients were asked to come back for the first follow-up after 2 weeks for the removal of stitches. Thereafter, patients were asked to come for follow-up after 4 weeks for 3 months, after 3 months for 1 year, and every 6 months in the second year.
On all follow-ups, orthogonal X-ray images of the whole spine were taken to assess union and any signs of implant loosening or reduction loss. Pulmonary function tests (FVC and FEV1) were assessed again after 3 months of surgery.
Statistical analysis
Data were analyzed using IBM SPSS Statistics ver. 25.0 (IBM Corp., Armonk, NY, USA). All quantitative data are presented as the mean±standard deviation (SD). Statistical comparisons of the radiographic measurements and pulmonary function test results were performed using a parametric paired sample t-test and repeated measure analysis of variance, and p<0.05 was considered statistically significant.
Results
Demographic and clinical profile
Thirty-four patients with kyphoscoliosis (male, 18; female, 16) were included in the study. Their age ranged from 9 to 27 years (mean±SD, 15.4±4.3 years). Nearly 19 (56%) presented with congenital scoliosis, 8 (23.5%) had idiopathic scoliosis, and the remaining patients had neuromuscular conditions, except for cerebral palsy. All but two patients had intact neurology. One of them presented with disturbed lower limb neurology (decreased sensation over the L2–L4 dermatome), and the other had 4/5 power in the left lower limb.
Radiological parameters and traction data
The coronal Cobb angle (scoliosis) ranged from 92° to 155° (mean±SD, 116°±16.2°), and in the traction view radiograph, it ranged from 70° to 125° (mean±SD, 93.5°±13.3°) (Table 1). The sagittal Cobb angle ranged from 16° to 135° (mean±SD, 84°±28.3°). Nearly 26 patients (76.5%) had a thoracic curve, 5 (14.7%) had a thoracolumbar curve, and 3 (8.8%) had a lumbar curve. The Risser grades were between 0 and 5 (3.9±1.6), and nearly 5 (14.7%) had open tri-radiate cartilage.
Follow-up during and after the distraction period
General behavior and satisfaction rate of the patients
The duration of distraction ranged from 30 to 85 days. If neurological symptoms occurred, the distraction was reversed to approximately 10 mm and stopped until symptom resolution, which took 7–15 days. The distraction was again started at a slower pace of 0.5 mm twice a day. In general, the halo-pelvic device was very well tolerated by all 34 patients (refer to Supplement 2) (Table 2).
Post-distraction corrections and improvements
After the distraction period, the height and weight of the patients improved, which was highly significant (p<0.001) for height, whereas no significant difference was seen for weight. The coronal Cobb angle improved by 52%, which was highly significant (p<0.001), whereas the sagittal Cobb angle improved significantly by 40% (p<0.001). AVT and coronal balance also improved significantly (p<0.001) (Table 1, Fig. 2). The sagittal balance improved; however, no significant difference was seen. Age and sex did not have any significant effect on the improvement of any parameter.
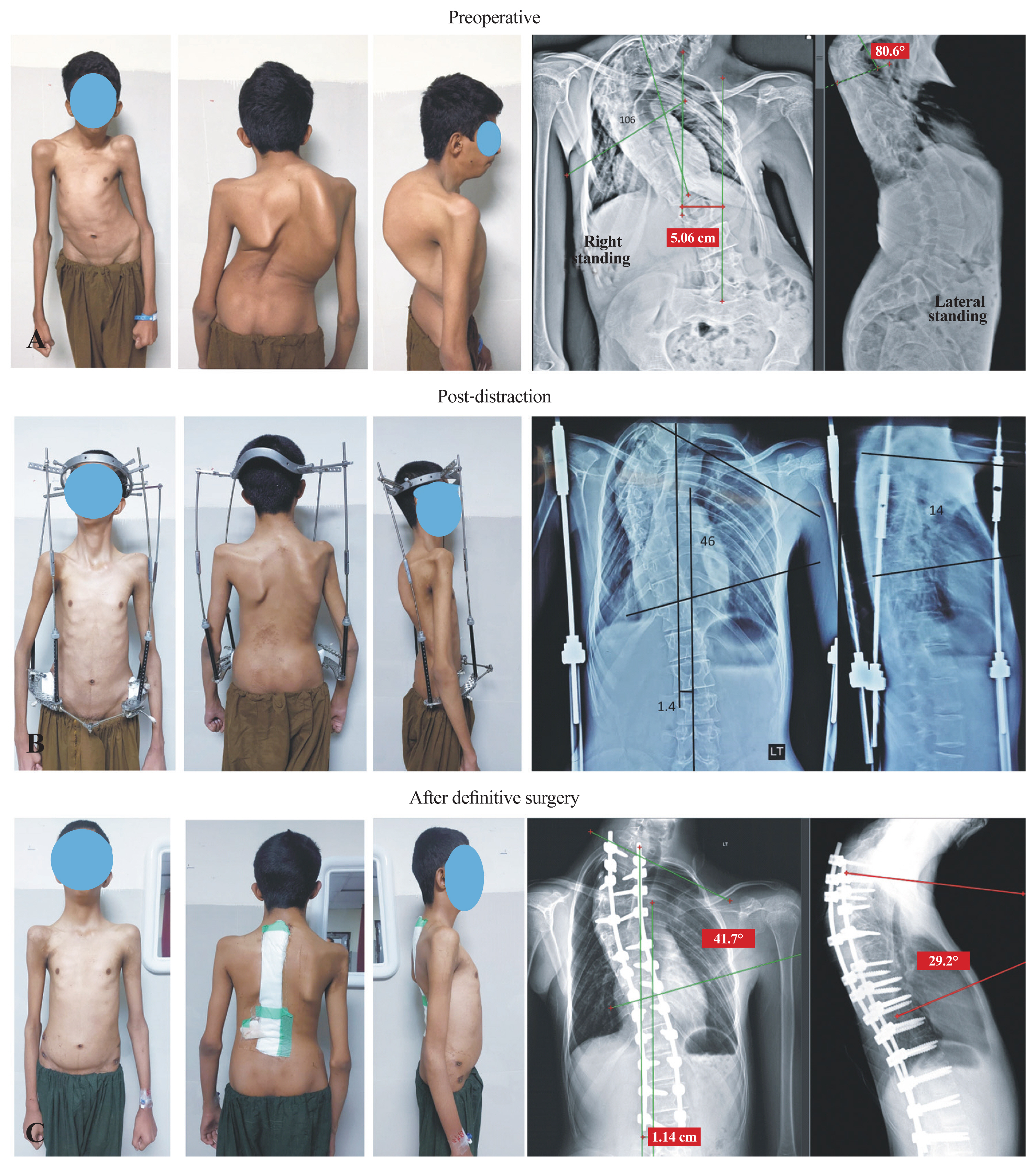
(A–C) A 15-year-old male, 106° coronal Cobb angle showed improvement to 46° after distraction and 41° after definitive surgery. Sagittal Cobb from 81° to 14° after distraction and then 29° after definitive surgery. Marked improvement in coronal balance was seen that was from 5 to 1.4 cm after distraction and further improved to 1.1 cm after definitive surgery. Written informed consent for the publication of this image was obtained from the patient.
Definitive surgery and follow-up after surgical correction
Definitive surgery was performed without Ponte osteotomy and vertebral column resection. The procedure was completed smoothly on all patients without any complications. After the final corrective surgery, the weight and height of the patients remained unchanged (Table 1).
Post-surgical corrections and improvements
The coronal and sagittal Cobb angles were further significantly reduced by 29% (p<0.001) and 27% (p<0.001), respectively. The AVT and coronal balance also improved significantly (p=0.001, p<0.001) (Fig. 3).
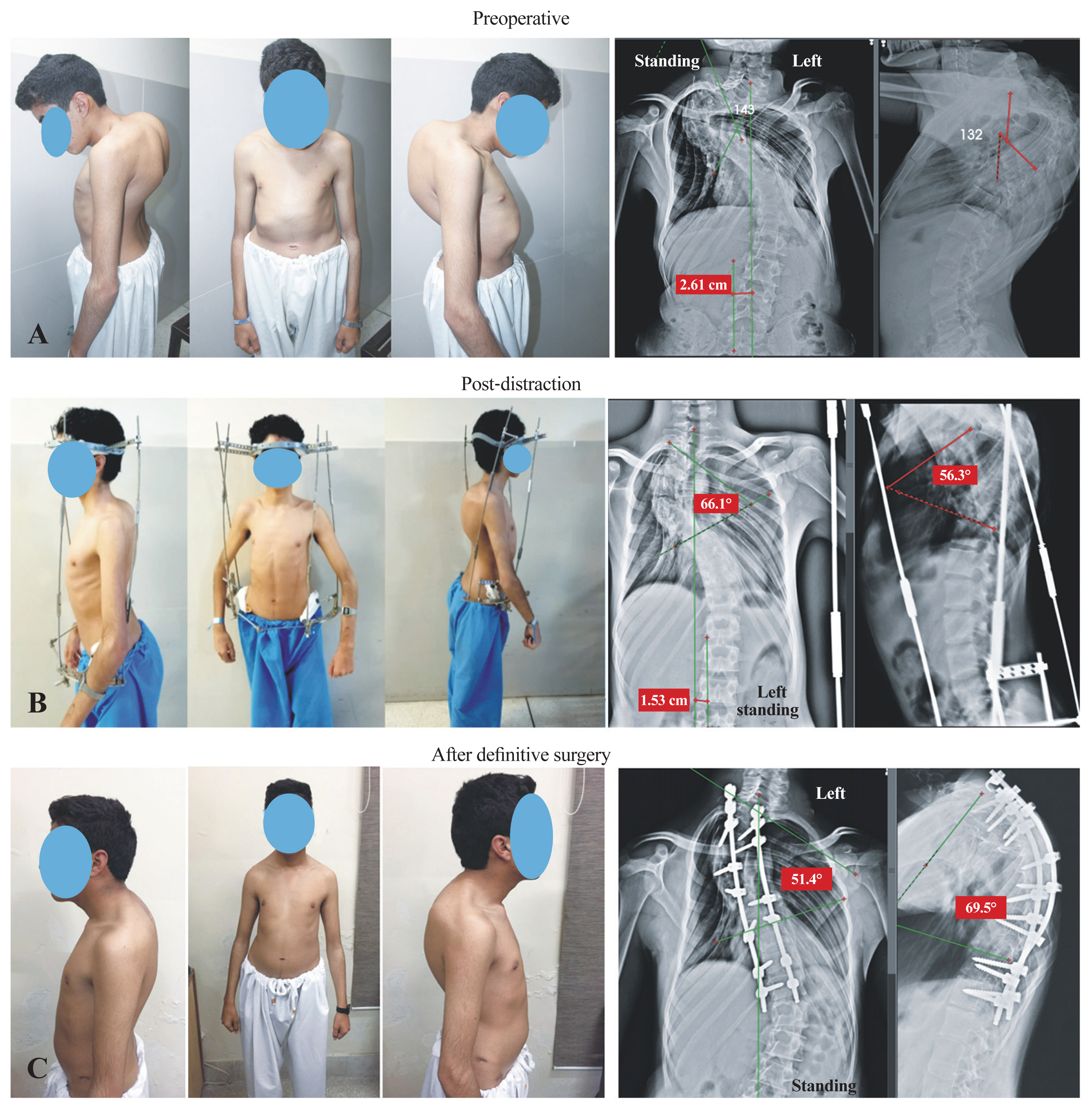
(A–C) A 16-year-old male with severe kyphoscoliosis showing improvement in coronal Cobb angle of 143° to 66° after distraction and 51° after definitive surgery. The sagittal Cobb angle corrected from 132° to 56° after distraction to 69° after definitive surgery. Coronal balance showed improvement from 2.6 to 1.5 cm which became neutral after surgery. Written informed consent for the publication of this image was obtained from the patient.
In the repeated measure ANOVA with Greenhouse–Geisser correction, the mean height, coronal and sagittal Cobb angles, AVT, and coronal balance differed significantly between time points (F [1.15, 35.72]=54.4, p<0.001; F [1.5, 51.31]=426.9, p<0.001; F [1.4, 37.4]=66.2, p<0.001; F [1.6, 54.05]=35.85, p<0.001; and F [1.8, 50.7)]=21.1, p<0.001, respectively) (Table 3).
Pulmonary function tests
Significant improvements in FEV1 and FVC were seen in patients after surgical correction. FEV1 increased from a mean of 0.88 to 1.6 L (p=0.002). Similarly, the FVC improved from a mean of 1.05 to 1.71 L (p=0.001) (Table 1).
Complications
After the application of the assembly, pin tract infections developed in 20 patients, which were treated successfully with oral antibiotic therapy. Half-pin (in one patient, supra-acetabular; and in two, iliac) loosening was reported in three patients after 3 weeks; thus, the half-pins were removed, and distraction was continued with the remaining half-pins. Two patients experienced decreased lower limb muscle strength after 2–3 weeks of distraction. The traction was stopped, and patients were allowed to recover. Another patient was observed to have decreased sensation over the T11–T12 dermatome, which was also managed in the same way. Those two patients who presented with impaired lower limb neurology remained as such.
Discussion
In this study, our modified halo-pelvic Ilizarov distraction assembly achieved significant curve reduction before the definitive correction surgery (Fig. 4). The results showed average correction of the coronal and sagittal Cobb angles of >50% and 40%, respectively, which were quite considerable in magnitude when compared with the average Cobb angle in the traction X-ray images that signify the excellent efficacy of the device. In addition, a significant increase in the average height of nearly 8 cm was noted. Spinal curve reduction significantly increased the amount of space in the chest, which effectively improved pulmonary functions and provided better tolerance and prognosis for aggressive surgery.
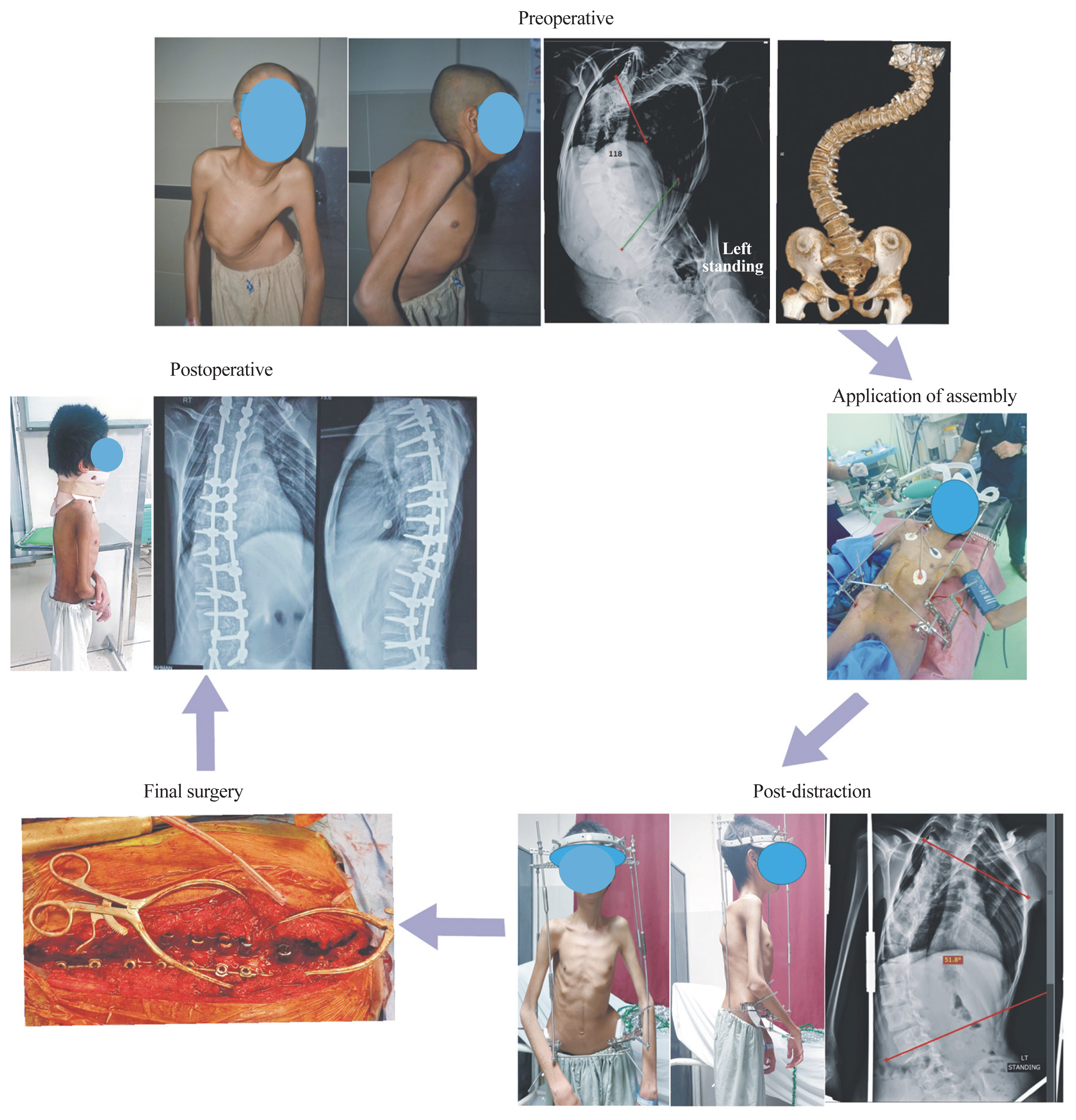
The figure showcasing the progression from preoperative severe spinal curves to significant reduction after halopelvic assembly. The upper panel depicts a spine with severe kyphoscoliosis, the right panel highlights the application of assembly and post-distraction correction. Finally, the left panel demonstrates the surgical intervention and postoperative outcome, displaying the substantial reduction in spinal curvature.
The concept of halo-pelvic assembly dates back to 1959 when it was initially applied to immobilize unstable cervical segments and later in the 1970s for spinal deformities [9]. The gradual traction force exerted through the halo-pelvic device creates continual fatigue of the paraspinal muscles while displacing the adjacent soft tissues such as tendons and ligaments. Tissue cells adapt to this new structural state, which facilitates correction [10]. This traction mechanism is preferred over halo-femoral and halo-gravity tractions, particularly in severe and rigid curves where a slightly longer traction period is required. Halo-femoral traction requires an extended period of bed rest, and patients have increasing risks of pressure sores, chest infections, and deep venous thrombosis [11], whereas halo-gravity traction provides limited traction [12]. Nonetheless, the traditional halo-pelvic traction device led to major complications, such as paraplegia, cranial nerve palsies, pain, radiological degenerative changes, avascular necrosis of dens, and various others, contributing to its gradual decline in use. The circular pelvic ring in the traditional device caused discomfort for patients when lying on their backs; furthermore, the anchoring pins passing through the pelvis were associated with a higher incidence of infections [13,14].
Recently, clinical studies have reported reasonable results with fewer complications using their modified assemblies; however, limitations persist, including patients’ distress and negative sagittal balance [9,15,16]. Our tailored assembly addressed all those concerns and yielded satisfactory results. A slow and continuous distraction was infused with the components of the Ilizarov distraction assembly, and severe and rigid deformities were effectively corrected, surpassing the outcomes of halo-gravity traction [17]. The versatility of the Ilizarov apparatus allowed us to customize the assembly for the needs of each patient. Linear distraction and angular correction were comfortably adjusted based on individual’s requirement, achieving stable fixation while minimizing neurological complications. Surgical correction did not require extensive soft tissue releases or osteotomies, such as Ponte osteotomy or vertebral procedures, which are significantly associated with morbidity, increased operative time, and blood loss [18,19].
The lateral arches in our assembly enhanced the comfort level of the patients and allowed them to perform routine tasks easily and sleep in the supine position. The selection of the supracetabular area for half-pin insertion proved to be a strong anchorage point and provided sturdy support unlike previous assembly in which pins are inserted between the inner and outer tables of the ileum [15]. Because patients with scoliosis are frequently osteoporotic with weak bones, using only the ilium in these cases may be a poor anchorage point for screws.
In our technique, we used four rods, two anterolateral and two posterolateral, instead of just anterolateral rods used in the previously reported halo-pelvic assembly [15], which provided balanced distraction force. The distraction duration depended on the severity of the curve and response of the patient. In most patients, the desired correction was achieved in 3–4 weeks. However, in some patients with compromised neurology, the distraction rate was adjusted and reverted a few millimeters to reverse the neurology. No complications related to cranial nerves, brachial plexus, broken pins, subluxation of atlantoaxial joint, and so forth were reported as with previous modified assemblies [9,15,20]. The most frequent complication was mild pin tract infection, which was handled effectively with antibiotics, compared with previously reported severe infections [21]. Close monitoring of the patients during the distraction period helped us identify and handle the complications immediately.
In developing countries where patients with scoliosis usually present with severe and rigid curves along with cardiorespiratory complications, surgical correction is a major challenge [22]; thus, appropriate and well-managed halo-pelvic traction combined with correction surgery is highly efficacious in these cases, as in our modified halo-pelvic Ilizarov traction, which is reliable and has relatively minor complications. Compared with previously documented halo-pelvic assemblies and alternative techniques, patient mobility remained uncompromised, and notable enhancements in curvature severity were observed, avoiding the need for complex osteotomies during corrective surgery. However, the study’s strength could have been further enhanced with comprehensive data comparing different traction methods specifically from our institution.
Conclusions
Our modified halo-pelvic Ilizarov distraction assembly is a potent, effective, and safe tool for the preoperative correction of rigid and severe kyphoscoliosis before definitive surgery. It reduces the rigidity and severity of the curve to an extent that surgical procedure becomes convenient and conducive with minimal risks of complications.
Key Points
The study evaluates the effectiveness of a modified halo-pelvic Ilizarov distraction assembly in managing severe kyphoscoliosis over a 2-year follow-up period.
The assembly comprised of a pelvic component and halo ring was applied with distraction rate of 2–3 mm/day for 6–12 weeks.
Significant improvements were observed in both coronal and sagittal Cobb angles following treatment along with other spinopelvic parameters and pulmonary functions.
The modified halo-pelvic Ilizarov distraction assembly appears to be effective in correcting severe spinal deformities with minimal neurological risks and complications.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
MSI designed and applied the assembly and acquired the complete data. AS performed the final fusion surgeries and helped in acquiring the data. UZ analyzed and interpreted the data, wrote the initial draft, and finalized the manuscript. MI and HE helped in the acquisition of data, assisted the surgeons during the surgery, and in postoperative care. AA supervised and helped in designing the project, facilitated the whole process, and data collection. All the authors have read and approved the final submitted manuscript.
Supplementary Materials
Supplementary materials can be available from https://doi.org/10.31616/asj.2024.0104.
Supplement 1. Application of assembly.
asj-2024-0104-Supplementary-Video-1.mp4Supplement 2. Patient compliance video.
asj-2024-0104-Supplementary-Video-2.mp4


