 |
 |
- Search
| Asian Spine J > Volume 18(3); 2024 > Article |
|
Abstract
Purpose
Overview of Literature
Methods
Results
Conclusions
Notes
Funding
This study was supported by Project of National Clinical Research Base of Traditional Chinese Medicine in Jiangsu Province, China (JD2022SZXMS07), Scientific Research Project of Jiangsu Provincial Health Commission (M2022095), and the Seventh Batch of National Chinese Medicine Experts’ Academic Experience Inheritance Work Project (22QGSC6).
Fig. 1
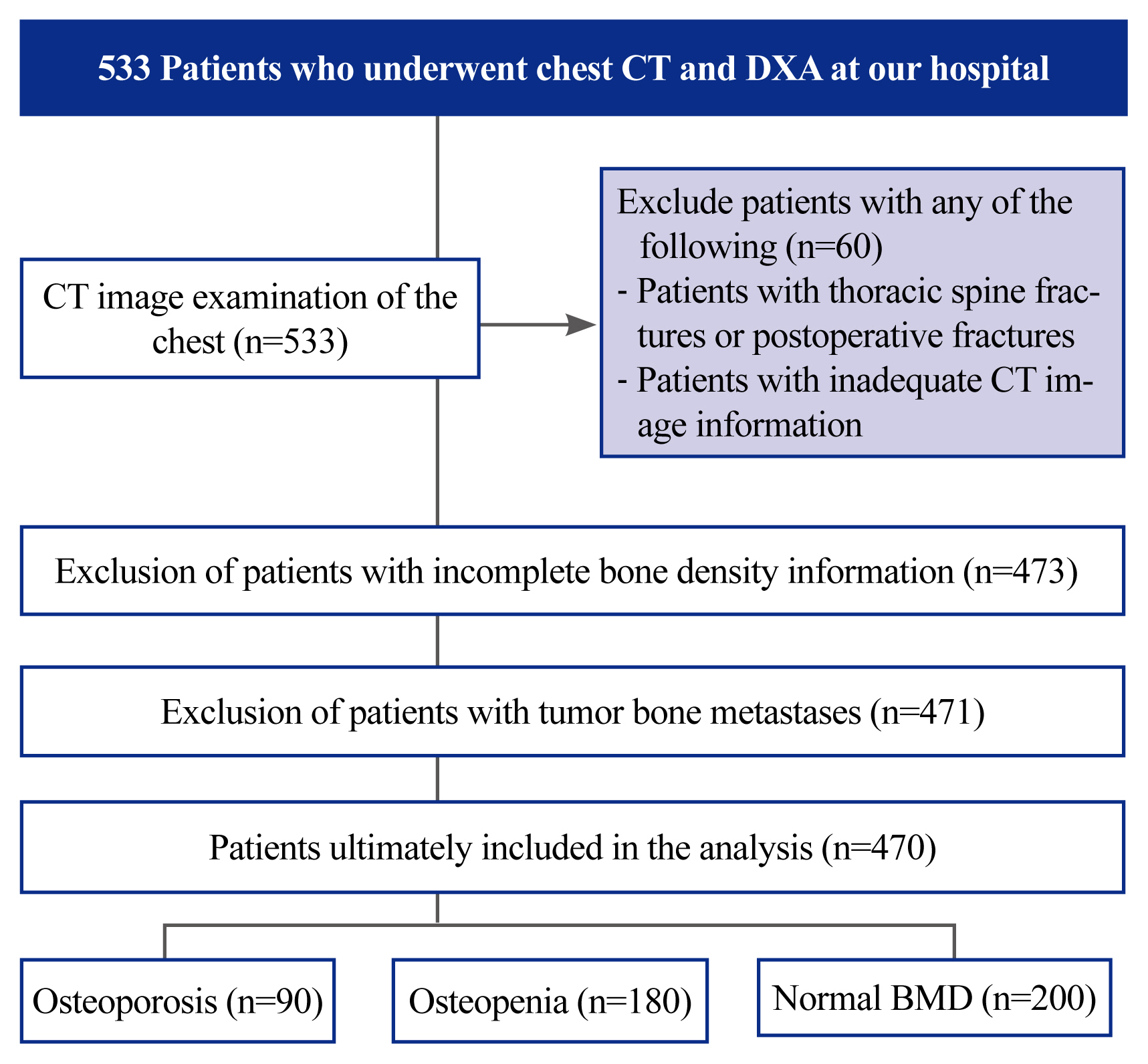
Fig. 2
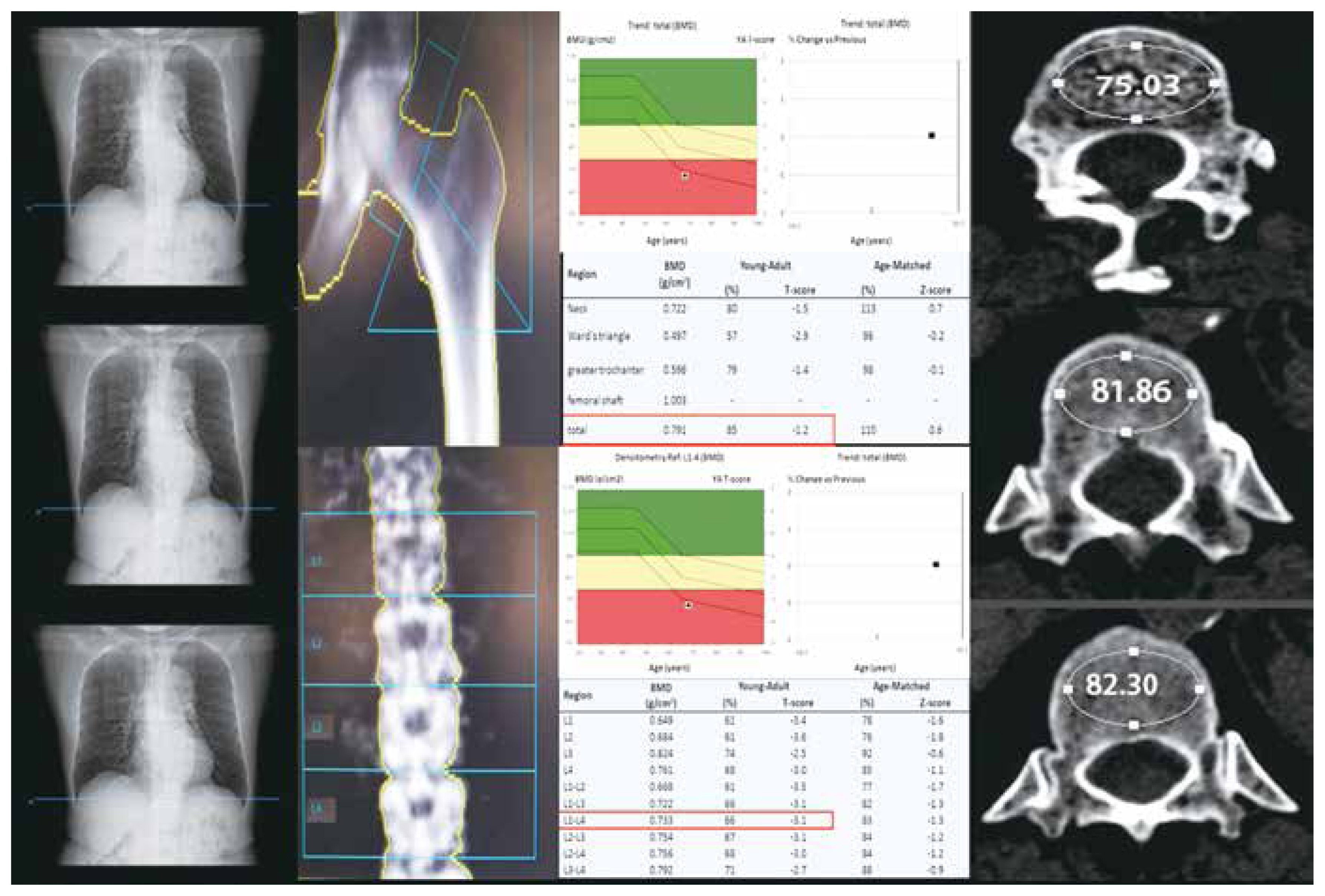
Fig. 3
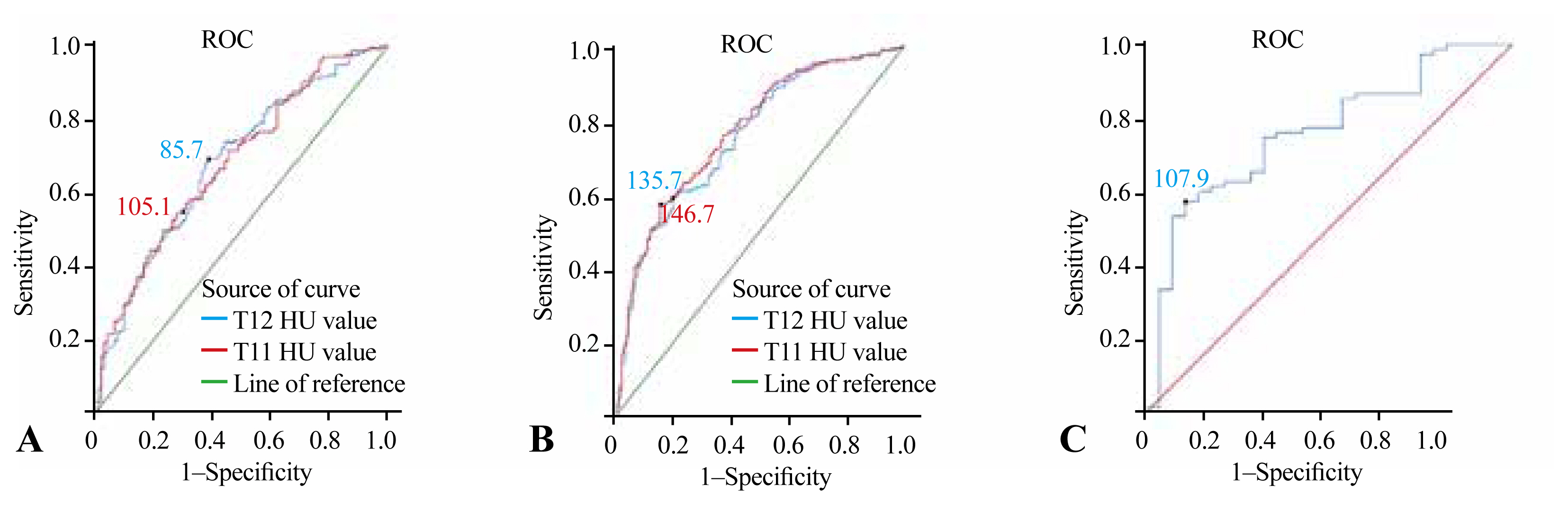
Table 1
Values are presented as mean±standard deviation. The basic information such as height, weight, age, gender, BMI, as well as the interval between CT and DXA examinations, lumbar spine and hip T-score and bone mineral density values, and thoracic spine thoracolumbar segment HU values of the included patients were recorded. The IBM SPSS ver. 25.0 software was used to calculate the mean values of all patients’ recorded information and the mean values of different genders.
Table 2
| Hip-BMD (g/cm2) | L-BMD (g/cm2) | Mean T-score from L1–L4 | Hip T-score | |
|---|---|---|---|---|
| T12 HU value | 0.572** | 0.497** | 0.503** | 0.576** |
| T11 HU value | 0.564** | 0.493** | 0.496** | 0.568** |
The correlation between the mean lumbar and hip BMD and T values and the mean thoracic thoracolumbar segment HU values were calculated in 470 patients by using Spearman’s correlation coefficient with IBM SSPS ver. 25.0 software. The results showed statistically significant differences between the BMD and T-score of the lumbar spine and hip and the HU values of the thoracic spine and thoracolumbar segment. All r-values were positive, suggesting a positive correlation between BMD and T values and HU values. Among them, a significant positive correlation was shown between HU values and T values in the thoracic spine (r=0.576, p<0.01), and the correlation between HU and total hip was significantly stronger than that in the lumbar spine for both T-score and BMD.
Table 3
The thresholds for differentiating osteoporosis, osteopenia, and normal BMD in the thoracic lumbar segment of the thoracic spine were calculated based on the receiver operating characteristic curve. Using an Microsoft Excel spreadsheet (Microsoft Corp., Redmond, WA, USA), all patients were ranked from lowest to highest HU value size, and the number of each group classified by the optimal HU threshold was counted. When the T11 HU value was ≤105.1, 65 of 169 patients were found to have osteoporosis. When the T12 HU value was ≤85.7, osteoporosis was found in 55 out of 120 patients. When the T11 HU value was ≥146.7, 115 of 146 patients had normal BMD. when the T12 HU value was ≥135.7, 119 of 162 patients had normal BMD.
Table 4
The thresholds for differentiating osteoporosis, osteopenia, and normal BMD in the thoracolumbar segment of the thoracic spine were calculated according to the ROC curve, and the sensitivity and specificity of the thresholds were recorded. Positive and negative predictive values were calculated by counting the number of each group according to the calculation formula combined with Table 4. Positive predictive value=number of true positive cases/(number of true positive cases+number of false positive cases); negative predictive value; negative predictive value=number of true negative cases/(number of true negative cases+number of false negative cases). T11 HU values had the highest specificity and negative predictive value for predicting normal BMD. Optimal thresholds were used to detect osteoporosis and normal BMD.
Table 5
| Study time | Study population | No. of included patients | Prevalence of osteoporosis (%) | Vertebrae | The best HU threshold for distinguishing osteoporosis | AUC | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Buckens et al. [19] (2015) | Netherlands | 302 | 27.0 | T12 | 104 | 0.74 | 62.0 | 79.0 | - | - |
| Netherlands | 302 | 27.0 | L1 | 99 | 0.74 | 62.0 | 79.0 | - | - | |
| Kim et al. [20] (2016) | Korea | 232 | 25.6 | T4, T7, T10, L1 (T12) | 136.2 (male) | 0.886 | 95.0 | 77.6 | 59.4 | 97.8 |
| Korea | 232 | 32.5 | T4, T7, T10, L1 (T12) | 137.9 (female) | 0.867 | 96.0 | 64.4 | 56.5 | 97.1 | |
| Cohen et al. [21] (2021) | Israel | 246 | 27.0 | L1–L4 | 121 | 0.764 | 74.0 | 61.0 | 41.0 | 87.0 |
| Zou et al. [22] (2018) | China | 334 | 61.4 | L1 | 110 | 0.86 | 60.8 | 88.5 | - | - |
| Jain et al. [23] (2020) | USA | 313 | 10.9 | L1 | 135 | - | 71.0 | 60.0 | - | - |
| Kim et al. [24] (2019) | Korea | 180 | - | L1–L3 | 146 | 0.96 | 94.3 | 87.5 | 97.6 | 74.5 |
| Li et al. [25] (2018) | China | 109 | 56.9 | L1–L5 | 136 | 0.86 | 90.3 | 72.3 | 81.2 | 85.0 |
Seven published studies reporting HU thresholds for osteoporosis testing such as T12 or L1 from different ethnic and geographic populations were summarized. Sensitivity and specificity of study populations and current use of HU thresholds were counted in an Microsoft Excel spreadsheet (Microsoft Corp., Redmond, WA, USA) and compared across all studies in terms of population, number of patients, vertebral HU values, sensitivity, and characteristics. If the thresholds determined to distinguish osteoporosis from osteopenia were lower than in other regions. The thoracolumbar HU values in other regions ranged from 99 to 146. If the thresholds determined by differentiating between osteopenia and normal BMD were compared with other researchers, it was found that the thresholds obtained in the Chinese, Korean, and American studies were similar and higher than those in the Israeli and Dutch studies. It can be seen that the threshold values obtained in this study are consistent with Asian populations.







