 |
 |
- Search
| Asian Spine J > Volume 18(3); 2024 > Article |
|
Abstract
Study Design
This was a retrospective case-control study using 8 years of data from a nationwide database of surgical outcomes in the United States.
Purpose
This study aimed to improve our understanding of the risk factors associated with a length of stay (LOS) >1 day and aid in reducing postoperative hospitalization and complications.
Overview of Literature
Despite the proven safety of transforaminal lumbar interbody fusion (TLIF), some patients face prolonged postoperative hospitalization.
Methods
Data were collected from the American College of Surgeons National Surgical Quality Improvement Program dataset from 2011 to 2018. The cohort was divided into patients with LOS up to 1 day (LOS ≤1 day), defined as same day or next-morning discharge, and patients with LOS >1 day (LOS >1 day). Univariable and multivariable regression analyses were performed to evaluate predictors of LOS >1 day. Propensity-score matching was performed to compare pre- and postdischarge complication rates.
Results
A total of 12,664 eligible patients with TLIF were identified, of which 14.8% had LOS ≤1 day and 85.2% had LOS >1 day. LOS >1 day was positively associated with female sex, Hispanic ethnicity, diagnosis of spondylolisthesis, American Society of Anesthesiologists classification 3, and operation length of >150 minutes. Patients with LOS >1 day were more likely to undergo intraoperative/postoperative blood transfusion (0.3% vs. 4.5%, p<0.001) and reoperation (0.1% vs. 0.6%, p=0.004). No significant differences in the rates of postdischarge complications were found between the matched groups.
Conclusions
Patients with worsened preoperative status, preoperative diagnosis of spondylolisthesis, and prolonged operative time are more likely to require prolonged hospitalization and blood transfusions and undergo unplanned reoperation. To reduce the risk of prolonged hospitalization and associated complications, patients indicated for TLIF should be carefully selected.
Transforaminal lumbar interbody fusion (TLIF) is one of the most common procedures for treating lumbar spinal pathologies such as spondylolisthesis and spondylolysis. Between 2001 and 2010, TLIF and posterior lumbar interbody fusion (PLIF) accounted for 79%–86% of all lumbar interbody fusions, and TLIF and PLIF are increasingly performed annually [1-4]. Although these procedures are generally well tolerated, the hospital cost per procedure has steadily increased, averaging more than US $50,000 per admission in 2015 [1,3].
The postoperative length of stay (LOS) is an indicator of patient comorbidities, case complexity, and perioperative complications [5-7]. Extended LOS increases costs for both patients and hospital systems [5]. Previous studies have shown increased LOS in cases associated with morbid obesity, advanced age, higher American Society of Anesthesiologists (ASA) classification, longer operative times, and perioperative blood transfusions [6-9]. However, these studies have focused on different procedures or include only specific approaches [5,8].
Although single-level TLIF may be appropriate for the outpatient setting, few studies have examined factors that prevent patients from leaving on the day of or after surgery. Analysis of these factors may aid in selecting patients who are suitable candidates for the outpatient setting, thereby reducing costs and decreasing potential complications. In this study, the national multicenter American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database was used to examine the perioperative factors, complications, and readmissions associated with LOS ≤1 day in patients undergoing single-level TLIF.
Data were collected from the ACS-NSQIP dataset from 2011 to 2018. The ACS-NSQIP database is a random sample of surgical patient demographic information, perioperative parameters, and adverse events data from over 700 hospitals worldwide. The ACS-NSQIP dataset contains prospectively collected data that are audited for interobserver agreeability, as opposed to several administrative databases commonly used for neurosurgical research [10]. Because the data are de-identified and publicly available, this study is not considered a human subject research by the institutional review board at our institution; thus, it is exempt from review, and patient consent was not sought.
The ACS-NSQIP encodes procedures using current procedural terminology (CPT) codes and diagnoses with International Classification of Diseases (ICD), 9th or 10th Revision, Clinical Modification codes. Patients were included if they had CPT code 22612 (arthrodesis, posterior or posterolateral technique, single-level; lumbar [with lateral transverse technique, when performed]). Patients were excluded if they (1) were <18 years old; (2) had an ASA score of ≥4 because these patients are unlikely to be considered candidates for discharge on postoperative day 1; (3) underwent an emergency or nonelective procedure; (4) received a multilevel fusion (identified by CPT code 22614); (5) received an adjunctive posterior or anterior lumbar interbody fusion; (6) had undergone a procedure that was not performed by either a neurosurgeon or orthopedic surgeon; (7) had a postoperative ICD or CPT code corresponding to a deformity, infection, malignancy, or fracture; (8) had undergone a revision procedure, (9) had a missing discharge date, or (10) had undergone a staged procedure, defined as a related, planned reoperation for spinal fusion during the same admission (Fig. 1).
Several variables as predictors of primary and secondary endpoints were collected from the ACS-NSQIP database. The following data were collected: patient age, sex, race, height, weight, ASA classification, functional status (independent or dependent), elective admission status, diabetes, smoking, chronic obstructive pulmonary disease, congestive heart failure, hypertension, corticosteroid use for a chronic condition, hematocrit, sodium, partial thromboplastin time (PTT), international normalized ratio (INR), platelets, and leukocyte count. Age was categorized at the 25th and 75th percentiles for the eligible study population, which resulted in age groups 18–54 years, 55–71 years, and >71 years. Anemia was defined as <41% in males and <36% in females. Platelets were categorized as <150,000/µL or ≥150,000/µL; leukocytes as ≥12,000/µL, <4,000/µL, or in between; albumin as ≥3 g/dL or <3 g/dL; sodium as ≥135 mEq/L or <135 mEq/L; PTT as >40 seconds or ≤40 seconds; and INR as >1.4 or ≤1.4. Height and weight were used to calculate the body mass index (kg/m2) and then categorized into World Health Organization (WHO) class I obesity (30–34.9 kg/m2), WHO class ≥II obesity (≥36 kg/m2), and nonobese. Each patient’s primary postoperative diagnosis, reported with ICD codes, was collected from the registry and categorized into the following groups: spinal stenosis, degenerative disk disease (DDD), disk displacement, spondylosis, and spondylolisthesis.
Numerous procedural/hospital characteristics were also analyzed. Information regarding the surgeon’s specialty, operation length, and use of a graft (CPT codes 20930, 20931, and 20936–20938) was also collected. Operative time was categorized by selecting the 30-minute intervals nearest to the 50th and 75th percentiles of the eligible study population (150 minutes and 220 minutes, respectively). The graft type was categorized as allograft or autograft.
The primary outcome of interest was LOS, measured as the number of calendar days between the day the procedure was performed and the day of discharge. The study specifically focused on patient characteristics and operative factors that resulted in LOS of >1 day; therefore, the study population was divided into cohorts of individuals having LOS ≤1 day and LOS >1 day. Based on this categorization, patients in the LOS ≤1 day cohort were either discharged on the same day of the procedure or after 1 night of overnight observation.
A concern in discharging patients early or performing procedures in the ambulatory setting is that those who experience complications may not be immediately recognized and treated. The secondary endpoints of our study were readmission rates and postdischarge complication rates within 30 days including reoperation, blood transfusion, wound-related infection (both superficial and deep incisional surgical site infections), deep venous thrombosis (DVT), pulmonary embolism (PE), sepsis (including septic shock), pneumonia, urinary tract infections, myocardial infarction, unplanned intubation, wound dehiscence, failure to wean from the ventilator within 48 hours, and acute renal failure. The predischarge complication rates were also compared to better understand which complications precluded patients from being discharged within 1 day.
Missing data in the ACS-NSQIP database reflect laboratory values that were either not obtained preoperatively or were missing from the registry. Baseline rates of missing data were assessed for each laboratory value and were then imputed using a nonparametric multiple imputation missForest method, based on the random forest machine-learning approach [11]. Variables imputed in this manner included hematocrit, leukocyte count, platelet count, sodium, PTT, and INR.
To determine the baseline differences between patients with LOS >1 day and ≤1 day, unadjusted comparisons were first performed between groups using Pearson’s chi-square tests for categorical variables and independent two-sided Student t-tests for continuous variables. To evaluate for predictors of LOS >1 day, separate univariate logistic regression analyses were first performed to screen each covariate for its ability to predict LOS >1 day; thereafter, covariates with a p-value of <0.20 in the univariate analysis and present in >1.0% of the study population were entered into the final multivariate logistic regression model.
To elucidate whether individuals discharged within 1 day were at greater risk for postdischarge complications, a propensity-score matching algorithm was utilized to select LOS >1 day and LOS ≤1 day cohorts for comparison using all collected covariates; therefore, the selected cohorts should be similar with respect to these characteristics. Patients from the LOS >1 day group were paired with those from the LOS ≤1 day group in a 1:1 ratio using a balanced nearest-neighbor approach. Baseline characteristics were compared in the matched groups using Pearson’s chi-square test and Welch’s two-sample t-test to ensure that differences were eliminated by matching.
Which patients who were discharged within 1 day and were most likely to be readmitted within 30 days were also sought. To accomplish this, a backward stepwise logistic regression analysis over all collected covariates with 30-day readmission as the outcome and reported readmission rates by each covariate subgroup as percentages of the population within that subgroup was performed [12,13].
A p-value of <0.05 was defined a priori to represent statistical significance; however, because 26 independent comparisons were made between matched and unmatched groups with respect to covariates, Bonferroni multiple comparisons correction was applied. After correction, the p-value for significance was adjusted to <0.002 for the entire study [14]. Accordingly, 99.8% confidence intervals (CI) were reported for all odds ratios (OR). All statistical analyses were performed using R ver. 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria), and propensity-score matching was performed using the R package MatchIt ver. 3.0.2 (R Foundation for Statistical Computing) [15].
A total of 41,941 patients were identified in the ACS-NSQIP database as having undergone a TLIF between 2011 and 2018. After applying all the exclusion criteria, a total of 12,664 patients were deemed eligible for the study, of whom 1,879 (14.8%) had LOS ≤1 day and 10,785 (85.2%) had LOS >1 day. The mean age of the study population was 62.3±12.8 years, with 6,966 being female (55.0%). The most common diagnostic category was spinal stenosis, followed by spondylolisthesis and DDD. A complete listing of patient demographics and comorbidities for the entire study population is presented in Table 1.
The results of the multivariable logistic regression model for LOS are presented in Table 2. Associations were noted between increased LOS and female sex (OR, 1.74; 99.8% CI, 1.49–2.06; p<0.001), Hispanic identity (OR, 1.55; 99.8% CI, 1.04–2.38; p=0.001), diagnosis of spondylolisthesis (OR, 1.46; 99.8% CI, 1.17–1.83; p<0.001), ASA category 3 (OR, 1.42; 99.8% CI, 1.18–1.7; p<0.001), and operation lengths of 150–220 minutes (OR, 3.76; 99.8% CI, 3.07–4.64; p<0.001) and >220 minutes (OR, 8.01; 99.8% CI, 5.96–11.0; p<0.001) (Fig. 2).
All baseline differences between the study cohorts were completely eliminated by propensity-score matching, and the resulting matched groups were similar in all collected characteristics (Supplement 1). In terms of predischarge complication rates, patients who had LOS >1 day were more likely to have received intraoperative or postoperative blood transfusions (0.3% versus 4.5%, p<0.001) and were more likely to have undergone reoperations (0.1% versus 0.6%, p=0.004), although the latter did not reach statistical significance upon multivariable logistic regression (Table 2). No significant differences in the postdischarge complication rates were found between the matched cohorts.
Table 3 presents the results of the stepwise logistic regression model for 30-day unplanned readmission for patients with LOS ≤1 day. The factors that demonstrated the strongest associations were female sex, dependent functional status, hypertension, chronic steroid use, and thrombocytopenia. Of these, dependent functional status was the only significant predictor of readmission in the cohort of patients who were discharged on or before postoperative day 1 (OR, 8.4; 99.8% CI, 1.75–30.41; p=0.001).
This study presents a review of patient and intraoperative factors and complications associated with LOS ≤1 day for single-level TLIF between 2011 and 2018 using the ACS-NSQIP database. In this study, female sex, Hispanic ethnicity, diagnosis of spondylolisthesis, ASA classification 3, and operation lengths of 150–220 minutes and >220 minutes were found to be associated with LOS >1 day. Patients with LOS >1 day who received intraoperative or postoperative blood transfusions were more likely to undergo a reoperation. However, no differences were found for the 30-day readmission rates or postdischarge complication rates between the LOS ≤1 day and LOS >1 day cohorts. In the LOS ≤1 day cohort, dependent functional status was significantly associated with unplanned readmission within 30 days.
Female sex, which represented 55.0% of the cohort in this study, was a significant risk factor for LOS >1 day. This may be due to an increasing number of female patients undergoing spine surgery and the gender bias in female patients using more medical care than male patients [16,17]. This finding is consistent with those of previous studies, although conflicting results have also revealed that men had a greater risk of reoperation after lumbar spine surgery [17,18]. Socioeconomic status in relation to race, insurance status, and marriage affects surgical outcomes [19]. One study of 1,896 patients undergoing cervical spine surgery showed extended LOS in patients identified as non-White, which is similar to our study population [20]. However, this finding remains controversial because other studies have not found an association between race and clinical outcomes [21].
Preoperative spondylolisthesis was associated with LOS >1 day compared with other indications for single-level TLIF. Spondylolisthes result from the degeneration of the weight-bearing facet joints, leading to the anatomical slippage of the vertebrae and altering the sagittal balance of the spine [22]. Consequently, hyperlordosis of the spine occurs as a compensatory mechanism; therefore, additional inpatient management such as physical and occupational therapy may convey a perceived postoperative benefit [6,9]. Other studies have suggested that surgical intervention for spondylolisthesis has better outcomes than other indications such as DDD or spinal stenosis, although these studies focus on long-term outcomes rather than on postoperative LOS [23,24]. Higher ASA class has been well established with longer LOS, complications, and readmission after spine surgery and was consistent with our findings [17].
Intraoperative factors of operation lengths of 150–220 minutes and >220 minutes were associated with LOS >1 day. In the LOS >1 day cohort, they were associated with receiving a perioperative blood transfusion and undergoing unplanned reoperation. Cases with longer operating times have increased complexity, leading to increased estimated blood loss and risk of complications [7,17]. Furthermore, patients who receive perioperative blood transfusions are more likely to have higher estimated blood loss and/or lower preoperative hemoglobin levels, indicating a higher likelihood of preexisting comorbidities [7]. Increased rates of unplanned reoperation may result from the increased complexity and complications in these patients [25]. Overall, these results are consistent with those of previous studies. A case series of 78 patients undergoing single-level minimally invasive (MIS) TLIF similarly found that patients who had higher estimated blood loss, lower preoperative hemoglobin levels, and longer operating times were likely to have LOS >1 day [26]. Another study of 4,995 patients undergoing single-level TLIF showed that longer operative times were associated with higher readmission rates [17].
Regardless of whether patients were discharged within 1 day or >1 day, no differences in postdischarge complications and readmissions were found. However, among patients with LOS ≤1 day, those with dependent functional status were associated with readmission within 30 days. This increased readmission rate may be explained by functionally dependent patients who are more likely to have complicated medical histories and are potentially more likely to require assistance with activities of daily living [27,28]. In cervical spine and orthopedic surgeries, a dependent functional status has been associated with increased readmission rates and worse outcomes, such as nonhome discharge, prolonged hospital stay, reoperation, and reintubation, which is consistent with our results [27,28].
As a retrospective national database study, its limitations must be noted. In particular, the variables in the ACS-NSQIP database are predetermined and were not originally constructed to analyze risk factors associated with single-level TLIF. In addition, both open and MIS approaches for single-level TLIF use the same CPT code; thus, distinguishing between the two approaches using the NSQIP database is impossible. MISTLIF is known to have shorter LOS, fewer complications, and improved functional recovery [29,30]. As such, the analysis may bias LOS ≤1 day to incorporate more patients with MIS-TLIF compared with LOS >1 day. Furthermore, variables such as hematoma formation and screw misplacement are not quantified in the database, which may further elucidate why patients undergo reoperation. In addition, postoperative complications previously shown to significantly affect LOS, such as DVT, PE, and pneumonia had low incidence rates in the NSQIP database, indicating the need for a larger sample size to accurately quantify the risk of these complications. Similarly, data on the exact causes of certain outcomes, such as unplanned readmission or reoperation are not available in the NSQIP database, warranting additional prospective studies to identify these causes. However, surgeons may consider these perioperative factors for patients undergoing single-level TLIF as an ambulatory procedure or those requiring inpatient management.
This study using the ACS-NSQIP database for single-level TLIF revealed that patients with a higher ASA class, diagnosis of spondylolisthesis, female sex, Hispanic identity, and prolonged operative time were more associated with LOS >1 day. Patients with LOS >1 day were associated with perioperative blood transfusions and unplanned reoperations. For patients with LOS ≤1 day, a dependent functional status was associated with unplanned 30-day readmission. These factors should be considered when selecting patients for single-level TLIF to reduce the risk of prolonged hospitalization and associated complications.
Acknowledgments
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) and the hospitals participating in the ACS-NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Supplementary Materials
Supplementary materials can be available from https://doi.org/10.31616/asj.2023.0372.
Supplement 1.
Baseline characteristics of the propensity-score matched cohorts.
Fig. 1.
Identification and exclusion of patient population. NSQIP, National Surgical Quality Improvement Program; TLIF, transforaminal lumbar interbody fusion; ASA, American Society of Anesthesiologists; PLIF, posterior lumbar interbody fusion; ALIF, anterior lumbar interbody fusion; LOS, length of stay.
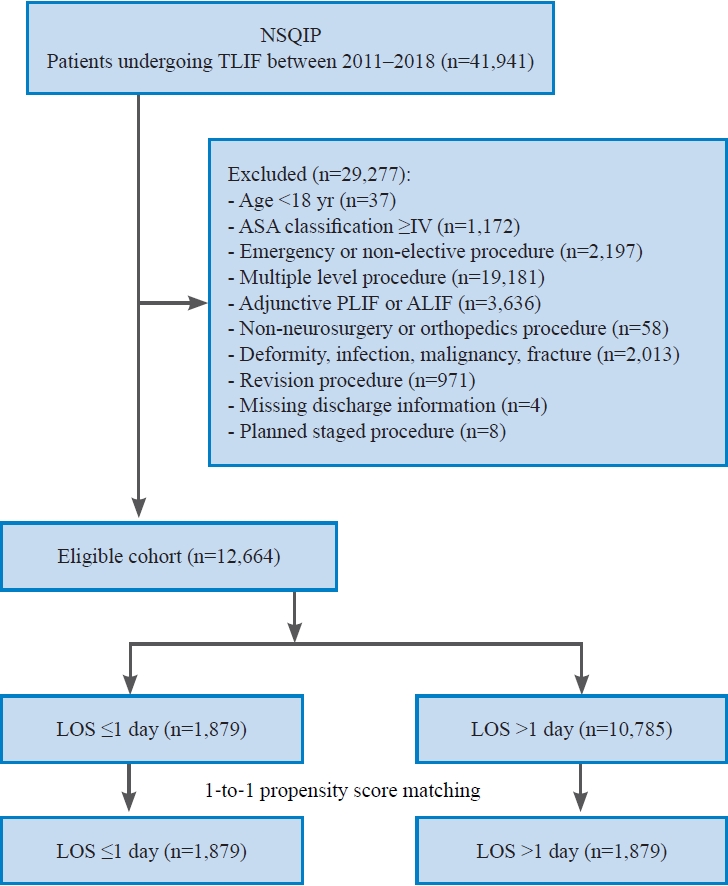
Fig. 2.
Multivariate logistic regression analysis of predictors for length of stay (LOS) >1 day; bold indicates significance (α=0.002) after applying Bonferroni correction. CI, confidence interval; Ref, reference; ASA, American Society of Anesthesiologists classification; DDD, degenerative disc disease.
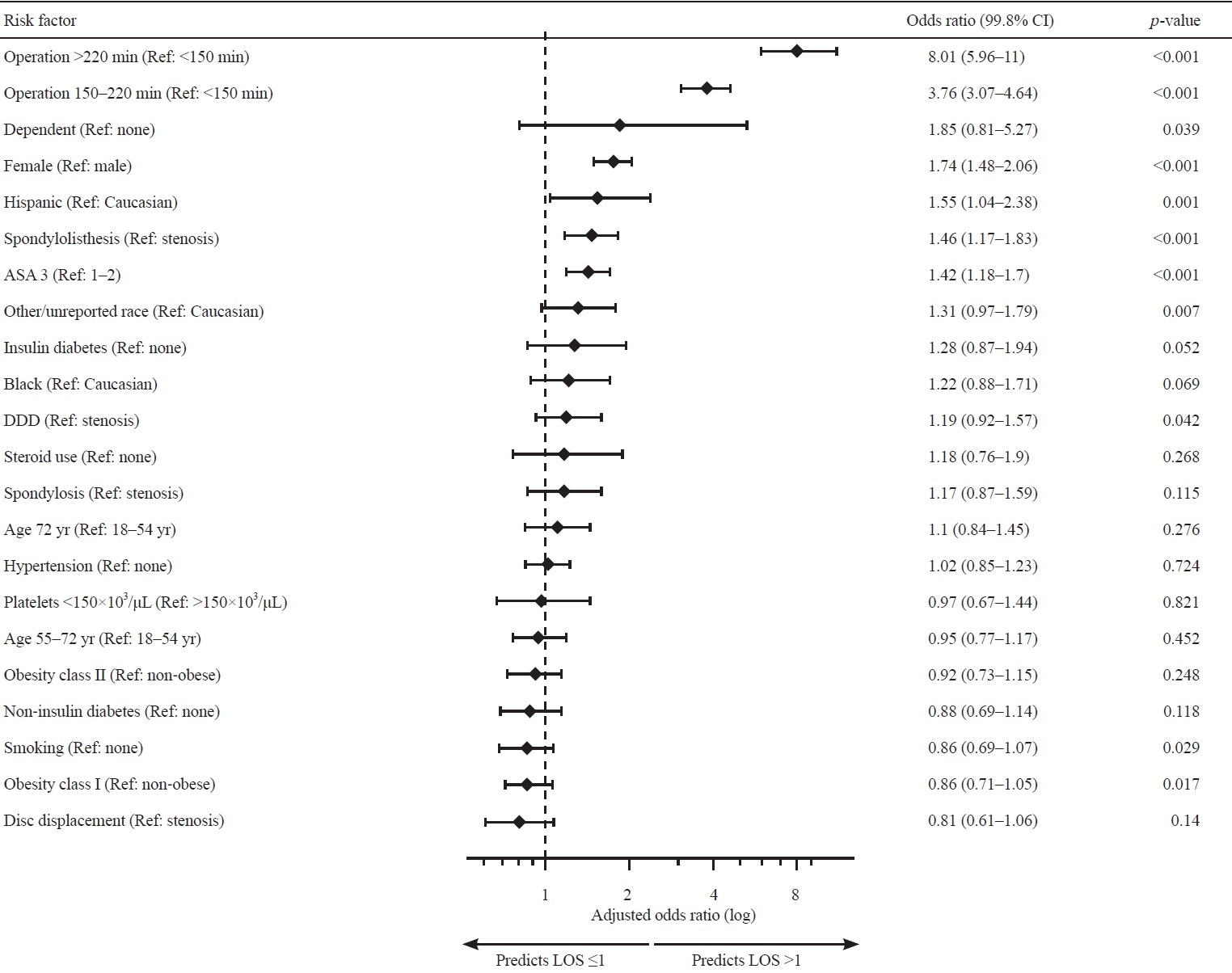
Table 1.
Demographics and operative characteristics of the study population
| Characteristic | Total (n=12,664) | LOS ≤1 day (n=1,879) | LOS >1 day (n=10,785) | p-valuea) |
|---|---|---|---|---|
| Age (yr) | 62.3±12.8 | 61.6±12.9 | 62.4±12.8 | 0.015 |
| Female | 6,966 (55.0) | 856 (45.6) | 6,110 (56.7) | <0.001b) |
| Race | <0.001b) | |||
| Caucasian | 9,891 (78.1) | 1,548 (82.4) | 8,343 (77.4) | |
| Black | 974 (7.7) | 119 (6.3) | 855 (7.9) | |
| Hispanic | 668 (5.3) | 73 (3.9) | 595 (5.5) | |
| Other/not reported | 1,131 (8.9) | 139 (7.4) | 992 (9.2) | |
| Primary diagnosis | <0.001b) | |||
| Spinal stenosis | 5,785 (45.7) | 943 (50.2) | 4,842 (44.9) | |
| Spondylolisthesis | 3,076 (24.3) | 327 (17.4) | 2,749 (25.5) | |
| Degenerative disc disease | 1,479 (11.7) | 215 (11.4) | 1,264 (11.7) | |
| Disc displacement | 1,168 (9.2) | 235 (12.6) | 932 (8.6) | |
| Spondylosis | 1,156 (9.1) | 158 (8.4) | 998 (9.3) | |
| ASA classification | <0.001b) | |||
| 1–2 | 6,311 (49.8) | 1,088 (57.9) | 5,223 (48.4) | |
| 3 | 6,353 (50.2) | 791 (42.1) | 5,562 (51.6) | |
| Obesity | 0.02 | |||
| WHO class I | 3,518 (27.8) | 553 (29.4) | 2,965 (27.5) | |
| WHO class II or III | 2,896 (22.9) | 385 (20.5) | 2,511 (23.3) | |
| Dependent functional status | 179 (1.4) | 13 (0.7) | 166 (1.5) | 0.015 |
| Diabetes mellitus | 0.029 | |||
| Non-insulin | 1,666 (13.2) | 251 (13.4) | 1,415 (13.1) | |
| Insulin | 719 (5.7) | 82 (4.4) | 637 (5.9) | |
| Current smoker | 2,205 (17.4) | 367 (19.5) | 1,838 (17.0) | 0.009 |
| Hypertension | 7,546 (59.6) | 1,080 (57.5) | 6,466 (60.0) | 0.044 |
| Chronic obstructive pulmonary disease | 578 (4.6) | 79 (4.2) | 499 (4.6) | 0.412 |
| Congestive heart failure | 31 (0.2) | 4 (0.2) | 27 (0.3) | 0.762 |
| Chronic steroid use | 522 (4.1) | 59 (3.1) | 463 (4.3) | 0.02 |
| Anemia | 2,421 (19.5) | 342 (18.2) | 2,129 (19.7) | 0.12 |
| Leukocytes | 0.650 | |||
| ≥12,000/μL | 401 (3.2) | 53 (2.8) | 348 (3.2) | |
| <4,000/μL | 49 (2.0) | 37 (2.0) | 212 (2.0) | |
| Platelets <150,000/μL | 564 (4.5) | 94 (5.0) | 470 (4.4) | 0.196 |
| Sodium <135 mEq/L | 553 (4.4) | 86 (4.6) | 467 (4.3) | 0.629 |
| Partial thromboplastin time >40 sec | 80 (0.6) | 8 (0.4) | 72 (0.6) | 0.012 |
| International normalized ratio >1.4 | 73 (0.6) | 12 (0.6) | 61 (0.6) | 0.7 |
| Surgeon specialty | 0.879 | |||
| Neurosurgery | 7,279 (57.5) | 1,077 (57.3) | 6,202 (57.5) | |
| Orthopedics | 5,385 (42.5) | 802 (42.7) | 4,583 (42.5) | |
| Autograft | 6,288 (49.7) | 922 (49.1) | 5,366 (49.8) | 0.583 |
| Allograft | 4,316 (34.1) | 640 (34.1) | 3,076 (34.1) | 0.984 |
| Operative time (min) | <0.001b) | |||
| <150 | 5,845 (46.2) | 1,440 (76.6) | 4,405 (40.8) | |
| 150–220 | 3,890 (30.7) | 318 (16.9) | 3,572 (33.1) | |
| >220 | 2,929 (23.1) | 121 (6.4) | 2,808 (26.0) |
Table 2.
Comparison of pre- and post-discharge complications within 30 days between matched cohorts
| Outcome |
Pre-discharge |
Post-discharge |
||||
|---|---|---|---|---|---|---|
| LOS ≤1 day (n=1,879) | Matched LOS >1 day (n=1,879) | p-valuea) | LOS ≤1 day (n=1,879) | Matched LOS >1 day (n=1,879) | p-valuea) | |
| Intraoperative durotomy | 6 (0.3) | 13 (0.7) | 0.107 | - | - | - |
| Intraoperative or postoperative blood transfusion | 6 (0.3) | 85 (4.5) | <0.001b) | 1 (0.1) | 0 | 0.317 |
| Unplanned readmission | - | - | - | 61 (3.2) | 69 (3.7) | 0.475 |
| Unplanned reoperation | 1 (0.1) | 11 (0.6) | 0.004 | 26 (1.4) | 27 (1.4) | 0.89 |
| Deep venous thrombosis | 0 | 0 | 1.000 | 3 (0.2) | 8 (0.4) | 0.131 |
| Pulmonary embolism | 0 | 1 (0.1) | 0.317 | 3 (0.2) | 0 | 0.317 |
| Sepsis | 5 (0.3) | 12 (0.6) | 0.089 | 0 | 0 | 1.000 |
| Pneumonia | 0 | 5 (0.3) | 0.025 | 3 (0.2) | 4 (0.2) | 0.705 |
| Urinary tract infection | 1 (0.1) | 3 (0.2) | 0.317 | 10 (0.5) | 8 (0.4) | 0.637 |
| Wound-related infection | 14 (0.7) | 15 (0.8) | 0.852 | 15 (0.8) | 27 (1.4) | 0.063 |
| Wound dehiscence | 2 (0.1) | 6 (0.3) | 0.157 | 0 | 0 | 1.000 |
| Myocardial infarction | 0 | 5 (0.3) | 0.025 | 2 (0.1) | 4 (0.2) | 0.414 |
| Unplanned intubation | 2 (0.1) | 5 (0.3) | 0.256 | 0 | 2 (0.1) | 0.157 |
| Acute renal failure | 0 | 0 | 1.000 | 0 | 1 (0.1) | 0.317 |
Table 3.
Stepwise logistic regression model for predictors of 30-day unplanned readmission in patients discharged within 1 day
| Factor | Crude % readmitteda) | OR (99.8% CI) | p-value |
|---|---|---|---|
| Female sex | 22/856 (2.6) | 0.67 (0.38–1.16) | 0.159 |
| Dependent functional status | 3/13 (2.3) | 8.40 (1.75–30.41) | 0.001b) |
| Hypertension | 43/1,080 (4.0) | 1.60 (0.92–2.89) | 0.102 |
| Steroid | 4/59 (6.8) | 2.41 (0.70–6.27) | 0.105 |
| Platelets <150,000/μL | 8/94 (8.5) | 2.39 (0.99–5.10) | 0.036 |
References
1. Goz V, Weinreb JH, Schwab F, Lafage V, Errico TJ. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: an analysis of the Nationwide Inpatient Sample database. Spine J 2014;14:2019–27.


2. Grotle M, Smastuen MC, Fjeld O, et al. Lumbar spine surgery across 15 years: trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open 2019;9:e028743.



3. Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976) 2019;44:369–76.


4. Saifi C, Cazzulino A, Laratta J, et al. Utilization and economic impact of posterolateral fusion and posterior/transforaminal lumbar interbody fusion surgeries in the United States. Global Spine J 2019;9:185–90.




5. Zhan H, Guo R, Xu H, et al. Hospital length of stay following first-time elective open posterior lumbar fusion in elderly patients: a retrospective analysis of the associated clinical factors. Medicine (Baltimore) 2019;98:e17740.



6. Benton JA, Ramos RG, Gelfand Y, et al. Prolonged length of stay and discharge disposition to rehabilitation facilities following single-level posterior lumbar interbody fusion for acquired spondylolisthesis. Surg Neurol Int 2020;11:411.



7. Kobayashi K, Ando K, Kato F, et al. Predictors of prolonged length of stay after lumbar interbody fusion: a multicenter study. Global Spine J 2019;9:466–72.




8. Eckman WW, Hester L, McMillen M. Same-day discharge after minimally invasive transforaminal lumbar interbody fusion: a series of 808 cases. Clin Orthop Relat Res 2014;472:1806–12.


9. Lee KE, Martin TA, Peterson KA, Kittel C, Zehri AH, Wilson JL. Factors associated with length of stay after singlelevel posterior thoracolumbar instrumented fusion primarily for degenerative spondylolisthesis. Surg Neurol Int 2021;12:48.



10. Karhade AV, Larsen AM, Cote DJ, Dubois HM, Smith TR. National databases for neurosurgical outcomes research: options, strengths, and limitations. Neurosurgery 2018;83:333–44.


11. Stekhoven DJ, Buhlmann P. MissForest: non-parametric missing value imputation for mixed-type data. Bioinformatics 2012;28:112–8.



13. Venables WN, Ripley BD. Modern applied statistics with S. 4th ed. New York (NY): Springer; 2002.
15. Stuart EA, King G, Imai K, Ho D. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw 2011;42:1–28.
16. MacLean MA, Touchette CJ, Han JH, Christie SD, Pickett GE. Gender differences in the surgical management of lumbar degenerative disease: a scoping review. J Neurosurg Spine 2020;1–18.


17. Garcia RM, Khanna R, Dahdaleh NS, Cybulski G, Lam S, Smith ZA. Thirty-day readmission risk factors following single-level transforaminal lumbar interbody fusion (TLIF) for 4992 patients from the ACS-NSQIP database. Global Spine J 2017;7:220–6.




18. Kobayashi Y, Ogura Y, Kitagawa T, et al. Gender differences in pre- and postoperative health-related quality of life measures in patients who have had decompression surgery for lumbar spinal stenosis. Asian Spine J 2020;14:238–44.




19. Ko NY, Hong S, Winn RA, Calip GS. Association of insurance status and racial disparities with the detection of earlystage breast cancer. JAMA Oncol 2020;6:385–92.



20. Dial BL, Esposito VR, Danilkowicz R, et al. Factors associated with extended length of stay and 90-day readmission rates following ACDF. Global Spine J 2020;10:252–60.




21. Schoenfeld AJ, Lurie JD, Zhao W, Bono CM. The effect of race on outcomes of surgical or nonsurgical treatment of patients in the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 2012;37:1505–15.



22. Tebet MA. Current concepts on the sagittal balance and classification of spondylolysis and spondylolisthesis. Rev Bras Ortop 2014;49:3–12.



23. Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Single-level lumbar fusion for degenerative disc disease is associated with worse outcomes compared with fusion for spondylolisthesis in a workers’ compensation setting. Spine (Phila Pa 1976) 2015;40:323–31.


24. Carreon LY, Glassman SD, Howard J. Fusion and nonsurgical treatment for symptomatic lumbar degenerative disease: a systematic review of Oswestry Disability Index and MOS Short Form-36 outcomes. Spine J 2008;8:747–55.


25. Liu JM, Deng HL, Peng AF, et al. Unplanned reoperation of lumbar spinal surgery during the primary admission: a multicenter study based on a large patient population. Spine (Phila Pa 1976) 2016;41:1279–83.



26. Siemionow K, Pelton MA, Hoskins JA, Singh K. Predictive factors of hospital stay in patients undergoing minimally invasive transforaminal lumbar interbody fusion and instrumentation. Spine (Phila Pa 1976) 2012;37:2046–54.


27. Minhas SV, Mazmudar AS, Patel AA. Pre-operative functional status as a predictor of morbidity and mortality after elective cervical spine surgery. Bone Joint J 2017;99-B:824–8.



28. Burton BN, Lin TC, A’Court AM, Schmidt UH, Gabriel RA. Dependent functional status is associated with unplanned postoperative intubation after elective cervical spine surgery: a national registry analysis. J Anesth 2018;32:565–75.










