Do different pathologies of adult spinal deformity (idiopathic lumbar scoliosis against de novo lumbar scoliosis) affect preoperative and postoperative selfimage?
Article information
Abstract
Study Design
Retrospective single-center study.
Purpose
This study aimed to examine the factors associated with the self-image domain of the Scoliosis Research Society-22 revised (SRS-22r) in patients who underwent corrective surgery for adult idiopathic scoliosis (AdIS).
Overview of Literature
Adult spinal deformity (ASD) can be classified into AdIS and de novo scoliosis. However, no studies have investigated the effect of different ASD pathologies on self-image.
Methods
This study enrolled 60 patients who underwent corrective surgery and were followed up for >2 years postoperatively. AdIS was defined as adolescent idiopathic scoliosis in patients who had no history of corrective surgery, had a primary thoracolumbar/lumbar (TL/L) curve, and were ≥30 years old at the time of surgery.
Results
The AdIS (n=23; mean age, 53.1 years) and de novo (n=37; mean age, 70.0 years) groups were significantly different in terms of the main thoracic and TL/L curves, sagittal vertical axis, thoracic kyphosis, and thoracolumbar kyphosis preoperatively. The scores in the self-image domain of the SRS-22r (before surgery/2 years after surgery [PO2Y]) were 2.2/4.4 and 2.3/3.7 in the AdIS and de novo groups, respectively, and PO2Y was significantly different between the two groups (p<0.001). Multivariate regression analysis revealed that AdIS was an independent factor associated with self-image at PO2Y (p=0.039).
Conclusions
AdIS, a spinal deformity pathology, was identified as a significant factor associated with the self-image domain of SRS-22r in patients who underwent corrective surgery. AdIS is not solely classified based on pathology but also differs in terms of the clinical aspect of self-image improvement following corrective surgery.
Introduction
In the last decade, surgical outcomes of corrective surgery in adult spinal deformity (ASD) have considerably improved, owing to the establishment of the deformity classification [1], target alignment [2-4], osteotomy classification [5], and prevention of perioperative complications [6,7]. Surgical intervention may be necessary for patients with ASD exhibiting symptoms resistant to conservative treatment, such as back pain, claudication [8], visceral disturbance [9], and depression caused by physical appearance concerns [10]. Previous studies have reported improved postoperative health-related quality of life (HRQOL) in patients with ASD [11-14]. Corrective surgery could provide better HRQOL than conservative treatment, and postoperative HRQOL was maintained at a minimum of 5 years of follow-up. However, data on the self-image of patients with ASD remain limited. Notably, the importance of appearance in patients with adolescent idiopathic scoliosis (AIS) has been extensively reported [15,16], and low self-image scores on the Scoliosis Research Society-22 revised (SRS-22r) questionnaire for patients with ASD appear to be a substantial driving factor for surgical decision-making [17]. In addition, body disfigurement negatively affects self-image, decreasing self-esteem, and social confidence [18]. These findings collectively suggest that trunk asymmetry, prominence, and trunk shortening negatively affect self-image and mental health.
Adult scoliosis can be classified primarily into adult idiopathic scoliosis (AdIS) and de novo scoliosis [8,19]. Patients with AdIS exhibit relatively more extensive scoliosis and degenerative changes superimposed on the preexisting curve. For instance, Hori et al. [20] showed that patients with Lenke 5C often demonstrate a greater thoracolumbar/lumbar (TL/L) curve, which leads to thoracolumbar kyphosis and subsequent lumbar hypolordosis, followed by pelvic retroversion and sagittal imbalance after compensation failure. In contrast, patients with de novo scoliosis show kyphoscoliosis in the lumbosacral area, primarily due to disk degeneration. Differences in deformity type can result in distinct trunk shapes, which may lead to different perceptions of physical appearance and cosmetic issues.
A recent cross-sectional study revealed a negative correlation between the radiological parameters of patients with AdIS and their self-image score on SRS-22 [21]. In addition, a study indicated that patients with AdIS had significantly worse scores on the self-image domain of the SRS-22r than age- and sex-matched healthy volunteers [22]. However, no studies have investigated the effect of different ASD pathologies on self-image following corrective surgery. We hypothesized that the self-image domain of SRS-22r in patients with AdIS would more likely improve following corrective fusion surgery than that in patients with de novo scoliosis. Thus, this study aimed to investigate the factors associated with the self-image domain of SRS-22r in patients with AdIS or de novo scoliosis following corrective surgery.
Materials and Methods
Ethical statements
This retrospective cohort study protocol was approved by the Institutional Review Board of Osaka City General Hospital (approval no., 1305011). All study participants provided informed consent.
Patients
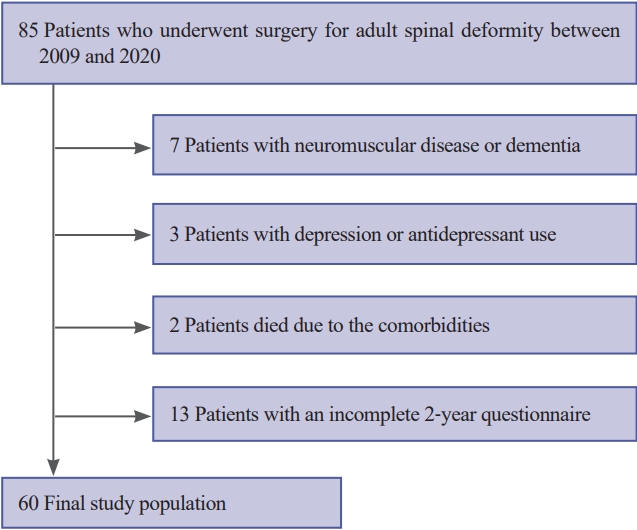
This study enrolled 85 patients with ASD who underwent corrective surgery by a single surgeon at a single institution between 2009 and 2020. Patients diagnosed with spinal deformity associated with congenital and neuromuscular diseases and those with a history of depression, psychiatric issues, or use of duloxetine and antidepressant medications were excluded. Patients who could not complete patient-oriented questionnaires 2 years postoperatively were also excluded. AdIS was defined (1) diagnosis of AIS, (2) no history of corrective surgery, (3) lumbar/thoracolumbar main curve, and (4) age ≥30 years at the time of surgery. The definition of age for AdIS was based on a previous report [22].
Radiographic evaluation
The following radiographic parameters were evaluated via standing posterior–anterior and lateral radiographs immediately before surgery, 2 weeks after surgery (PO2W), and 2 years after surgery (PO2Y): (1) Cobb angle of the main thoracic (MT) and main TL/L curve (TL/L), (2) distance between the C7-plumb line and the center for the sacral vertical line (C7–CSVL), (3) C7 sagittal vertical axis (C7–SVA), (4) degree of thoracic kyphosis (TK; T5–12), (5) degree of thoracolumbar kyphosis (TLK; T10–L2), (6) degree of lumbar lordosis (LL; T12–S1), (7) pelvic tilt (PT), and (8) pelvic incidence. All radiographic parameters were measured using the Synapse three-dimensional viewer software OB-V (Fuji Film Co., Tokyo, Japan).
Perioperative complication
Perioperative complications assessed included medical and surgical events. As regards mechanical complications, proximal junctional kyphosis (PJK) and rod fractures were evaluated. PJK was defined according to the criteria outlined by Bridwell et al. [23], which include (1) vertebral fractures at the upper instrumented vertebrae (UIV), UIV+1, and UIV-1 and (2) a change in the proximal junctional angle of ≥20° compared with the preoperative measurement.
Clinical evaluation
Two patient-oriented questionnaires, the Japanese edition of the SRS-22r and the 36-item Short-Form Health Survey (SF-36), were used to evaluate HRQOL before surgery and at PO2Y. The physical component summary (PCS) and mental component summary (MCS) of the SF-36 were computed as previously described [24]. The achievement of minimal clinically important differences (MCIDs) for the SRS-22r domains at PO2Y was calculated. The previously reported MCID values for each domain were as follows: function, 0.90; pain, 0.85; self-image, 1.05; mental health, 0.70; and subtotal, 1.05 [25].
Statistical analysis
The patients were classified into two groups based on our definition of AdIS, namely, the AdIS and de novo groups. Demographic data and radiographic parameters were compared between these groups. Fisher’s exact test was used to evaluate categorical variables, and the Mann-Whitney U test was employed to evaluate continuous variables in the univariate analysis. Multiple linear regression analyses were also performed to determine the association between AdIS and clinical scores recorded before surgery and at PO2Y. Explanatory variables included spinal deformity pathology (AdIS or de novo) and statistically significant variables in the univariate analysis. SRS-22r scores recorded before surgery and at PO2Y were considered objective variables. Furthermore, propensity score matching was performed to adjust for background data in the two groups as a subgroup analysis. To estimate the propensity score, a logistic regression model was fitted using the patient’s age, sex, preoperative PCS and MCS of the SF-36, and subtotal SRS-22r score. Clinical scores were compared between the two matched groups. All analyses were performed using R ver. 3.5.1 (patched; The R Foundation, Vienna, Austria) [26]. Statistical significance was set at p<0.05.
Results
Preoperative status
After implementing the inclusion and exclusion criteria, this study enrolled 60 patients who underwent corrective surgery and were followed up for >2 years (average age at the surgery, 63.3±13.7 years; average number of fused segments, 9.8±1.7; average follow-up period, 58.4±26.0 months) (Fig. 1). Overall, 23 and 37 patients were included in the AdIS and de novo groups, respectively (Table 1).
The AdIS group had a significantly lower mean age at the time of surgery than the de novo group (53.1 years versus 70.0 years, p<0.001). Except for hypertension, no significant differences were observed in other demographic factors and comorbidities between the groups. PJK occurred in seven patients (AdIS group [n=1], de novo group [n=6]), and no significant difference was found between these groups (p=0.399). In addition, no significant differences in the number of fused segments, surgical procedures, surgical site infection, or opioid use at the time of discharge were observed between the two groups.
Radiographic evaluation
Table 2 presents the comparisons of radiographic data between the AdIS and de novo groups. Significant differences in preoperative TL/L, MT, C7–SVA, TK, and TLK were found between the two groups (TL/L: 60.5° versus 35.7°, p<0.001; MT: 38.4° versus 19.3°, p=0.003; C7–SVA: 53.4 mm versus 98.3 mm, p=0.009; TK: 10.9° versus 18.9°, p=0.024; and TLK: 23.5° versus 11.7°, p=0.020). TL/L, MT, and TK were also significantly different at PO2Y between the AdIS and de novo groups (TL/L: 22.2° versus 13.7°, p<0.001; MT: 19.2° versus 6.8°, p=0.002; and TK: 26.3° versus 37.0°, p<0.001). However, no radiographic parameters were significantly differed between PO2W and PO2Y.
Clinical outcomes
Table 3 presents the comparisons of clinical outcomes based on SRS-22r between the two groups. The comparative analysis indicated that all SRS-22r domains, except for self-image, and PCS of SF-36 were significantly lower in the de novo group than in the AdIS group preoperatively, and the pain and mental health domains of SRS-22r and MCS of SF-36 were comparable between the two groups at PO2Y. The self-image in the AdIS group was comparable with that in the de novo group preoperatively; however, the AdIS group had significantly higher self-image than the de novo group at PO2Y. The satisfaction domain of SRS-22r at PO2Y was significantly higher in the AdIS group than in the de novo group (4.5 versus 4.0, p=0.036). Furthermore, the MCID of the self-image domain of SRS-22r was significantly higher in the AdIS group than in the de novo group (95.7% versus 62.2%, p=0.005). No significant differences were noted in the other domains of SRS-22r between the two groups.
Related factor analysis for self-image
A comparative analysis of the factors contributing to self-image was conducted both before surgery and at PO2Y. Based on the results, the following potential parameters were selected as explanatory variables: spinal deformity pathology (AdIS or de novo), sex, age, TL/L, C7–SVA, PT, TK, and TLK. Although the preoperative multivariate regression analysis did not reveal any significant factors associated with self-image, TL/L exhibited a slight trend (p=0.053). However, the multivariate analysis conducted at PO2Y identified AdIS, a spinal deformity pathology, as a significant factor associated with self-image (p=0.039). Table 4 presents the results of these analyses.
Subgroup analysis using propensity score matching
Patients’ age, sex, preoperative PCS and MCS scores of the SF-36, and the subtotal score of the SRS-22r were adjusted, which balanced the distribution of demographic characteristics, including age (59.3 years versus 63.1 years, p=0.497) and preoperative clinical scores between the two matched groups (n=10 per group) (Table 5). The analysis demonstrated that only the self-image domain of SRS-22r at PO2Y was significantly different between the matched groups (4.5 versus 3.8, p=0.008), whereas the remaining surgical outcomes showed no significant differences.
Discussion
To the best of our knowledge, this is the first study to determine whether the different pathological characteristics of spinal deformity affect self-image following ASD surgery. Self-image was not associated with the preoperative radiographic parameters, although the magnitude of the preoperative TL/L curve demonstrated certain tendencies. In addition, self-image in the AdIS group was comparable with that in the de novo group preoperatively; however, self-image in the AdIS group was significantly higher than that in the de novo group at PO2Y. Regarding MCID, only the self-image domain exhibited a significant difference between the two groups. Importantly, multivariate analysis revealed that the pathology of the idiopathic deformity was a significant factor associated with self-image at PO2Y. Moreover, the results of a propensity score-matched analysis, as a subgroup analysis, showed a significant difference in self-image between the matched groups at PO2Y.
Accumulating evidence indicates that appropriate sagittal alignment and mental and medical conditions can affect the HRQOL following ASD surgery. However, the effect of ASD surgery on self-image remains unknown. Raad et al. [27] evaluated 123 patients with ASD with complete data on the SRS-22r and Patient-Reported Outcomes Measurement Information System and concluded that a domain that reflects how patients with ASD perceive their self-image must be developed and validated. Hayashi et al. [28] also analyzed postoperative HRQOL in 391 patients with ASD and found that mental status and sagittal spinopelvic alignment are key determinants of self-image. However, their study enrolled patients with de novo scoliosis and AdIS and were >18 years at the time of surgery. Despite these interesting findings, whether the pathology of spinal deformity affects self-image remains unknown. Several studies on AIS have demonstrated that self-image does not correlate with radiological severity [29,30]. According to Cheshire et al. [31], the self-image domain of SRS-22r has little influence on the external shape of the torso. Considering the complexity of self-image, no single factor is sufficient to explain the self-image of patients with AdIS. However, Weiss et al. [18] demonstrated that body disfigurement negatively affects self-image and decreases self-esteem and social confidence. Patients with AdIS are typically diagnosed during adolescence, and their physical appearance can be compromised for an extended period because of body deformity, resulting in reduced self-confidence and psychological distress. Consequently, self-image may be more critical in patients with AdIS than in those with de novo scoliosis.
Although this study did not find significant correlation between radiographic parameters and self-image, magnitude of the preoperative TL/L curve showed some tendencies to be associated with self-image, with significant differences between the AdIS and de novo groups. Regarding the natural history of AIS, Weiss et al. [18] reported that 68% of the curves progressed after skeletal maturity in 102 patients who were followed up for >40 years. In the Lenke 5C curve AIS, Hori et al. [20] analyzed the prognostic natural history of sagittal and spinopelvic alignment and concluded that scoliotic and rotational deformity progresses to thoracolumbar hyperkyphosis, lumbar hypolordosis, and pelvic retroversion, and sagittal imbalance occurs after compensation failure. Therefore, the increasing magnitude of the TL/L curve and TLK are distinctive parameters in AdIS, with potential correlation with self-image. Understanding the natural history and distinctive radiographic parameters of AdIS may also facilitate the differentiation between AdIS and de novo scoliosis.
This study has some limitations. First, the pathology of spinal deformity was determined based on patient interviews, leading to the inclusion of mild AdIS cases in the de novo group. Second, this study did not find any substantial correlation between coronal radiographic parameters, including the Cobb angle and C7–CSVL, and self-image. Because of the complexity of self-image, these radiographic measurements may not account for all aspects of the deformity affecting self-image perception. Therefore, parameters that contribute to trunk deformities, including shoulder imbalance, waistline asymmetry, and scapula prominence, must be considered. Third, this was a single-surgeon and single-institute study. Fourth, the sample size was small, and the follow-up period was relatively short. Lastly, a psychological evaluation before surgery was not performed. Psychological and psychiatric status may influence self-image; consequently, patients with a history of psychological illness and psychoactive drug use were excluded. Thus, future studies should collaborate with psychologists.
Conclusions
In conclusion, this study highlighted the significant association between AdIS, a spinal deformity pathology, and the self-image domain of the SRS-22r. This emphasizes the importance of distinguishing AdIS from de novo because these conditions differ not only in their pathology but also in the clinical aspect of self-image improvement following corrective surgery.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
All authors participated in the study design, writing, and preparing the manuscript. All authors have read, reviewed, and approved the article.