Short-Term Risk Factors for Distal Junctional Kyphosis after Spinal Reconstruction Surgery in Patients with Osteoporotic Vertebrae
Article information
Abstract
Study Design
Level 3 retrospective cohort case-control study.
Purpose
This study aimed to investigate the risk factors for distal junctional kyphosis (DJK) caused by osteoporotic vertebral fractures following spinal reconstruction surgery, with a focus on the sagittal stable vertebra.
Overview of Literature
Despite the rarity of reports on DJK in this setting, DJK was reported to reduce when the lower instrumented vertebra (LIV) was extended to the sagittal stable vertebra in the posterior corrective fixation for Scheuermann’s disease.
Methods
This study included 46 patients who underwent spinal reconstruction surgery for thoracolumbar osteoporotic vertebral fractures and kyphosis and were followed up for 1 year postoperatively. DJK was defined as an advanced kyphosis angle >10° between the LIV and one lower vertebra. The patients were divided into groups with and without DJK. The risk factors of the two groups, such as patient background, surgery-related factors, radiographic parameters, and clinical outcomes, were analyzed.
Results
The DJK and non-DJK groups included 14 and 32 patients, respectively, without significant differences in patient background. Those with instability in the distal adjacent LIV disc had a significantly higher risk of DJK occurrence (28.6% vs. 3.2%, p=0.027). DJK occurrence significantly increased in those with the sagittal stable vertebra not included in the fixation range (57.1% vs. 18.8%, p=0.020). Other preoperative radiographic parameters were not significantly different. Instability in the distal adjacent LIV disc (adjusted odds ratio, 14.50; p=0.029) and the exclusion of the sagittal stable vertebra from the fixation range (adjusted odds ratio, 5.29; p=0.020) were significant risk factors for DJK occurrence.
Conclusions
Regarding spinal reconstruction surgery in patients with osteoporotic vertebral fractures, instability in the distal adjacent LIV disc and the exclusion of the sagittal stable vertebra from the fixation range were risk factors for DJK occurrence in the short term.
Introduction
Studies have reported the risk factors for proximal junctional kyphosis (PJK) as a complication of corrective spinal fusion in osteoporotic vertebral fractures (OVFs) [1–3]. According to Du et al. [1], the risk factors for PJK included age >70 years, body mass index (BMI) >28 kg/m2, bone mineral density (BMD) <−3.5 standard deviation, preoperative pelvic incidence (PI) minus lumbar lordosis (LL) (PI–LL) >20°, and posterior ligamentous complex injury [2]. Tamai et al. [3] reported that severe osteoporosis and immobilization to the sacrum are risk factors for PJK. However, few studies have reported about distal junctional kyphosis (DJK), and many factors remain unclear. In addition, the occurrence of DJK was reported to have reduced when the lower instrumented vertebra (LIV) was extended to the sagittal stable vertebra (SSV) in the posterior corrective fixation for Scheuermann’s disease [4–6]. Therefore, we hypothesized that the SSV may be useful in kyphosis associated with thoracolumbar OVFs. Thus, this novel study aimed to investigate the risk factors for DJK in reconstructive spine surgery for kyphosis due to OVFs, focusing on the SSV.
Materials and Methods
1. Patient population
This retrospective study included patients at our institution who underwent spinal osteotomy+posterior fusion (PF) or anterior vertebral body replacement (AVBR)+PF for OVFs with kyphosis, whose primary fracture was in the thoracolumbar region. All patients provided informed consent, and the study protocol was approved by the institutional review board of Osaka City University (approval no., 3170). Seventy patients underwent three-column osteotomy (3CO)+PF or AVBR+PF for kyphosis with OVFs between April 2011 and October 2021. Of the 70 patients, 24 were excluded because their primary fractures were not in the thoracolumbar transition region, they had undergone spinal fusion surgery, or they had no postoperative whole-spine standing radiographs. Finally, the study included 46 patients with measurable whole-spine standing radiographs taken preoperatively and 1 year postoperatively.
2. Selection of the fixation range
If the surgical technique was AVBR+PF, the basic choice was 1 above 1 below or 2 above 2 below; if 3CO+PF, 2 above 2 below or longer fixation range was chosen. The surgeon’s judgment was modified according to the location of the vertebral fracture or existing vertebral fracture.
3. Surgical technique
When kyphosis causing thoracolumbar fracture could be corrected to some extent in the supine position, AVBR+PF was selected, and when kyphosis could not be corrected in the supine position, 3CO+PF, such as pedicle subtraction osteotomy (PSO) or posterior vertebral column resection (PVCR), was preferred. AVBR+PF was first performed in the lateral supine position using a transthoracic retropleural or retroperitoneal approach, and AVBR+PF was first reconstructed anteriorly with a titanium cage (X-Core2; NuVasive, San Diego, CA, USA). Then, PF was performed posteriorly in the prone position. In addition, PSOs and PVCR were performed posteriorly.
4. Assessment items
Patient background factors including age, sex, BMI, femoral BMD, and fracture level were evaluated. The surgical procedure and number of fixed vertebrae were examined as surgery-related factors. If the fracture involved more than one vertebra, the vertebra that was the main cause of kyphosis deformity was determined. Imaging evaluation included the assessment of the degree of degeneration and the instability of the distal adjacent LIV disc and the presence of SSV, DJK, PJK, and cage subsidence in each whole-spine sagittal parameter preoperatively and 1 year postoperatively. The degree of disc degeneration was evaluated using the Pfirrmann classification [7], with grades 1–3 representing no disc degeneration and 4–5 representing disc degeneration [8]. Intervertebral instability was defined as degenerative spondylolisthesis (DS) with Meyerding grade 2 or DS with Meyerding grade 1 but segmental kyphosis of ≥5°, or displacement of ≥3 mm in forward or backward bending [9]. PJK was defined as an advanced kyphosis angle of ≥10° between the upper instrumented vertebra (UIV) and one superior vertebra [10], whereas DJK was defined as an advanced kyphosis angle of ≥10° between the LIV and one inferior vertebra [11].
Whole-spine sagittal parameters included the sagittal vertical axis, thoracic kyphosis (TK), LL, pelvic tilt, sacral slope, PI, and T1 pelvic angle. Two spinal surgeons evaluated each image. The clinical outcomes included preoperative and 1-year postoperative low back pain Visual Analog Scale (VAS) and Japanese Orthopedic Association (JOA) scores. In patients who underwent reoperation for DJK, PJK, or cage subsidence during the 1-year postoperative follow-up, the outcomes immediately before reoperation were evaluated as the outcomes at the last follow-up.
5. Statistical analysis
To examine the risk factors for DJK in patients with OVFs who underwent spinal reconstruction surgery for kyphosis, patients were divided into the DJK and non-DJK groups based on the radiographic data collected 1 year postoperatively. For both groups, univariate analysis was performed on patient-related, surgery-related, pre- and postoperative radiographic, and pre- and postoperative clinical data. To assess normality, the Mann-Whitney U test was used for nonparametric items, whereas Student t-test was used for parametric items. When comparing clinical outcomes, an analysis of covariance was used to adjust for covariates that included each preoperative outcome.
Subsequently, multivariate logistic regression analysis was employed, which included variables with p<0.05 in the previous analysis as explanatory variables, adjusting for age. As a subanalysis, the low back pain VAS and JOA scores taken 1 year postoperatively were compared between the DJK and non-DJK groups, excluding the PJK and cage-sinking cases, using the analysis of covariance. All statistical analyses were performed using the EZR graphical user interface (Saitama Medical Center, Jichi Medical University, Saitama, Japan).
Results
1. Main results
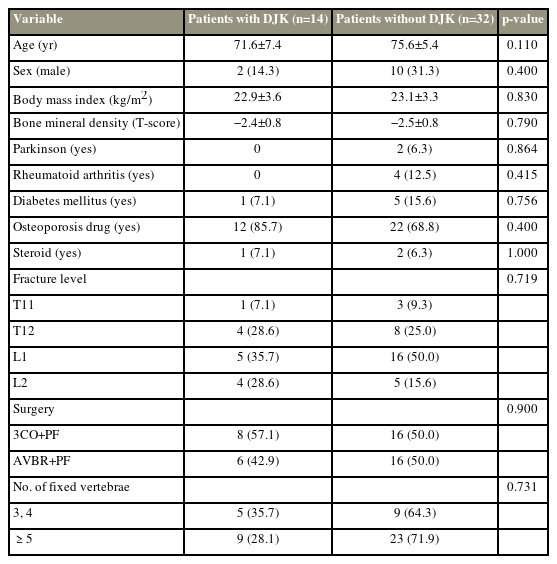
The demographic data of the patients are shown in Table 1. The mean patient age was 74±7.2 years (range, 52–86 years). This study included 12 men and 34 women. The fracture level was T11 in four cases, T12 in 12, L1 in 21, and L2 in nine. Surgery was performed with 3CO+PF in 24 of the 46 patients and AVBR+PF in 22 patients. The number of fixed vertebrae was 2 in 11 cases, 3–4 in 20 cases, and ≥5 vertebrae in 15 cases. The degeneration of the distal adjacent LIV disc was present in 22 of 46 patients (48.9%) and instability in five of 46 patients (11.1%). Of the 46 patients (30.4%), 14 had DJK, 16 (34.8%) had PJK cases, and 16 (34.8%) were cage-sinking cases.
Table 2 shows the demographic data of the two groups. No significant differences in age, sex, BMI, BMD, comorbidities, use of osteoporosis drugs, intake of steroids, or surgery type were found between the two groups.
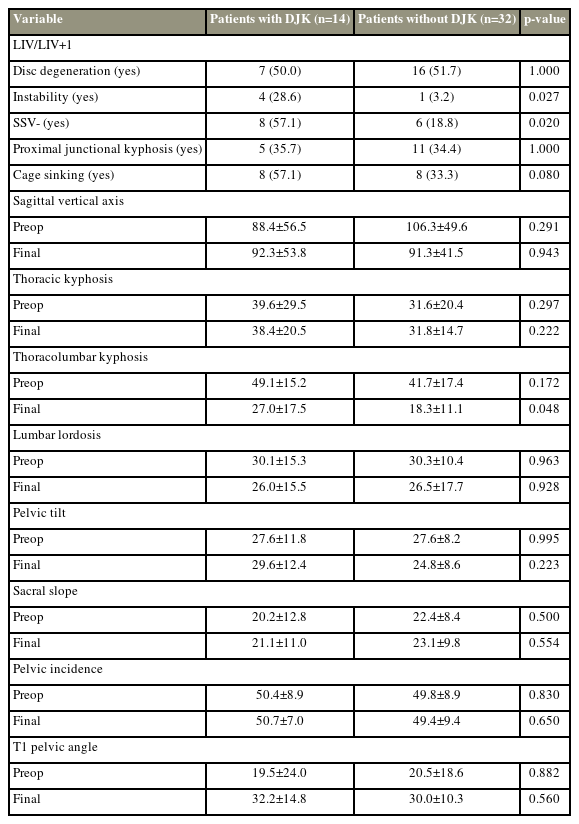
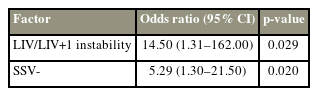
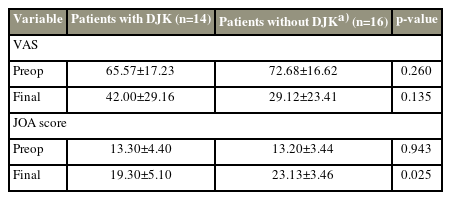
When comparing the radiographic data (Table 3), those with instability in the distal adjacent LIV disc were significantly more likely to experience DJK (28.6% versus 3.2%, p=0.027), and those that excluded the SSV in the fixation range had a significantly higher incidence of DJK (57.1% versus 18.8%, p=0.02). No significant differences were found for other preoperative radiographic parameters, including whole-spine sagittal parameters. The multivariate logistic regression analysis adjusted for age (Table 4) revealed that instability in the distal adjacent LIV disc (adjusted odds ratio, 14.50; p=0.027) and exclusion of SSV in the fixation range (adjusted odds ratio, 5.29; p=0.020) were significant factors for DJK development. In patients with and without DJK with relatively short fixation ranges, such as three- or four-fixed vertebrae, the exclusion of the SSV in the fixation range (20.0% versus 0.0%, p=0.357) and the instability in the distal adjacent LIV disc (0.0% versus 0.0%, p=1.000) were not identified as significant risk factors, whereas in those with relatively long fixation ranges, such as ≥5 fixed vertebrae, the exclusion of the SSV in the fixation range (77.8% versus 26.1%, p=0.015) and the instability in the distal adjacent LIV disc (44.4% versus 4.5%, p=0.017) were significant risk factors. The comparison of clinical outcomes between the DJK and non-DJK group excluding PJK and cage-sinking cases is shown in Table 5. The JOA score assessed 1 year postoperatively was significantly lower in the DJK group than in non-DJK group, excluding PJK and cage-sinking cases (DJK group: 19.3 points versus non-DJK group: 23.1 points; p=0.03).
2. Case discussion
1) Case 1
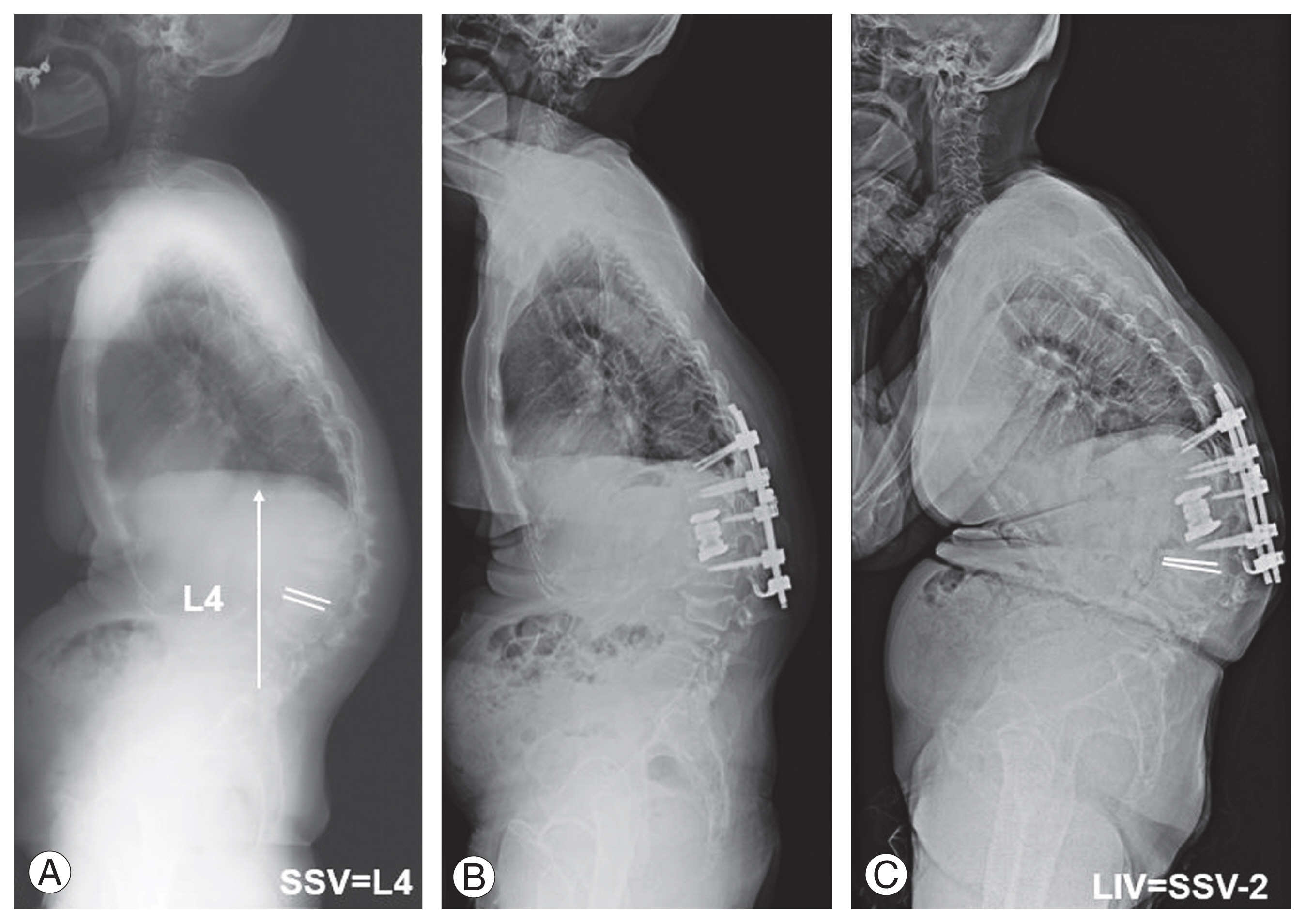
An 82-year-old woman underwent L1 vertebral column resection (VCR)+T11–L3PF for a kyphotic deformity after an L1 vertebral fracture (Fig. 1). The preoperative SSV was L4, and the SSV was excluded from the fixation range. In the 1-year postoperative radiograph, DJK occurred.

(A) Case 1: an 82-year-old woman with back pain and kyphosis due to an L1 vertebral fracture. The preoperative sagittal stable vertebrae (SSV) is L4. (B) The patient underwent L1PVCR+T11-L3PF. The SSV is excluded from the fixation range. (C) The 1-year postoperative X-ray shows distal junctional kyphosis. PVCR, posterior vertebral column resection; PF, posterior fusion.
2) Case 2
A 70-year-old woman underwent T12VCR+T10–L2PF for kyphotic deformity after a T12 vertebral fracture (Fig. 2). The preoperative SSV was L2 and was included in the fixation range. The 1-year postoperative radiograph did not reveal DJK.

(A) Case 2: a 70-year-old woman with back pain and kyphosis due to a T12 vertebral fracture. The preoperative sagittal stable vertebrae (SSV) is L2. (B) The patient underwent T12PVCR+T10-L2PF. The preoperative SSV L2 is included in the fixation range. (C) The 1-year postoperative X-ray reveals no distal junctional kyphosis. PVCR, posterior vertebral column resection; PF, posterior fusion.
3) Case 3
Another 70-year-old woman underwent L1 AVBR+T11–L2PF for kyphosis deformity after an L1 vertebral fracture (Fig. 3). The preoperative SSV was L4, which was excluded from the fixation range. The 1-year postoperative radiograph revealed DJK.
(A) Case 3: a 70-year-old woman with back pain and kyphosis due to an L1 vertebral fracture. The preoperative sagittal stable vertebrae (SSV) is L4. (B) The patient underwent L1AVBR+T11-L2PF. The SSV is not included in the fixation range. (C) The 1-year postoperative X-ray shows distal junctional kyphosis. AVBR, anterior vertebral body resection; PF, posterior fusion.
Discussion
This study showed that the exclusion of the SSV in the fixation range was a significant risk factor for DJK 1 year after spinal reconstruction surgery in patients with OVFs.
In older people, the selection of the fixation range for kyphosis deformity following OVFs is difficult because of varied opinions [12–15]. A study recommended fixing the UIV beyond the apical vertebra of the TK to avoid adjacent vertebral fractures immediately after surgery [2]. If the LIV is a lower lumbar vertebra, fractures may occur between the LIV and the sacral vertebra. In addition, PJK had several known risk factors. However, many uncertainties exist regarding DJK.
After long-range fixation, the distal moment arm is longer than the proximal moment arm; therefore, problems at the distal junction cause more imbalances in the sagittal plane than those in the proximal junction [16]. Although DJK has lower incidence than PJK, the rate of additional surgery was reported as higher than that of PJK [4,5,17]. Regarding clinical outcomes, Hasegawa et al. [12] reported a significantly lower 2-year postoperative Oswestry Disability Index in the DJK group than in the non-DJK group. Our results indicate a significant difference in the JOA score measured 1 year postoperatively in the DJK group compared with that in the non-DJK group, excluding PJK and cage-sinking cases; however, no significant difference was found in VAS scores assessed 1 year postoperatively because of the small number of cases.
Although DJK has multifactorial causes [18], which vary among diseases, the presence of a fixation moment in the distal junctional segment that exceeds mechanical resistance is a common factor [19]. Briefly, mechanical problems are the main risk factors in DJK, and the SSV is gradually becoming useful in reducing postoperative distal junctional mechanical problems in Scheuermann’s kyphosis [6,20].
Moreover, we hypothesized that the SSV is useful in kyphosis associated with thoracolumbar OVFs and demonstrated that the inclusion of the SSV in the fixation range reduces the incidence of DJK. Regarding other LIV treatment strategies, the distal junctional segment selected should be free of substantial degeneration and kyphosis or instability [19]. In the present study, the instability of the distal adjacent LIV disc was also a risk factor for DJK occurrence and must be determined. The LIV should be determined based on a composite judgment of various factors.
Increasing the fixation force at the LIV can also reduce implant-related failures [21]. In some cases, such as in case 3, the screw was not cut out because a hook was used at the LIV. Therefore, DJK did not occur. Fortunately, the clinical follow-up of this case revealed that the VAS score improved from 60 to 16 points, and the JOA score improved from 12 to 23 points when compared 1 year postoperatively.
The fixation of the PS with bone cement may also be useful in patients with osteoporosis. Biomechanical studies have confirmed that cemented PS exhibits greater load-bearing capacity against pullout axial forces [22,23]. They are also useful for clinical and radiological improvements in patients with osteoporosis requiring spinal instrumentation [24,25].
This study had some limitations. First, the number of DJK cases was small; thus, the risk factors for DJK were not adequately identified. Second, this is a retrospective study. Third, the follow-up period was relatively short (1 year), which was attributed to the small number of cases. More studies with longer follow-up periods and larger sample sizes are needed to validate the final results. However, the average time to DJK occurrence in this study was 3.77±2.31 months, suggesting that a 1-year postoperative follow-up may be useful to detect DJK caused by the instability of the distal adjacent LIV disc and excluding the SSV from the fixation range, which was a risk factor for DJK. In addition, DJK may have been newly caused by different factors in the long-term follow-up. Fourth, the reported risk factors of PJK (e.g., disc degeneration [26] and posterior ligamentous complex damage [1]) were not investigated. Finally, the strategy for the extent of spinal reconstruction fixation for kyphosis deformity in thoracolumbar OVFs is inconsistent because it depends on the vertebral fracture site and presence of other nearby vertebral fractures. Risk factors for DJK were further examined for different fixation ranges because the fixation range was not the same (Table 6). In the DJK and non-DJK groups with relatively long fixation ranges, such as ≥5 fixed vertebrae, the exclusion of the SSV in the fixation range and the instability in the distal adjacent LIV disc were identified as significant risk factors but not for those with relatively short fixation ranges, such as three- or four-fixed vertebrae. Therefore, the difference in the mechanism of DJK occurrence was considered, and DJK causes were classified into LIV, such as LIV screw loosening and LIV fractures, and distal adjacent LIV disc, and statistically examined. Although no significant difference was noted between the two groups (p=0.091), those with relatively short fixation ranges, such as three- or four-fixed vertebrae, tended to be caused by the LIV (80.0%), whereas those with relatively long fixation ranges, such as ≥5 fixed vertebrae tended to be caused by the distal adjacent LIV disc (77.8%). During DJK, relatively short- and long-fixation ranges may result in the mechanical loading of the LIV and distal adjacent LIV disc, respectively.
Conclusions
In this study, the incidence of DJK for kyphotic deformity in OVFs was 30.4%, suggesting that DJK may affect the postoperative JOA score. In the spinal reconstruction surgery for patients with OVFs, instability in the distal adjacent LIV disc and the exclusion of the SSV in the fixation range were the risk factors for DJK development in the short term.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conception and design, data acquisition, and drafting of the manuscript: Sawada Y, Takahashi S; analysis of data: Sawada Y; and critical revision and supervision: Terai H, Kato M. Toyoda H, Suzuki A, Tamai K, Yabu A, Iwamae M, Nakamura H. All authors read and approved the final manuscript.