 |
 |
- Search
| Asian Spine J > Volume 18(1); 2024 > Article |
|
Abstract
Purpose
Overview of Literature
Methods
Results
Acknowledgments
Notes
Author Contributions
GW and PL did the data collection and wrote the article. YL and CZ finished the measurement and analysis. JS did the critical revision. All authors read and approved the final manuscript.
Funding
This article receives funding from the Natural Science Foundation of Shandong Province (Award No., ZR2020QH264), Clinical Medical Science and Technology Innovation Plan of Jinan (Award No., 202019202), Shanghai Natural Science Foundation (No., 21ZR1459500), Municipal Commission of Health and Family Planning Foundation of Shanghai (No., 202140413), Medical Health Science and Technology Innovation Plan of Jinan (No., 202019182), science and technology innovation project of Medical staff in Shandong Province, and Natural Science Foundation of Shandong Province (No., ZR2020QH264).
Fig. 1

Fig. 2

Fig. 3
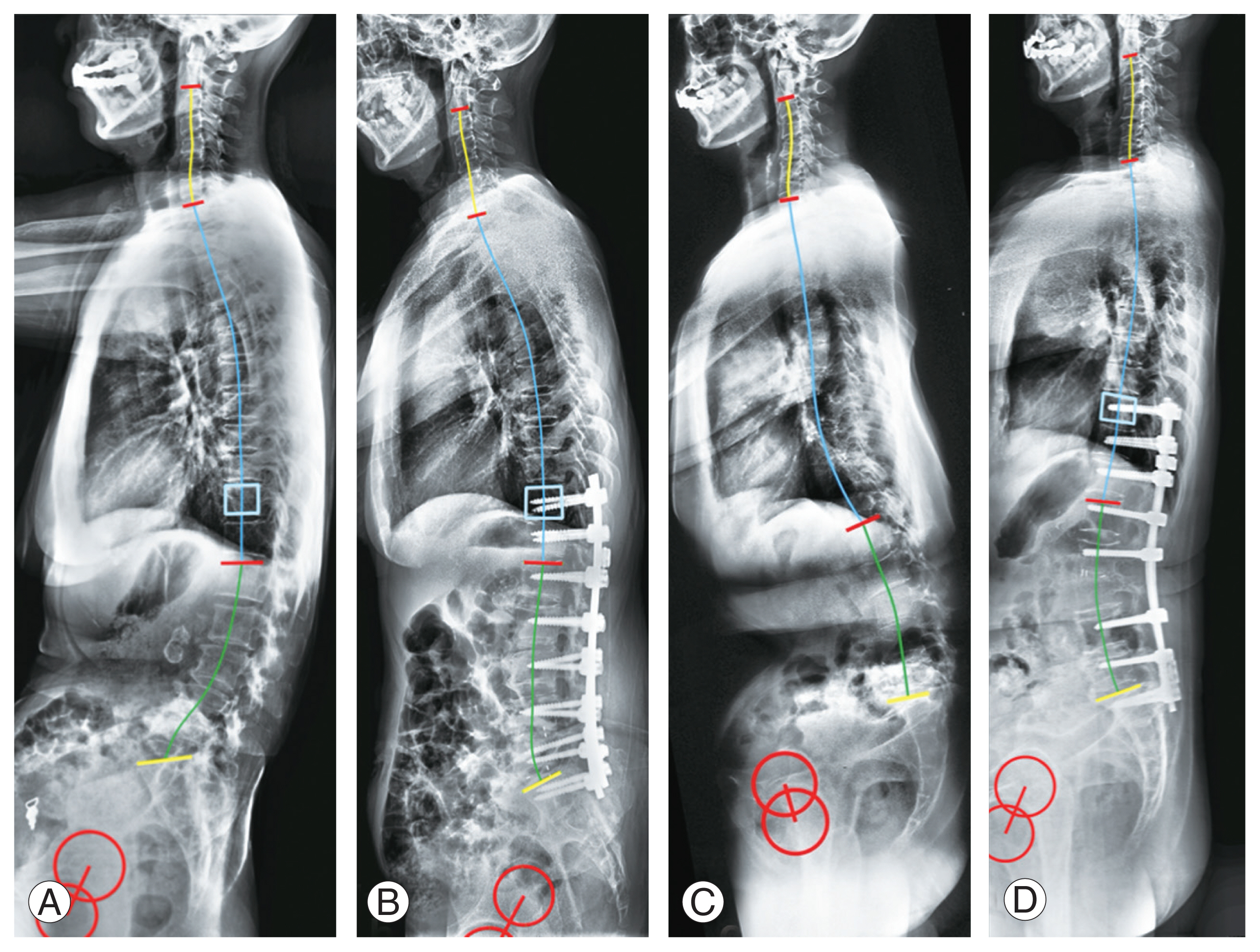
Table 1
| Variable | Group 1 | Group 2 | p-value |
|---|---|---|---|
| ES muscularity | 0.79±0.24 | 0.49±0.17 | 0.001* |
| MF muscularity | 0.24±0.06 | 0.17±0.07 | 0.004* |
| ES FIA | 0.32±0.21 | 0.51±0.29 | 0.090 |
| MF FIA | 0.41±0.25 | 0.58±0.26 | 0.127 |
| SVA (mm) | −2.4±31.4 | 112.6±15.9 | <0.001* |
| PI–LL (°) | 34.7±6.0 | 46.4±7.1 | 0.012* |
| TPA (°) | 23.3±6.6 | 35.6±11.6 | 0.001* |
| PI (°) | 45.8±15.0 | 49.2±11.8 | 0.471 |
| PT (°) | 31.2±6.3 | 34.6±12.9 | 0.351 |
| SS (°) | 14.4±11.7 | 14.7±11.0 | 0.942 |
| LL (°) | −11.6±19.5 | −2.8±15.7 | 0.158 |
| PLL (°) | 11.4±24.6 | 7.8±17.9 | 0.650 |
| DLL (°) | −26.4±15.4 | −12.3±14.1 | 0.015* |
| TLK (°) | 10.2±23.2 | 2.4±13.7 | 0.234 |
| TK (°) | 7.3±12.8 | 7.4±14.3 | 0.987 |
| PJK rate | 7 out of 21 | 10 out of 19 | 0.177 |
| ODI | 57.5±7.9 | 60.2±10.3 | 0.763 |
Values are presented as mean±standard deviation. Statistically significant results are marked in bold.
ES, erector spinae; MF, multifidus; Muscularity, ratio of cross-sectional area of muscle-vertebrae body; FIA, fatty infiltration area; SVA, sagittal vertical axis; PI–LL, pelvic incidence-lumbar lordosis mismatch; TPA, T1-pelvic angle; PI, pelvic incidence; PT, pelvic tilt; SS, sacrum slope; LL, lumbar lordosis; PLL, proximal lumbar lordosis; DLL, distal proximal lumbar lordosis; TLK, thoracolumbar kyphosis; TK, thoracic kyphosis; PJK, proximal junctional kyphosis.
Table 2
Table 3
| Variable | Multivariable regression analysis | |
|---|---|---|
| OR (95% CI) | p-value | |
| ES muscularity | 0.001 (0.000–0.600) | 0.039* |
| MF muscularity | 0.002 (0.000–153.2) | 0.368 |
| ES FIA | 0.166 (0.002–11.56) | 0.407 |
| MF FIA | 0.100 (0.001–9.731) | 0.324 |
| SVA | 1.034 (1.000–1.069) | 0.048* |
| PI–LL | 1.068 (0.997–1.144) | 0.059 |
| TPA | 1.098 (0.993–1.214) | 0.069 |
| PI | 1.045 (0.965–1.133) | 0.280 |
| PT | 1.053 (0.974–1.139) | 0.193 |
| SS | 0.978 (0.879–1.089) | 0.684 |
| LL | 1.049 (0.980–1.124) | 0.170 |
| PLL | 0.997 (0.940–1.058) | 0.928 |
| DLL | 1.083 (0.994–1.179) | 0.068 |
| TLK | 0.988 (0.941–1.037) | 0.633 |
| TK | 0.994 (0.929–1.064) | 0.873 |
OR, odds ratio; CI, confidence interval; ES, erector spinae; MF, multifidus; Muscularity, ratio of cross-sectional area of muscle-vertebrae body; FIA, fatty infiltration area; SVA, sagittal vertical axis; PI–LL, pelvic incidence-lumbar lordosis mismatch; TPA, T1-pelvic angle; PI, pelvic incidence; PT, pelvic tilt; SS, sacrum slope; LL, lumbar lordosis; PLL, proximal lumbar lordosis; DLL, distal proximal lumbar lordosis; TLK, thoracolumbar kyphosis; TK, thoracic kyphosis.
References
- TOOLS







