Adolescent Idiopathic Scoliosis: Is the Feasible Option of Minimally Invasive Surgery using Posterior Approach?
Article information
Abstract
The purpose of this systematic review and meta-analysis is to perform a systematic review and meta-analysis of previous studies on minimally invasive scoliosis surgery (MISS) in adolescents with idiopathic scoliosis (AIS). Some data on MISS in AIS compared with conventional open scoliosis surgery (COSS) are conflicting. A systematic literature search was conducted in Medline, Embase, and Cochrane Library, including studies reporting outcomes for MISS in AIS. The meta-analysis compared the operative, radiological, and clinical outcomes and complications between MISS and COSS in patients with AIS. Of the 208 records identified, 15 nonrandomized studies with 1,369 patients (reviews and case reports are excluded) were included in this systematic review and meta-analysis. The mean scale was 6.1, and eight of the 15 included studies showed satisfactory quality using the Newcastle-Ottawa scale. For operative outcomes, MISS had significant benefits in terms of estimated blood loss (standard mean difference [SMD], −1.87; 95% confidence interval [CI], −2.94 to −0.91) and hospitalization days (SMD, −2.99; 95% CI, −4.45 to −1.53) compared with COSS. However, COSS showed significantly favorable outcomes for operative times (SMD, 1.71; 95% CI, 0.92–2.51). No significant differences were observed in radiological outcomes, including Cobb’s angle of the main curve and thoracic kyphosis. For clinical outcomes, MISS showed significant benefits on the visual analog scale score (SMD, −0.91; 95% CI, −1.36 to −0.47). The overall complication rates of MISS were similar to those of COSS (SMD, 0.96; 95% CI, 0.61–1.52). MISS using the posterior approach provides equivalent radiological and clinical outcomes and complication rates compared with COSS. Considering the lower estimated blood loss, shorter hospitalization days, and longer operative times in MISS, COSS is still the mainstay of surgical treatment in AIS; however, MISS using the posterior approach is also one of the surgical options of choice in the case of moderate AIS.
Introduction
Minimally invasive surgery (MIS) in the spine field has become a widely employed practice in degenerative spine disorders, with approaches ranging from discectomy and fusion to deformity correction [1,2]. The advantages of MIS compared with conventional open surgery include smaller incisions, less blood loss, and musculoligamentous sparing, which contribute to lower complication rates [3]. Owing to its distinct characteristics, MIS has been explored for treating various diseases, including adolescent idiopathic scoliosis (AIS) [3,4].
Regarding its biomechanics, AIS is generally recognized as a three-dimensional deformity. Thus, the surgical goal of AIS is to correct the scoliotic (i.e., coronal deformity) and sagittal deformity [5]. To restore coronal and sagittal balance, pedicle screw instrumentation (PSI) with rod derotation (RD) using the posterior approach is a standard surgical treatment in AIS [6]. Despite the rapid evolution of MIS, attempts to perform MIS in AIS have been challenging because it requires correction of a much larger curve, longer instrumentation, and specific surgical techniques, such as RD and direct vertebral rotation (DVR) [7].
In AIS, conventional open scoliosis surgery (COSS) by the posterior approach has been proven effective in achieving powerful fixation using PSI and three-dimensional deformity correction using RD and DVR [6]. However, COSS has the drawback of a significantly long surgical incision, which leads to postoperative dissatisfaction among adolescents [5,7,8]. Consequently, the demand for MIS using posterior approaches has increased. In 2008, Sarwahi et al. [7] first introduced the MIS technique for patients with moderate AIS using three skin incisions of approximately 2 inches (5.08 cm). MISS in AIS has been performed by many skilled surgeons [9–23]. Particularly, the coin-hole technique reported by Yang et al. [14] has been introduced to overcome wound-related problems from MISS using the posterior approach. However, outcomes for surgical treatment of AIS using the posterior approach between COSS and MISS are conflicting [9–23]. Given the paucity and conflicting data, this systematic review and meta-analysis assessed the operative, radiological, and clinical outcomes, including the complication rates, between MISS and COSS using the posterior approach in moderate AIS.
Materials and Methods
The protocol for this systematic review and meta-analysis was registered in advance with the International Prospective Register of Systematic Reviews (PROSPERO; CRD42023430522). This systematic review and meta-analysis was performed and reported according to the Meta-analysis of Observational Studies in Epidemiology and the Preferred Reporting Items for Systematic Reviews and Meta-analyses checklists. The protocol for this review was not published [24,25].
1. Search strategy and selection criteria
Various databases, including PubMed/Medline, Embase, and the Cochrane Library, were searched on May 27, 2023, for MISS studies comparing COSS in AIS. The search syntax was as follows: (“idiopathic”[All Fields] OR “idiopathically”[All Fields] OR “idiopathics”[All Fields]) AND (“scoliosis”[MeSH Terms] OR “scoliosis”[All Fields] OR “scolioses”[All Fields]) AND (“minimal*”[All Fields]) AND (“invasibility”[All Fields] OR “invasible”[All Fields] OR “invasion”[All Fields] OR “invasions”[All Fields] OR “invasive”[All Fields] OR “invasively”[All Fields] OR “invasiveness”[All Fields] OR “invasives”[All Fields] OR “invasivity”[All Fields])) in PubMed/Medline, “idiopathic” AND (“scoliosis”/exp OR “scoliosis”) AND “minimal*” AND “invasive” in Embase, and (“idiopathic scoliosis”) AND (“minimal* invasive”) in Cochrane Library using Medical Subject Headings (MeSH) terms to identify studies published in English.
After removing duplicate articles in Endnote, two reviewers independently screened the extracted studies for eligibility based on the titles and abstracts using Covidence (Melbourne, VIC, Australia). After title and abstract screening, the same two reviewers independently reviewed full-text articles; any disagreements on the eligibility of full-text articles were resolved by consensus or discussion with a third reviewer. Studies that reported MISS in moderate AIS, including randomized controlled trials, cross-sectional studies, and cohort studies (retrospective or prospective studies), were included in this review. Moderate AIS was defined as the major curve’s Cobb angle <70° or 80°, and flexibility >50% on side-bending films in patients with AIS. Case reports, reviews, language other than English, non-availability of full-text articles, nonfusion surgery, MISS using anterior approaches, and revision surgery of MISS were excluded. The outcomes of interest of MISS in comparison with those of COSS were operative (estimated blood loss, operative time, and hospitalization days), radiological (Cobb’s angle of the main curve and thoracic kyphosis), and clinical (Scoliosis Research Society [SRS]-22r score, and Visual Analog Scale [VAS] for surgical site pain) outcomes, as well as complications (overall, surgical site infection [SSI], implant failure, and pedicle screw misplacement).
2. Data extraction
The same four reviewers, working in pairs, independently extracted the data using a predefined data extraction file. Two reviewers independently performed the risk-of-bias assessment and extracted the study data. The following baseline characteristics were extracted from the included studies: first author, year of publication, study design, period, country in which the study was performed, setting, number of included patients, mean age, sex, mean follow-up duration, MIS indication for patients with AIS, and MIS techniques.
3. Quality assessment
The same two reviewers independently assessed the quality of the nonrandomized studies using the Newcastle-Ottawa Scale in the meta-analysis [26]. Any discrepancy was resolved by the two authors after discussion. Publication bias was assessed using funnel plots.
4. Statistical analysis
Continuous variables were extracted as the mean±standard deviation by converting the values for the extracted data using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions, if sufficient information was available [27]. They were presented as standardized mean differences (SMDs) with a 95% confidence interval (CI) using the inverse variance weighting method. Dichotomous variables were extracted as absolute numbers and/or percentages, pooled using the Mantel-Haenszel method, and presented as odds ratios (ORs) with a 95% CI. The random-effects model was used for all analyses, and statistical heterogeneity between studies was assessed by visual inspection of forest plots and I2 and χ2 statistics for heterogeneity. For the subgroup assessment, the difference in effect estimates between the two subgroups was assessed as described in the Cochrane Handbook for Systematic Reviews of Interventions [27]. The significance level across the subgroups was determined by testing for subgroup differences. We also assessed potential publication bias by visual inspection of funnel plots of risk ratios and standard errors. Statistical analyses were performed using RevMan Web (Cochrane, London, UK) or the Meta package in R ver. 4.3.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
1. Search
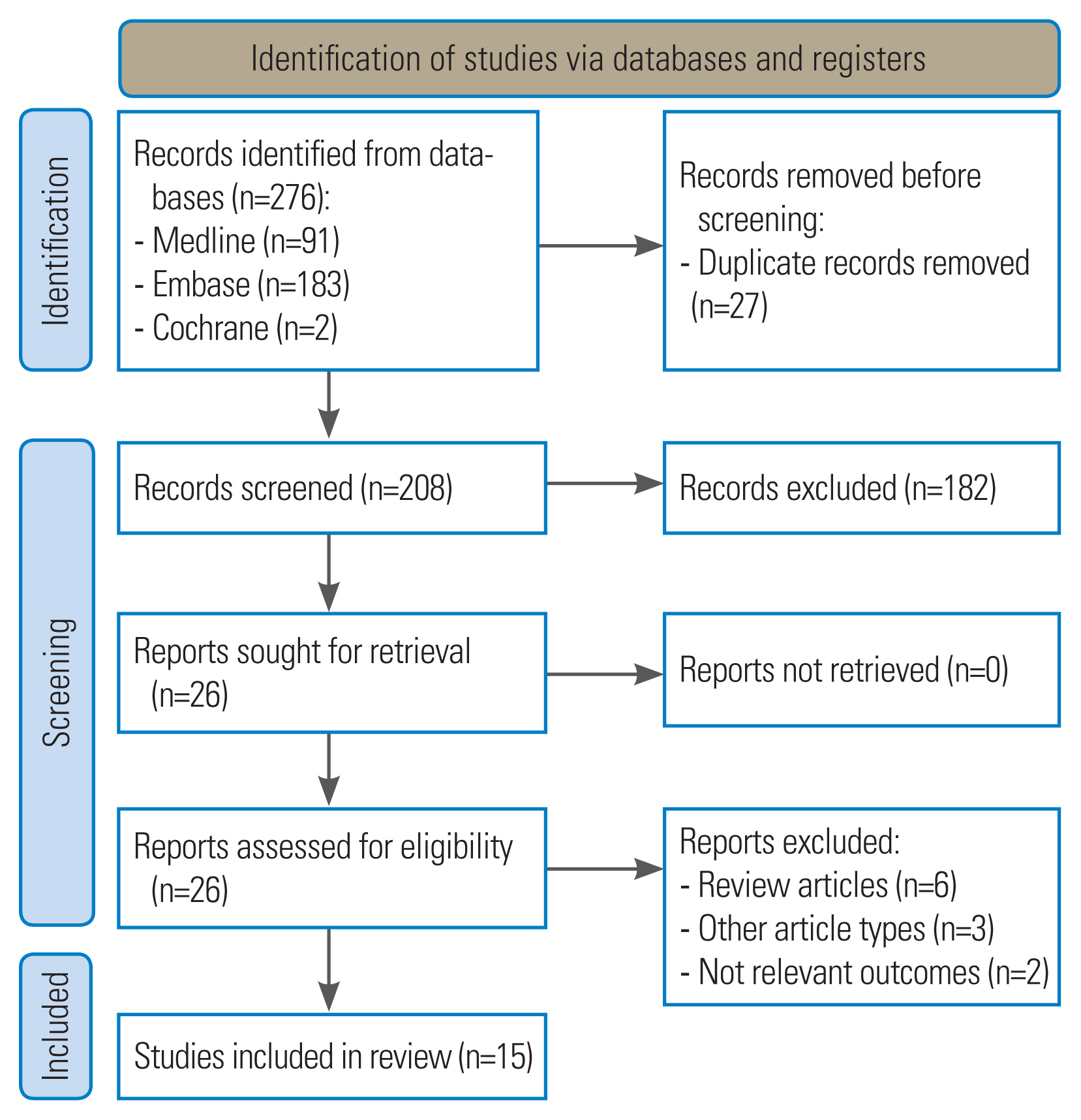
After screening 208 articles from the title and abstracts, 26 articles were identified in the reports for eligibility. After reviewing the full-text articles, 11 articles were excluded as follows: review articles (n=6), other article types such as case reports and letters (n=3), and studies including nonrelevant outcomes of MISS and COSS (n=2). Finally, 15 nonrandomized studies were included in this systematic review and meta-analysis (Fig. 1).
2. Baseline study characteristics
A total of 15 nonrandomized studies with 1,369 patients—of whom 805 were treated with MISS and 564 with COSS—were included. Five of the included studies only assessed the outcome of MISS and included COSS information. The baseline study characteristics of the included studies are summarized in Table 1.
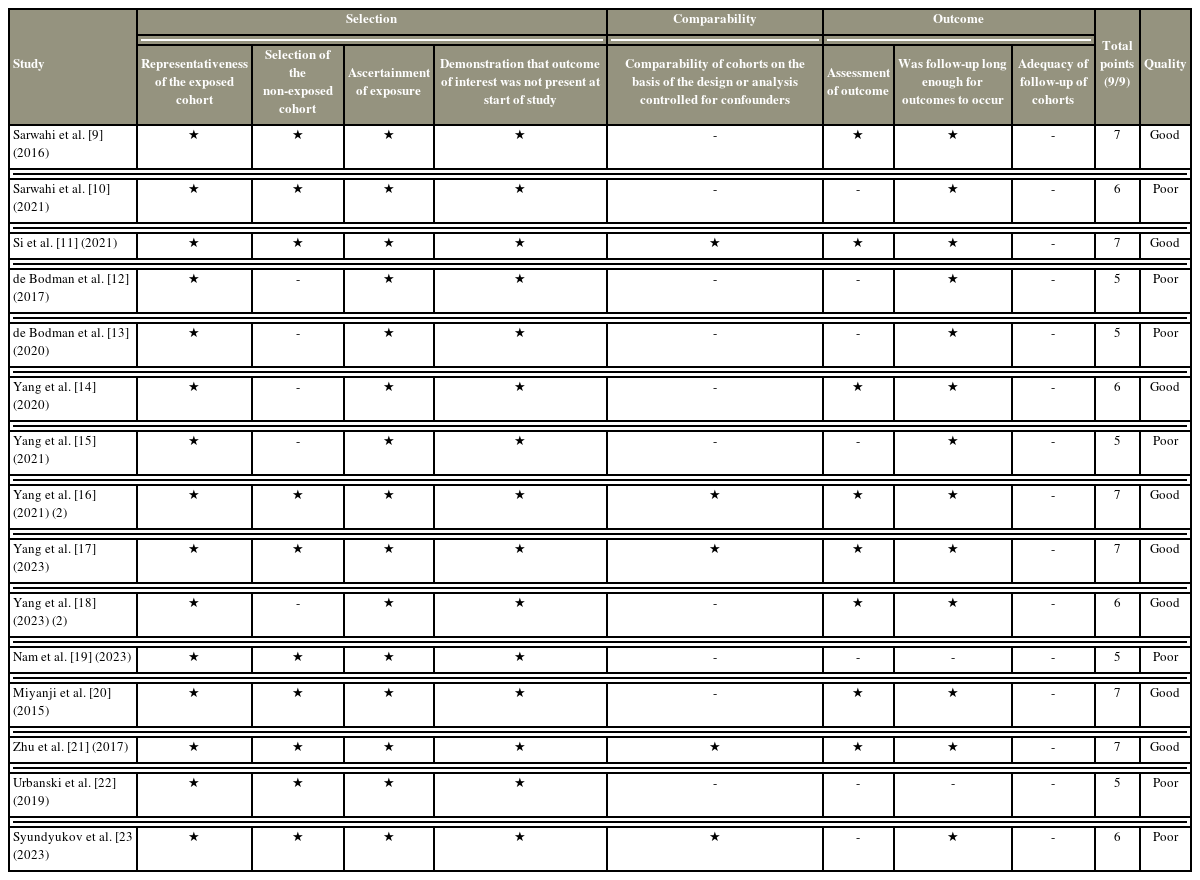
3. Quality assessment
All 15 included studies were non-randomized; thus, we assessed the risk of bias using the Newcastle-Ottawa Scale. The mean scale was 6.1 (range, 5–7), and eight of the 15 included studies showed satisfactory quality. The details of the quality assessment in this study are presented in Table 2.
4. Operative outcome measures
The estimated blood loss in eight studies, operative time in eight studies, and number of hospitalization days in seven studies were measured as operative outcomes. All of the measured operative parameters exhibited heterogeneity (I2=96%, estimated blood loss; I2=94%, operative time; I2=96%, hospitalization days). For the estimated blood loss, the overall pooled effect showed that MISS was associated with a significant reduction in estimated blood loss compared with COSS (SMD, −1.87; 95% CI, −2.94 to −0.91; p<0.001) (Fig. 2A). For the operative time, the overall pooled effects showed that MISS had a significantly longer operative time than COSS (SMD, 1.71; 95% CI, 0.92–2.51; p<0.001) (Fig. 2B). For hospitalization days, the overall pooled effect showed that MISS was associated with a significant reduction in hospitalization days compared with COSS (SMD, −2.99; 95% CI, −4.45 to −1.53; p<0.001) (Fig. 2C).

Comparison of operative outcome measures in this meta-analysis. (A) Estimated blood loss. (B) Operative time. (C) Hospitalization days. MISS, minimally invasive scoliosis surgery; COSS, conventional open scoliosis surgery; SD, standard deviation; SMD, standard mean difference; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
To evaluate radiological outcomes, Cobb’s angle of the main curve was measured in 10 studies and thoracic kyphosis in eight studies. Heterogeneity was observed as I2=86% in Cobb’s angle of the main curve and I2=79% in thoracic kyphosis. For Cobb’s angle of the main curve, the overall pooled effect revealed that MISS did not show significant differences in Cobb’s angle of the main curve compared with COSS (SMD, −0.3; 95% CI, −0.70 to 0.10; p=0.15) (Fig. 3A). For thoracic kyphosis, no significant differences were observed between MISS and COSS (SMD, −0.20; 95% CI, −0.59 to 0.19; p=0.31) (Fig. 3B). Cobb’s angle of the main curve was measured in >10 studies. The presented funnel plots were relatively symmetrical, indicating no evidence of publication bias (Fig. 3C).

Comparison of radiological outcome measures in this meta-analysis. (A) Cobb’s angle of the main curve. (B) Thoracic kyphosis. (C) Funnel plot for Cobb’s angle of the main curve to assess the publication bias. MISS, minimally invasive scoliosis surgery; COSS, conventional open scoliosis surgery; SD, standard deviation; SMD, standard mean difference; IV, inverse variance; CI, confidence interval; df, degrees of freedom; SE, standard error; MD, mean difference.
For the clinical outcomes, the postoperative VAS score was measured in two studies and the SRS-22r score in four studies. Heterogeneity was observed in the SRS-22r score (I2=83%); however, it was not observed in the VAS (I2=56%). For VAS, the overall pooled effect showed that MISS was associated with a significant reduction in postoperative VAS compared with COSS (SMD, −0.91; 95% CI, −1.36 to −0.47; p<0.001) (Fig. 4A). For the SRS-22r score, the overall pooled effect of the SRS-22r score showed no significant difference between MISS and COSS (SMD, 0.31; 95% CI, −0.29 to 0.91; p=0.31) (Fig. 4B).
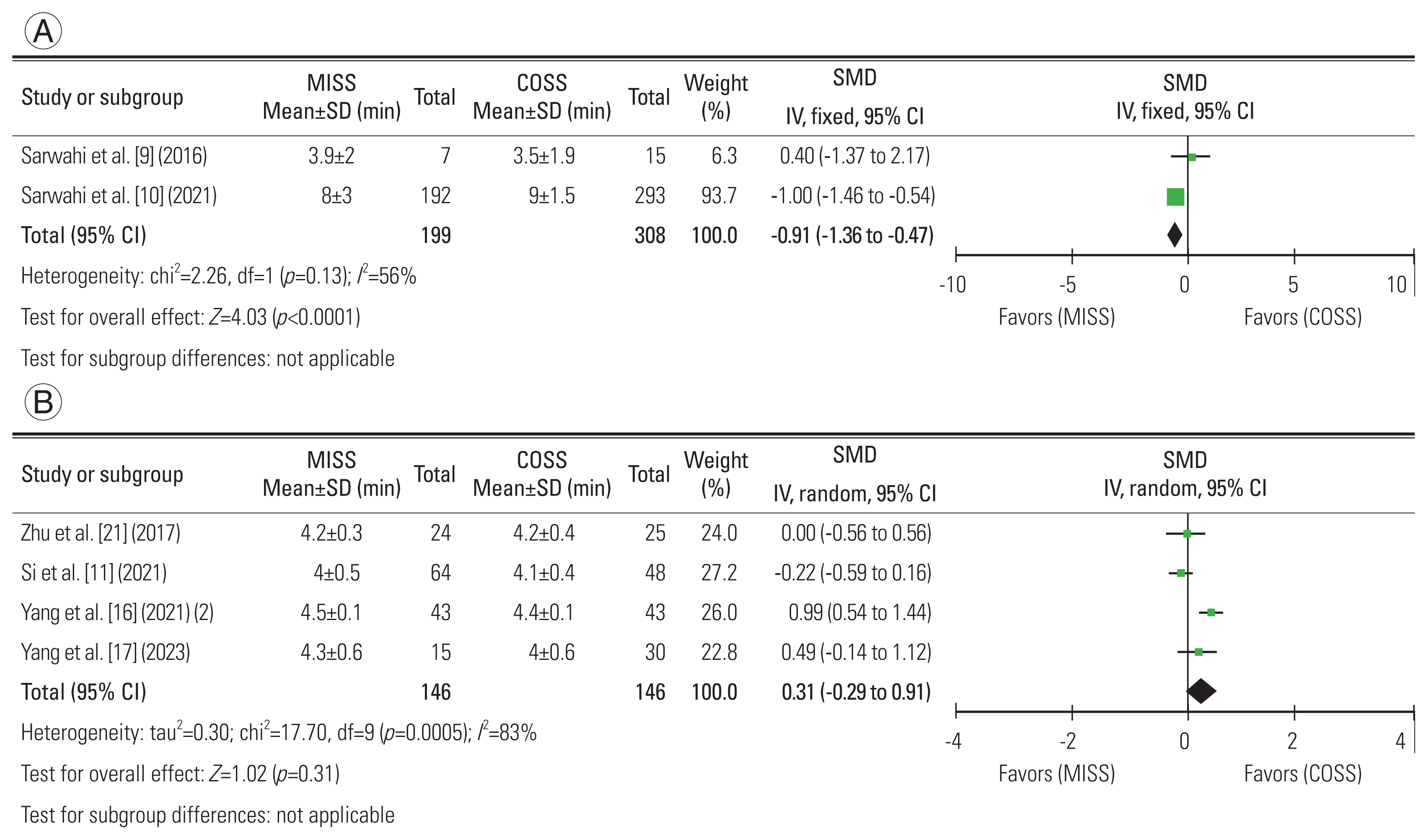
Comparison of clinical outcome measures in this meta-analysis. (A) Visual Analog Scale (VAS). (B) Scoliosis Research Society-22r (SRS-22r) score. MISS, minimally invasive scoliosis surgery; COSS, conventional open scoliosis surgery; SD, standard deviation; SMD, standard mean difference; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
The presence of overall complications, such as SSI, implant failure, and pedicle screw misplacement, were evaluated for the comparison of the complication rates between MISS and COSS. None of the data regarding the complication-related parameters had heterogeneity as an overall complication (I2=0%), SSI (I2=5%), implant failure (I2=0%), or pedicle screw misplacement (I2=0%). The overall pooled effect of overall complication (OR, 0.96; 95% CI, 0.61–1.52; p=0.87), SSI (OR, 1.63; 95% CI, 0.82–3.22; p=0.16), implant failure (OR, 1.36; 95% CI, 0.47–3.93; p=0.57), and pedicle screw misplacement (OR, 1.18; 95% CI, 0.94–1.48; p=0.15) showed no significant difference between MISS and COSS (Fig. 5).

Comparison of complication measures in this meta-analysis. (A) Overall complications. (B) Surgical site infection. (C) Implant failure. (D) Pedicle screw misplacement. MISS, minimally invasive scoliosis surgery; COSS, conventional open scoliosis surgery; SD, standard deviation; SMD, standard mean difference; M-H, Mantel-Haenszel; CI, confidence interval; df, degrees of freedom. (Continued on next page.)
Discussion
In the era of MISS in spine surgery, the demand for MISS in AIS has increased to overcome the disadvantages of COSS [14]. Since Sarwahi et al. [7] initially suggested the MISS technique in AIS, many studies on the surgical outcomes of MISS in AIS have been published [9–23]. In these studies, conflicting results have been observed, such as those for complications; however, the causes of these discrepancies have been explained from various perspectives. Considering the pooled effect estimate in outcome measures, this meta-analysis provided the advantages of MISS in moderate curves of AIS: less blood loss, fewer hospitalization days, and lower postoperative pain score with equivalent radiological correction than COSS in the surgical treatment of AIS using posterior approaches. Meanwhile, COSS is favorable with respect to the operative time. Furthermore, no differences were found in the complications between MISS and COSS. However, radiation exposure in the management of AIS is one of the problems that needs caution for adolescents, which was not considered in this study. Thus, future studies with long-term follow-up data need to be established.
MISS using the posterior approach involves distinctive procedures compared with COSS. First, two or three shorter incisions are made during MISS compared with the long longitudinal single incisions in COSS [10]. A small scar length is considered one of the factors in functional outcomes in the perioperative period [14,16]. Second, MISS for facetal fusion involved less extensive soft tissue dissection and decreased area of subperiosteal exposure, whereas COSS was performed with posterior fusion with wide bone and soft tissue exposure [9,17]. Third, Yang et al. [15] used a tubular retractor as a coin-hole technique to protect the surrounding soft tissue area of the operation field. These distinctive characteristics of MISS have resulted in less estimated blood loss and fewer hospitalization days [10,16]. However, MISS is still in its early stages; therefore, the operative time did not reflect the learning curve of MISS [3,18,28]. Yang et al. [18] suggested that MISS has a mild learning curve with 46 cases of experience. Furthermore, in our meta-analysis, Sarwahi et al. [10] in 2021 showed an SMD of 0.15 of and 95% CI of −0.03 to 0.33, which are the results from proficient and skilled experience. Thus, current data are mostly the results of MISS using the posterior approach performed by proficient surgeons for moderate AIS curves, requiring careful interpretation of our meta-analysis.
The radiological outcomes of MISS were consistently equivalent or similar to those of COSS. Our focused radiological outcome measures were Cobb’s angle of the main curve in the coronal alignment and thoracic kyphosis in the sagittal alignment. Guo et al. [29] noted that anterior column overgrowth leads to harmful effects of thoracic kyphosis, which potentially contributes to cervical alignment. Thus, thoracic hypokyphosis in sagittal alignment is a critical issue for treating AIS [30–32]. In addition, Schlösser et al. [33] suggested that the RD-only technique can lead to inappropriate correction of thoracic kyphosis instead of proper correction of the main curves, or vice versa. Therefore, MISS provided equivalent radiological outcomes in Cobb’s angle of the main curve and thoracic kyphosis compared with COSS. However, MISS using the posterior approach has a limitation for three-dimensional correction in larger and stiffer curves [14–16].
Regarding clinical outcomes between MISS and COSS, VAS was only measured in the studies by Sarwahi et al. [9,10]. In 2016, Sarwahi et al. [9] did not find significant differences in VAS between MISS and COSS; however, small-sized sample data were measured with an early stage of MISS. After 5 years, Sarwahi et al. [10] in 2021 showed the advantages of postoperative VAS in MISS with large-sized sample data. The benefit of postoperative VAS affected the management of the perioperative period; thus, it may have been associated with shorter hospital stays in MISS [10]. Contrary to the VAS findings, the SRS-22r score was not significantly different between MISS and COSS. SRS-22r was measured based on function, pain, self-image, mental health, and satisfaction. The cosmesis in SRS-22r was only part of the factor; thus, a future trial is needed to evaluate cosmesis as a new measurement tool, such as scar cosmesis assessment and a rating scale from short-term to long-term follow-up between MISS and COSS [34].
In the background of the coin-hole technique by Yang et al. [14], the initial study of the MIS technique by Sarwahi et al. [9,10] reported a higher complication rate in MISS than in COSS in terms of wound problems such as late-onset wound problems (from 1 month after the MISS to 3-year follow-up) and hypertrophic scars. By employing the 20- to 24-mm diameter tubular retractor system, adequate exposure of the surgical field has been established as a form of coin hole, which reduces skin–muscle damage during free-hand pedicle screw insertion [15]. Although the overall pooled effect of SSI showed no significant difference, the OR of SSI was higher in the MISS technique by Sarwahi et al. [9,10] (OR, 2.15 from the random-effect model) than in the method by Yang et al. [16,17,19] (OR, 1.26 from the random-effect model) between MISS and COSS in AIS. However, all results in this meta-analysis were not fully considered a learning curve, which is an important factor in assessing complication rates. Therefore, an updated meta-analysis considering the learning curve is essential [5,18,28]. The intraoperative pedicle screw misplacement rate was relatively higher in MISS than in COSS (OR, 1.18; 95% CI, 0.94–1.48; p=0.15). MISS with limited surgical vision had obstacles to the process of free-hand pedicle screw insertion [19]. Limited surgical vision in coin hole and angled lesions to insert the pedicle screw may intraoperatively lead to pedicle screw misplacement [10,19,35]. However, these results showed no significant differences, indicating an acceptable range of pedicle screw placement in MISS compared with COSS despite limited surgical vision.
Although MISS using the posterior approach is a feasible option based on our analysis, special attention is needed when making judgments based on these results. MISS provides equivalent outcomes in terms of radiological, clinical, and complication rates. Meanwhile, in operative parameters, COSS required more bleeding loss (approximately 187 mL) and longer hospitalization days (approximately 3 days) than MISS. However, COSS is favorable with respect to the operative time (approximately 1.71 hours) compared with MISS in our meta-analysis. The requirement of a longer operative time can be a factor in surgeons’ hesitation to choose MISS. Although COSS is still a mainstay of the surgical treatment of moderate AIS using the posterior approach, this meta-analysis provides the need for future research on the preferences of surgeons.
Several possible limitations in this systematic review and meta-analysis must be considered. First, the missing article regarding MISS actually existed, which could have influenced the results of the meta-analysis. Although some missing articles may have existed in other databases, the included articles were from a relatively sound evidence-based database using a highly sensitive search strategy. Second, our study contained very small sample sizes. Although MIS in AIS has been sufficiently developed, MIS research remains in the early stages; thus, these data were also included, and consistent results were observed in this meta-analysis. After more evidence is presented, the efficacy and safety should be reevaluated with an updated meta-analysis. Third, heterogeneity was observed in nearly all our meta-analysis results. This may have been caused by several factors, including differences in the MISS technique between surgeons, not considering the learning curve in the current meta-analysis, and poor methodology quality from nonrandomized studies. Fourth, the definition of parameters was slightly different, such as thoracic kyphosis from T1 to T3 or T4 to T12, which also influenced the results. Lastly, the data conversion process may have affected the results by unifying the continuous data into mean±standard deviations. In this systematic review and meta-analysis, the studies of Sarwahi et al. [7,9,10] had a large influence; however, they expressed data as medians and interquartile ranges. Based on this meta-analysis, some concerns existed regarding heterogeneity and poor evidence data from nonrandomized studies [24]. Therefore, in the research of MISS in AIS, large-sample-sized randomized controlled trials with the same standard of MISS technique are needed to support our meta-analysis results. Despite these limitations, MISS offers significant advantages: our included studies consistently demonstrated its superior estimated blood loss and lower hospitalization days, with radiological outcomes in AIS comparable to those of COSS.
Conclusions
This systematic review and meta-analysis provide comparable evidence for the efficacy and safety of MISS using the posterior approach in AIS. MISS using the posterior approach provides equivalent radiological and clinical outcomes and complication rates compared with COSS. Considering the lower estimated blood loss, shorter hospitalization days, and longer operative times in MISS, COSS is still the mainstay of surgical treatment in AIS; however, MISS using the posterior approach is also one of the surgical options of choice in moderate AIS.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
HJK and DGC conceptualized the study. HJK designed the study. HJK and DGC analyzed and interpreted the data. HJK acquired the data. HJK drafted the manuscript. LGL, JP, RC, PDT, MY, and MPK critically reviewed the work. LGL, JP, RC, PDT, MY, and MPK verified the data in the study. All authors had full access to all the data and had final responsibility for the decision to submit for publication.