Surgical Management of Unstable U-Shaped Sacral Fractures and Tile C Pelvic Ring Disruptions: Institutional Experience in Light of a Narrative Literature Review
Article information
Abstract
Unstable U-shaped sacral fractures and vertical shear Tile C pelvic ring disruptions are characterized by rare lesions occurring in patients with severe trauma. Because the initial damage-control resuscitation primarily aims to stop life-threatening bleeding, emergency treatment often includes an anterior external pelvic fixator. Delayed surgery is mandatory to allow early mobilization, reduce mortality, and improve functional outcomes. Regarding U-shaped sacral fractures, although Roy-Camille type 1 U-shaped sacral fractures can be treated with iliosacral screws, types 2 (posteriorly displaced, equivalent to AO Spine C3) and 3 (anteriorly displaced, equivalent to AO Spine C3) fractures require spinopelvic triangular fixation. Besides, proper reduction of type 2 and some type 3 sacral fractures is mandatory to prevent wound complications. In patients with neurological deficits, the need for sacral laminectomy is left at the discretion of the surgeon, given the indirect decompression already obtained with fracture reduction. Tile C pelvic disruptions with posterior ring injury located lateral to the sacral foramen can be treated with either iliosacral screws or triangular spinopelvic fixation, combined with anterior pelvic fixation. Conversely, Tile C pelvic disruptions with posterior ring injury located at, or medial, to the sacral foramen (Denis zone II or III) induce vertical lumbosacral instability and thus require spinopelvic triangular fixation with anterior pelvic osteosynthesis. Although minimally invasive techniques have been developed, open surgeries are still required for inexperienced operators and in case of major displacement. The complication rate reaches approximately 33.33% of the cases, and complications include hardware malposition, wound infection or dehiscence, hardware prominence, and sometimes hardware failure.
Introduction
Historically, patients suffering from pelvic ring injuries or complex sacrum fractures carried a life-long burden of functional and neurological disability [1,2]. Indeed, these injuries involve a peculiar biomechanical bone chain maintained by numerous muscles and ligaments and allow the weight transfer of the upper body to the lower limbs with continuous postural adaptation [3]. Hence, unstable sacral fractures and pelvic ring injuries jeopardize one’s ability to maintain a standing position or to walk with disrupted biomechanical pelvic arches and to compress the cauda equina nerve roots passing through the sacrum. Since the first surgical attempts in the early 1980s [4], a myriad of surgical techniques have been attempted to restore pelvic arches [5]. Given that the functional prognosis after unstable sacral fractures or pelvic ring injuries is closely related to proper bone alignment [6], surgical reduction and fixation should be performed as early as possible to prevent vicious malunion, which may be difficult to correct later [7–9]. Moreover, early stabilization facilitates mobilization, reduces early mortality, and improves long-term outcomes than conservative treatment [10–14]. Nevertheless, these injuries may be frequently misdiagnosed or neglected in patients with very severe trauma who are at high risk of death by exsanguination during the first 24 hours [2,6,14–16]. Besides, no consensus has been reached regarding the surgical treatment of such fractures given their rarity (1% of all fractures) [16] and technical challenges [6,17,18]. Many classifications have been proposed for these fractures, including Roy-Camille et al. [19] (1985), Tile [20] (1988), Denis et al. [1] (1988), Isler [21] (1990), Strange-Vognsen and Lebech [22] (1991), and AO Spine (2020) [18], which may be confusing at first. Considering these blurring elements, this work aims to provide typical clinical situations with surgical treatment examples to guide surgeons in the management of spinopelvic complex fractures.
Materials and Methods
1. Literature review
A scoping literature review was conducted using the Medline database (https://pubmed.ncbi.nlm.nih.gov/) to search for articles using the surgical management of U-shaped sacral fractures and Tile C pelvic ring injuries. Articles were screened using either: (1) the advanced search mode of Medline database using the following keywords: U-shaped, U-type, H-shaped, H-type, sacrum fracture, sacral fracture, Tile C, vertical shear, pelvic ring, iliac screw, iliosacral screw, iliolumbar, spinopelvic, and triangular; or (2) by looking into the reference list of relevant articles.
We retained articles regarding a new or significant surgical technique, a widely used classification, or a homogeneous cohort of patients depending on the needs of the narrative review.
2. Institutional experience
Our operative database was screened from 2020 to 2022, and three cases illustrating three precise surgical situations were retained.
Results
1. U-shaped sacral fractures
1) Pathophysiology
U-shaped sacral fractures are generally caused by high falls and then by traffic accidents [23–25]. U-type fractures occur when the sacrum, which constitutes a bone arch hinge between the spine and pelvis, cannot withstand these important deceleration forces given its oblique position associated with pelvic incidence and sacral slope, changing the course of the pelvis and lower sacrum upward or backward [3]. The H-type of sacral fractures constitutes more complete forms of U-shaped fractures passing throughout the whole sacrum [23].
The position of the upper sacral fragment relative to the lower fragment is probably caused by the patient’s body position during the impact and to the pelvic incidence and Roussouly type of his back by Roussouly and Pinheiro-Franco [3]. Hence, Roy-Camille et al. [19] in 1985 introduced a three-grade classification: (1) compression flexion fracture with the upper sacral fragment affecting the lower sacrum and flexed anteriorly (probably associated with a middle pelvic incidence); (2) posterior displacement of the inferior portion of the upper fragment, making the upper sacrum almost horizontal and pointing toward the skin (probably associated with a low pelvic incidence); (3) and anterior displacement of the upper fragment, making it almost vertical, parallel to the lower sacrum (probably associated with a high pelvic incidence) (Fig. 1). This classification was adapted by Strange-Vognsen and Lebech [22] in 1991, with grade 4 being comminuted upper sacral fragment.
2) First surgical attempts
Purser [12] in 1969 reported a partial reduction of kyphosis of a U-shaped sacral fracture after a 2-month orthopedic treatment. Then, Fardon [4] reported one of the first surgical treatment attempts for U-shaped sacral fractures, with L5 and sacral laminectomy associated with interlaminar fixation using Harrigton’s hooks. Roy-Camille et al. [19] presented a patient series of U-shaped sacral fractures, among whom 85% (11/13) attempted jumping suicide, thus coining it the “suicidal jumper’s fracture.” He supported sacral laminectomy for the visual control of sacral nerve root freedom and bone reduction and introduced surgical fixation with straight lumbosacral plates [19].
3) Iliosacral screw fixation
Nork et al. [10] in 2001 introduced percutaneous iliosacral screw fixation for U-shaped sacral fractures in patients lying supine, with pads under their backs to exaggerate lumbar spine lordosis using ligamentotaxis. Ruatti et al. [7] in 2013 modified a technique for moderately displaced U-shaped sacral fractures.
Remarkably, percutaneous iliosacral screwing can be technically difficult. Indeed, the screws may be placed suboptimally through the fracture site, resulting in poor fracture immobilization. Furthermore, a significant risk of transfixing major pelvic blood vessels or sacral nerve roots is observed [26,27]. Lastly, the variability of the sacrum anatomy and pelvic parameters can influence the usual radiographic landmarks [28]. Hence, the use of intraoperative navigation guidance may greatly support inexperienced operators [29,30].
Furthermore, Schildhauer et al. [11] in 2006 warned against the potential remaining rotational instability for unstable sacral fractures treated solely by iliosacral screws, without triangular spinopelvic fixation.
4) Lumboiliac screw fixation
Hessmann and Rommens [31] in 2002 introduced the use of lumbosacral pedicle screws for the surgical treatment of Roy-Camille type 3 U-shaped sacral fractures. Then, Schildhauer et al. [32] in 2003 reported the visionary concept of “triangular osteosynthesis” using lumboiliac fixation and iliosacral screws for unstable sacral fractures.
Mouhsine et al. [24] in 2006 presented a “modified” triangular osteosynthesis using lumboiliac fixation for vertical distraction and a complementary transverse rod connecting the two sides of instrumentation to treat horizontal instability. Lyo et al. [33] in 2008 reported modified lumboiliac fixation of type 3 U-shaped sacral fractures using two iliac screws on each side, allowing early weight bearing. Tan et al. [25] in 2012 confirmed the efficacy of “modified” triangular osteosynthesis using a transverse connector for horizontal instability. He also provided examples of long-segment spinopelvic fixation for complex sacral fractures associated with thoracolumbar junction fractures. Several studies reported triangular spinopelvic fixation for displaced U-shaped sacral fractures with similar results [34,35]. Kelly et al. [23] in 2018 confirmed that iliosacral screw fixation is preferred for type 1 U-shaped fractures and spinopelvic fixation for more displaced (type 2 or 3) U-shaped fractures.
5) Surgical technique for iliac screw placement
Schildhauer et al. [36] in 2002 described the classic entry point for iliac screws along the iliac crest, just 1 cm cephalic to the posterior superior iliac spine. He recommended recessing the iliac screw head within the iliac crest by creating a bone window with a rongeur to avoid wound issues due to prominent hardware (Fig. 2) [36]. Freehand iliac screw placement was also described [37].
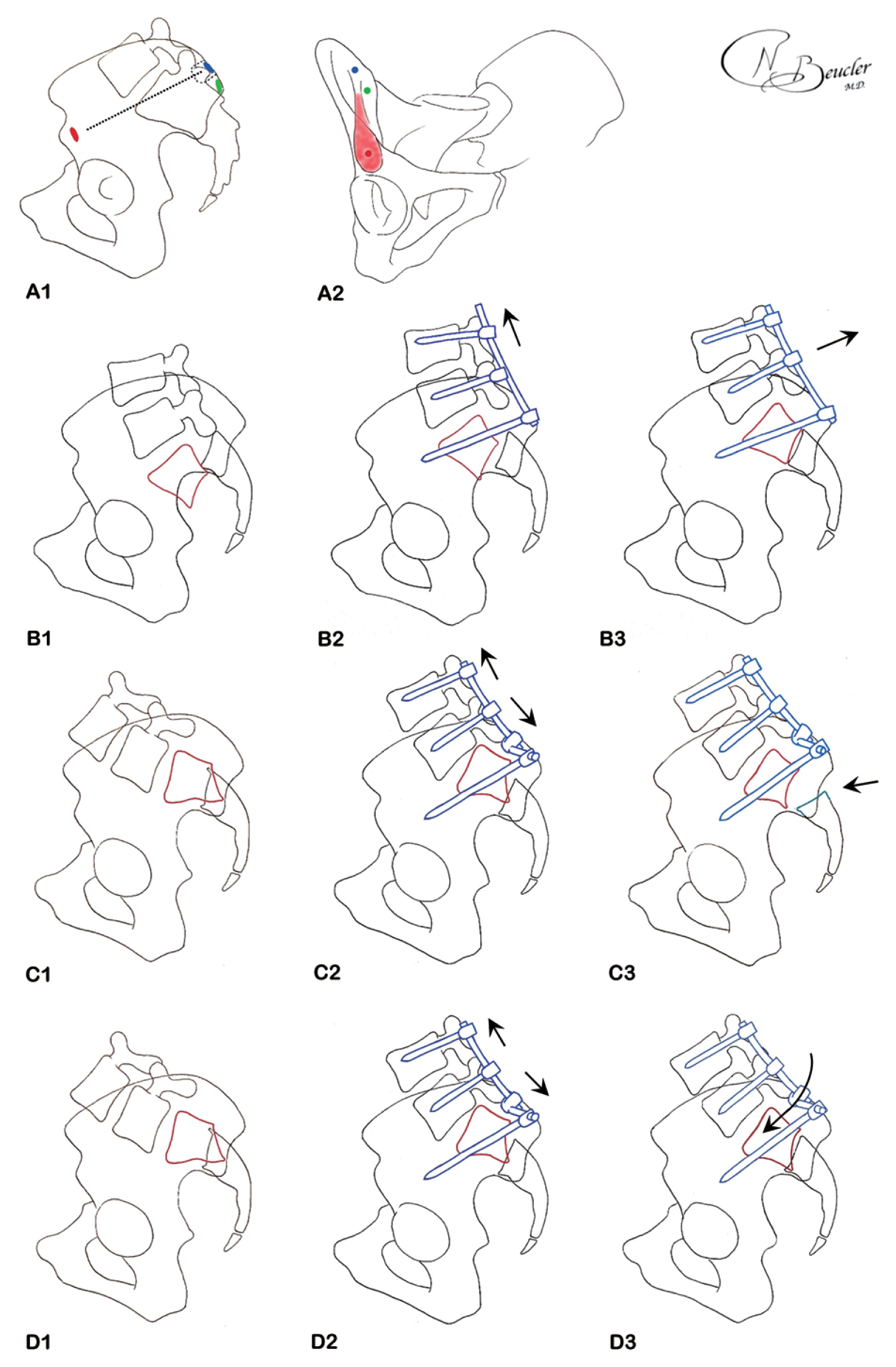
Artistic views of iliac screw placement and reduction techniques for Roy-Camille type 2 and 3 U-shaped sacral fractures. (A) Entry point (blue dot) and objective point (red dot) for iliac screw placement, 1 cm cephalic to posterior superior iliac spine (green dot), in sagittal (A1) and tear-drop (A2) view. (B1) Roy-Camille type 3 U-shaped sacral fracture, (B2) reduction technique (Linhart, 2022) with distraction on L4 pedicle screws and iliac screws, and (B3) persuasion on L5 pedicle screws. (C1) Type 2 sacral fracture, (C2) reduction technique (Fuentes, 2021) with distraction, and (C3) sacral osteotomy. (D1) Type 2 sacral fracture, (D2) reduction technique (current article, patient 2) with distraction, and (D3) manual reduction with direct impaction. Drawings performed by Nathan Beucler.
Sponseller et al. [38] in 2010 introduced S2 sacral alar-iliac fixation as an alternative to classic iliac screws to reduce hardware prominence in children. Then, the technique was adopted for sacral fractures in adults [39].
Sohn et al. [40] in 2016 presented a modified entry point for iliac screws located 1-cm medial and 1-cm caudal to the posterior superior iliac spine. This allowed both direct connections of the iliac screws to the spinal rods without needing a connector and a reduced prominence of the iliac screw under the skin [40].
Schildhauer et al. [36] also described the radiographic teardrop figure formed by aligning the supra-acetabular iliac bone and posterior iliac spines, used to properly insert iliac screws (Fig. 3). The outer edges of the drop were formed using the inner and outer cortical layers of the iliac bone, and the objective was to target the center of the drop, corresponding to the anterior inferior iliac spine (Fig. 2). Nowak et al. [41] in 2021 presented the optimal X-ray placement with 45° axial inclination and 25° sagittal inclination to obtain the teardrop sign in a patient in the prone position.
6) Importance of reducing displaced Roy-Camille type 2 and 3 U-shaped sacral fractures
The sacrum lies directly under the very thin skin of the lower back. Hence, proper reduction of displaced U-shaped sacral fractures is crucial to prevent bed sores, especially in type 2 and 3 fractures where a prominent bone fragment directly points toward the skin [5]. Hence, the radiographic criteria assessing the proper reduction of U-shaped sacral fracture is the reduction of sacral traumatic angulation, also known as sacral kyphosis [5]. A review by Patel et al. [5] demonstrated that the mean reduction of sacral kyphosis was 21.7°.
Ruatti et al. [7] moderately reduced displaced type 2 sacral fractures by applying brutal cranial and caudal traction to the patients placed in an exaggerated hyperextension back position using ligamentotaxis. Complementary intraoperative distraction is typically sufficient in achieving proper reduction, although manual effects might be sometimes necessary. In the case of impacted sacral fragment refractory to manual reduction, Farah et al. [42] in 2022 proposed a sacral osteotomy (Fig. 2).
For displaced type 3 sacral fractures, Linhart et al. [43] in 2022 presented a two-staged reduction method using maneuvers on hardware: vertical displacement was reduced by distracting L4 pedicle and iliac screws, and anterior displacement was corrected using rod persuasion into L5 pedicle screws (Fig. 2).
Non-displaced type 2 or 3 sacral fractures and type 1 sacral fractures generally cause lesser skin tension. In such cases, bone alignment is essentially used for indirect cauda equina decompression, and specific maneuvers are rarely necessary.
7) Decompressive sacral laminectomy
Neurological deficits of the lower limbs and/or perineum were reported in 57%–92% of patients suffering from U-shaped sacral fractures [2,19,24,25]. The Gibbons score by Gibbons et al. [2] became the gold standard for reporting deficits associated with U-shaped sacral fractures [5]. A review by Patel et al. [5] reported that sacral laminectomy was systematically performed in patients with neurological deficits in 11 studies, whereas five studies of neurological decompression were performed either with laminectomy (direct decompression) or proper fracture reduction (indirect decompression). A few authors also used sacral laminectomy to reduce upper sacral fragments under visual control [19,42].
8) Summary of evidence regarding U-shaped sacral fractures
König et al. [17] in 2012 recommended minimal invasive spinopelvic fixation with iliosacral screwing as a first-choice procedure, given the rather good functional recovery with an acceptable complication rate. He then recommended an open procedure for very important bone displacement.
Yi and Hak [6] in 2012 indicated iliosacral screws for minimally displaced U-shaped sacral fractures (Roy-Camille type 1, equivalent to AO Spine C0), but recommended an open procedure with a rigid spinopelvic fixation for very displaced fractures (Roy-Camille type 2 or 3, equivalent to AO Spine C3). Laminectomy was recommended for nerve root compression [6].
A systematic review by Patel et al. [5] in 2022 confirmed the efficacy of spinopelvic fixation for sacral fractures with spinopelvic dissociation. The mean preoperative Gibbons’ score was lower in percutaneous fixation than in open fixation (1.9 versus 2.7); however, he noticed a higher reduction of the Gibbons’ score using an open technique. Although decompressive laminectomy was commonly performed in patients with neurological deficits, there was no strict argument for or against it as long as proper bone alignment was achieved [5].
2. U-shaped sacral fractures, institutional examples
1) Case 1: short-segment spinopelvic fixation
A 32-year-old man was hit by a truck while biking and was projected 10 m away. Upon admission, he presented with a Glasgow Coma Scale (GCS) score of 13 (M6V4E3), neurological deficits of both lower limbs with L5 and S1 deficits ranked Medical Research Council (MRC) scale 2/5, and saddle hypoesthesia. Computed tomography (CT) scan displayed a right hemopneumothorax, grade 4a splenic injury with active bleeding, right psoas and retroperitoneal hematoma, and a Roy-Camille type 1 U-shaped sacral fracture passing through Denis zone II (sacral foramen) on the right side with wide pubic disjunction accounting for a Tile C pelvic disruption. The patient benefited from endovascular embolization and was then closely monitored in the intensive care unit. Open spinopelvic fixation was performed on day 28 using L4 and L5 pedicle screws connected to iliac screws, although spinopelvic fixation with L5 pedicle screws could be possibly sufficient. Moreover, triangular fixation, either with a transverse connector or trans-iliosacral screws, was not performed. Then, he benefited from an open plate and screw pubic fixation in the supine position. Sacral vertical and horizontal displacements were reduced from 12 to 0 mm and from 23 to 5 mm, respectively. His postoperative course was uneventful (Fig. 4). The patient was able to walk with a cane after 2 months and was ranked D on the American Spinal Cord Injury Association (ASIA) scale. Perineal sensibility gradually improved, allowing a urinary catheter withdrawal. Nonetheless, he presented lower limbs and perineal neuropathic pain that was treated with gabapentin.
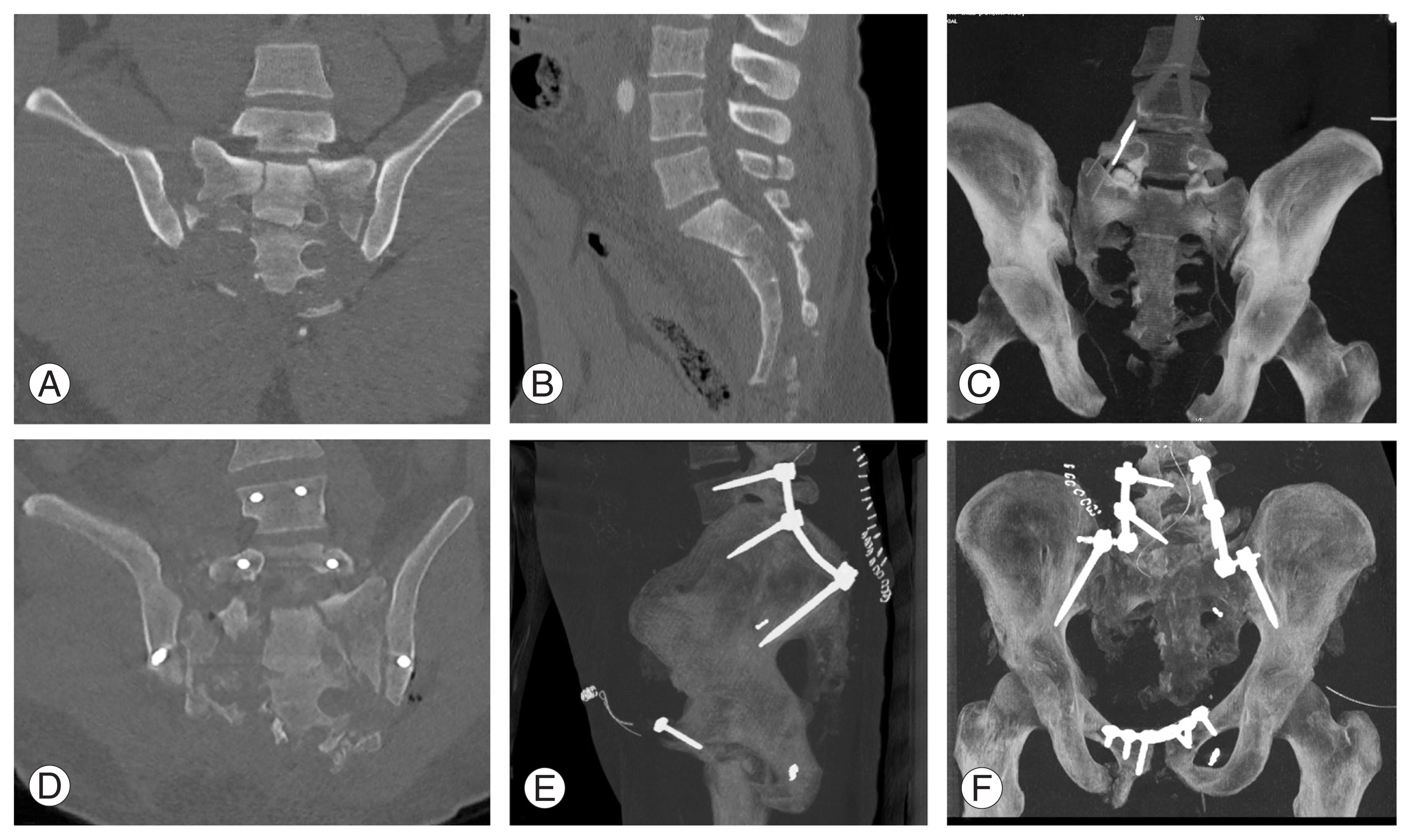
Patient 1: Roy-Camille type 1 U-shaped sacral fracture passing through Denis zone II (sacral foramen), right-sided Tile C pelvic disruption. Preoperative computed tomography (CT) scan in coronal view (A), sagittal view (B), coronal maximum intensity projection (MIP) multiplanar reformation (MPR) (C). Postoperative CT scan in coronal view (A), sagittal view (B), coronal MIP MPR (C) displaying lumbo-iliac fixation and anterior pubic plate and screws.
2) Case 2: long-segment spinopelvic fixation
A 21-year-old man sustained a 12 m fall. On admission, he presented a GCS of 15, and bilateral lower limbs motor ranked MRC scale 3/5 on L3 and L4 segments, 2/5 on the L5 segment, and 0/5 on the S1 segment, hypoesthesia starting at the L5 level, and complete saddle anesthesia with an incompetent anal sphincter, which ranked B on the ASIA score. He presented both conus medullaris and cauda equina compression syndrome. Full-body CT scan detected right rib fractures with right pneumothorax, bilateral foot fracture, and complex spine fractures with a T12 burst fracture (AO Spine A4), L2 and L3 compression fractures, L5 bilateral pedicular fracture, and a Roy-Camille type 2 dislocated U-shaped sacral fracture. Although the patient was slightly hemodynamically unstable, spinal surgery was decided. Then, an open procedure was performed with pedicle screws in T10, T11, L1, L2, L3, L4, and L5 vertebrae connected to iliac screws, which provided a satisfactory vertical distraction. Direct impaction allowed sufficient reduction of the dislocated upper sacral fragment. The dural sac was visible through the S2–S3 fracture site but intact. Two transverse connectors were added for horizontal stability. T12 laminectomy was finally performed. The patient benefited from auto-transfusion following the intraoperative massive transfusion protocol. Sacral kyphosis was reduced from 90° to 35° and vertical displacement was reduced from 10 to 8 mm (Fig. 5). His postoperative course was uneventful. Three months postoperatively, the patient’s neurological motor status had improved to an ASIA D score. Nonetheless, his back pain persisted, and he presented saddle hypoesthesia, requiring urinary self-catheterization.

Patient 2: Roy-Camille type 2 dislocated U-shaped sacral fracture, combined with T12, L2, L3, and L5 spine fractures. Preoperative computed tomography (CT) scan in sagittal view (A), sacrum in coronal (B) and sagittal (C) view. (D) Intraoperative X-ray shows sufficient bone sacral reduction. Postoperative CT scan in maximum intensity projection multiplanar reformation sagittal (E) and coronal (F) view, axial view of iliac screws (G), sagittal view of sacrum reduction (H).
3. Tile C pelvic ring injuries
1) Pathophysiology
Originally described by Malgaigne [44] in 1855, “vertical shear” disruptions of the pelvic ring have been investigated by Tile and Pennal [48] in 1980. Such injuries occur during falls from a height, motor vehicle accidents, or crush injuries causing high-energy vertical forces. Such mechanisms were further confirmed by Ward et al. [9], Dabezies et al. [45], Blum et al. [46], and Liu et al. [47], and illustrated by the mean injury severity score of 29.4 in the Kabak cohort of 40 patients by Kabak et al. [14]. These vertical shear pelvic ring disruptions were described to be unstable [48].
2) First surgical attempts: the birth of iliosacral screws
Historically, vertical shear pelvic fractures were managed with orthopedic treatment using bed rest augmented by traction or pelvic sling [49]. Open reduction was proposed for patients with major displacement [48]. Then, some authors proposed temporary external fixation [50]. Ward et al. [9] in 1987 was among the first authors to propose open surgical treatment with a manual reduction between the sacrum and ilium, and multiple iliosacral screw fixation with visual control was performed on the posterior sacral foramen to prevent sacral nerve roots. Then, Dabezies et al. [45] in 1988 proposed two bi-iliac threaded compression rods combined with anterior pubic fixation.
3) Classifications and criteria of radiologic reduction for pelvic ring disruptions
To compare pelvic rings and their major ligaments to a suspended bridge, Tile [20] in 1988 introduced a three-graded classification of pelvic ring injuries: (1) stable, fractures not involving the ring or minimal ring fractures; (2) rotationally unstable fractures, with complete rupture of the anterior ring and partial involvement of the sacroiliac complex, including open book fractures; and (3) rotationally and vertically unstable fractures, with anterior ring and complete posterior ring disruption, including three major sacroiliac ligaments (sacroiliac, sacrospinous, and sacrotuberous). Open surgery was indicated for type C injuries insufficiently reduced by an anterior external fixator [20]. Nevertheless, the surgical treatment by Tile [20] was confined to the pelvic ring using bi-iliac compression rods or iliosacral screws with pubic fixation and without stabilizing the lower lumbar spine.
Isler [21] in 1990 underlined the importance of lumbosacral instability associated with pelvic ring injuries with sacral fracture involving the L5–S1 facet joint. These fractures, corresponding to Denis et al. [1] in 1988 type 2 (transforaminal, corresponding to AO Spine C1) or 3 (medial to sacral foramen) sacral injuries, warrant that surgical stabilization encompasses the lumbosacral junction (Fig. 1) [21].
Tornetta and Matta [51] in 1996 introduced the remaining vertical displacement as the main radiologic criteria to reduce pelvic ring disruption using three grades: excellent (<4 mm), good (4–9 mm), and fair (10–20 mm).
4) From iliosacral screws to Schildhauer triangular osteosynthesis
Percutaneous iliosacral screw stabilization for vertically unstable pelvic ring injuries was introduced in the early 1990s [27]. However, Schildhauer et al. [32] was convinced that iliosacral screw fixation remained at high risk of rotational instability. Hence, he introduced the concept of triangular osteosynthesis using lumboiliac distraction osteosynthesis to treat vertical instability and a complementary iliosacral screw or trans-sacral plate fixation to treat horizontal instability in a series of 34 patients, aiming to allow early weight bearing. A total of 19 patients achieved partial weight bearing at day one and full weight bearing after a mean delay of 23 days [11].
The findings by Schildhauer et al. [32] were further confirmed for type II Denis fracture treated with triangular lumboiliac and iliosacral fixation with good outcomes according to the Majeed score [52,53]. Finally, Prost et al. [8] also achieved good outcomes for vertically unstable posterior pelvic ring injuries treated with minimal invasive triangular fixation.
5) Toward personalized treatments of vertical shear pelvic ring injuries
Blum et al. [46] in 2018 proposed a treatment algorithm for Tile C (AO Spine C2 and C3) pelvic ring injuries: (1) In patients with a posterior pelvic ring located lateral to the sacral foramen and if no other sacral fractures compromise the surgical corridor, then an iliosacral screw can be sufficient. Placing at least two screws at S1 and S2 on each injured side may reduce any potential rotational instability. (2) In patients with complex sacral fractures located at (Denis zone II) or medial to the sacral foramen (Denis zone III) or in patients with sacral fractures compromising the future corridor of any iliosacral screw (Strange-Vognsen grade 4), then open spinopelvic fixation is indicated.
4. Tile C pelvic ring injuries, institutional example
1) Case 3
A 33-year-old man sustained a motorcycle accident against a bus. On emergency room admission, he presented with a GCS score of 3 and was hemodynamically unstable. Full-body CT scan displayed nonsurgical mild traumatic brain injuries, right complete pneumothorax and bilateral pulmonary contusions, right-hand fracture, and right-sided Tile C pelvic ring injury without active pelvic bleeding. The pneumothorax was treated with a chest tube, and the patient was admitted to the intensive care unit. Delayed awakening revealed diffuse axonal injury on brain imaging; however, the patient’s neurological status gradually improved (GCS 13). Thus, delayed open unilateral right-sided spinopelvic fixation was performed on day 11 using L4 and L5 pedicle screws connected to an iliac screw, although an L5 pedicle screw could have been possibly sufficient. On day 13, the patient underwent right-sided S1 and S2 iliosacral screw placement, thus obtaining an authentic triangular construct. Finally, anterior pubic fixation was performed on day 19 (Fig. 6). Vertical and horizontal displacements were reduced from −10 to +4 mm and from 13 to 10 mm, respectively. Late wound infection was observed. Given that bone fusion was achieved, wound debridement and washing concomitant to hardware removal were performed at 6 months postoperatively, combined with proper antibiotic therapy. Later, the orthopedic restrictions on his daily activities were lifted.
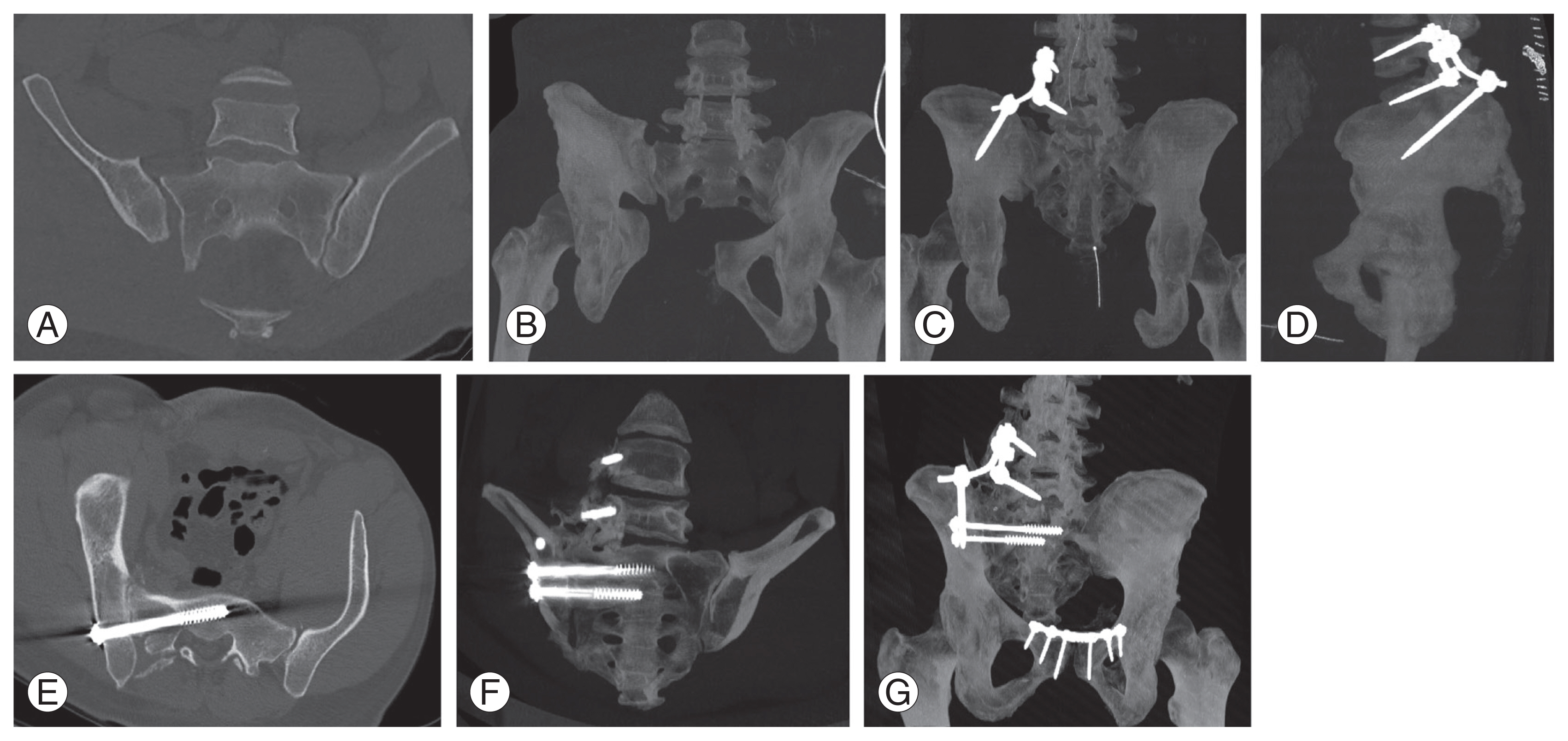
Patient 3: right-sided Tile C pelvic ring injury. (A, B) Preoperative computed tomography (CT) scan in coronal (A) and coronal maximum intensity projection (MIP) multiplanar reformation (MPR) (B) view. (C, D) CT scan in MIP MPR view after lumbo-iliac fixation in coronal (C) and sagittal (D) view. (E, F) CT scan of ilio-sacral screws in axial view (E) and coronal MIP MPR (F). This constitutes classic triangular osteosynthesis described by Schildhauer. (G) Coronal MIP MPR after pubic fixation.
5. Specific surgical considerations
1) Timing of surgery
Unstable U-shaped sacral fractures and pelvic ring injuries occur in patients with very serious severe trauma often presenting life-threatening trauma lesions [15]. Hence, anterior pelvic external fixation appears to be the treatment of choice in emergency cases [24]. Definitive surgery was performed after a mean delay of 9 days in patients with U-shaped sacral fractures [24,25] and 4.6–13 days in patients with pelvic ring disruption [8,11,20]. In the review by Patel et al. [5], the mean delay to surgery was 9.1 days.
2) Intraoperative considerations
Spinopelvic fixation is a heavy spinal trauma surgery requiring wide bone exposure for proper hardware placement with a mean operative time of 100–326 minutes for open procedures [23–25] and 137 minutes for minimal invasive triangular construct [8]. The review by Patel et al. [5] reported a mean operative time of 166 minutes.
Such procedures are associated with significant blood loss. Tan et al. [25] reported a mean blood loss of 1,033 mL for open procedures, and the review by Patel et al. [5] reported a mean blood loss of 474 mL with a significantly decreased blood loss for percutaneous fixation.
3) Postoperative complications
Given the trauma setting, the thin characteristics of the skin above the sacrum, the prominence of iliac hardware, and the proximity of the perineal area, lumbopelvic fixation is significantly associated with perioperative morbidity.
Several authors reported varied postoperative complications. Wound dehiscence was reported in 7.4%–13% of the cases [5,23], wound infection in 7.2%–13% [5,11,14,23], hardware failure in 9%–13% [11,23], hardware prominence in 21%–100% leading to hardware removal in 11%–100% [5,24], and iatrogenic neurological injury in 3% of the cases [11]. In summary, the review by Patel et al. [5] revealed that wound dehiscence, wound infection, and iliac hardware prominence leading to hardware removal in 11% of cases occurred in 7.4%, 7.2%, and 21.3%, respectively.
Lastly, caregivers should be advised to look for peculiar trauma complications, such as Morel-Lavallée lesions, which may be a supplementary risk factor for wound complications [54].
Discussion
1. Preoperative considerations
Unstable U-shaped sacral fractures and Tile C pelvic disruptions are characterized by high-energy trauma lesions occurring in patients with severe trauma. In an acute setting, management is aimed at stopping any eventual life-threatening active bleeding and performing damage-control treatments for unstable spinopelvic lesions, oftentimes with an anterior external pelvic fixator [15,16,24,55]. Surgical treatment of unstable spinopelvic injuries remains a surgical challenge even for experienced spine surgeons, which should be scheduled in a subacute setting in a hemodynamically stable patient [5,8,11,24,25,30].
2. Surgical treatment of U-shaped sacral fractures
Non-displaced U-shaped sacral fractures (AO Spine C0) without neurological deficits can be managed conservatively if the patient suffers from other lesions requiring bed rest. Orthopedic treatment or iliosacral screws can be indicated for slightly displaced Roy-Camille type 1 U-shaped sacral fractures [7,56]. Type 2 and 3 U-shaped sacral fractures (equivalent AO Spine C3) frequently require surgical stabilization. Multiple efficient reduction techniques have been proposed, including external maneuvers [7], osteotomy [42], and hardware maneuvers [43]. Stabilization is achieved using triangular spinopelvic fixation, either with the technique by Schildhauer et al. [11] or modified fixation using a transverse connector [24].
The operator should strive to achieve sufficient vertical distraction during spinopelvic fixation using iliac screws associated with L5 and S1 pedicle screws to reduce the risk of adjacent lumbar segment diseases. Nevertheless, sometimes the lever arm is necessary to reduce vertical displacement [8], the need for hardware maneuver reduction techniques [43], or the Strange-Vognsen grade four sacral fracture by Strange-Vognsen and Lebech [22] requires the use of L4 pedicle screws.
In case of neurological deficits, the need for complementary sacral laminectomy remains at the operating surgeon’s discretion due to the lack of evidence on this matter [5]. Indeed, sacral laminectomy may unduly reveal a contained traumatic dural tear with a high risk of cerebrospinal fluid leak and wound infection [4,33].
3. Surgical treatment for Tile C pelvic ring injuries
Posterior ring disruptions located lateral to the sacral foramen and with only moderate vertical displacement can be efficiently stabilized using either multiple iliosacral screws or triangular spinopelvic fixation. In patients requiring vertical displacement indicated with complete rupture of the sacroiliac complex inducing vertical instability, triangular spinopelvic fixation is required. Conversely, transforaminal sacral fractures (Denis zone II, equivalent AO Spine C1) or fractures located medially to the sacral foramen (Denis zone III) also destabilize the lumbosacral junction [1,21]. These injury patterns require triangular spinopelvic fixation (Table 1) [11].
4. Timing of anterior pelvic ring fixation
For Tile C pelvic ring injuries or sometimes unstable U-shaped sacral fractures, surgical treatment of the associated anterior pelvic ring disruption, whether it involves the pubic symphysis or rami, should ideally be performed afterward despite the absence of formal consensus on the matter [30]. Otherwise, proper reduction of the posterior pelvic ring injury may be hampered, thus jeopardizing the patient’s functional prognosis [57].
Conclusions
Unstable U-shaped sacral fractures and Tile C vertical shear pelvic ring injuries result in the occurrence of rare lesions in patients with severe trauma. These lesions warrant surgical treatment after hemodynamically stabilizing a patient. Although there is still no consensus regarding the appropriate surgical technique, iliosacral screws can be indicated for non-displaced lesions, whereas more unstable or displaced fractures require triangular spinopelvic osteosynthesis. The need for complementary sacral laminectomy remains at the surgeon’s discretion. Due to the demands required in these techniques, the operating surgeon must use the technique best suited for him or her to safely complete the procedure. If needed, fixation of the anterior pelvic ring should be performed afterward.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
NB designed the article. NB, PT, and AD participated to the clinical care of the patients. NB, PT, and AD participated to the literature review. NB, PT, and AD participated to the drafting of the manuscript. NB conceptualized the illustrations. NB, PT, and AD participated to the critical revision of the manuscript. NB performed the final revision of the manuscript.



