A New Technique for Lumbar Spondylolisthesis Reduction Using T-Shaped Tools
Article information
Abstract
Study Design
Retrospective study.
Purpose
To introduce a simple technique to facilitate lumbar spondylolisthesis reduction during posterior lumbar interbody fusion (PLIF).
Overview of Literature
Spondylolisthesis reduction has been conducted in various ways, but most of them require special complicated tools.
Methods
T-shaped levering tool was newly designed. This study included 23 patients who underwent PLIF for lumbar spondylolisthesis treatment using newly designed T-shaped tools and followed up for >2 years. Demographic, clinical, and surgical data, which had been routinely collected in a database, were analyzed. The degree of listhesis was measured on lateral radiographs by the Taillard method.
Results
The authors could achieve lumbar spondylolisthesis reduction without difficulty using newly designed T-shaped tools. Immediate postoperative lateral radiographs revealed a reduced preoperative slip of 36.9%±9.6% to 1.2%±1.9%, showing a correction rate of 96.7%. The final follow-up radiographs revealed the mean final slip of 2.6%±2.7%, showing a correction rate of 93.0%.
Conclusions
This technique allowed lumbar spondylolisthesis reduction without difficulty.
Introduction
The issue of surgical lumbar spondylolisthesis reduction versus in situ fusion remains controversial. Many satisfactory clinical outcomes have been reported in the in-situ fusion of low-grade spondylolisthesis. However, historically, many studies have reported significant rates of nonunion or subsequent slip-on in-situ fusion of high-grade spondylolisthesis [1–5]. Surgical techniques to reduce spondylolisthesis have been developed and conducted in various ways, including Harrington rod distraction using additional sacral bar fixation [6], sacral hook plate and double threaded pedicle screws [7], and assembly of the reduction instrument [8,9]. However, they required extensive incisions, special complicated tools, or extra-cost of implants. We designed a T-shaped levering tool to facilitate lumbar spondylolisthesis reduction during posterior lumbar interbody fusion (PLIF). The tool was modeled after the atlantoaxial reduction tool of Suh et al. [10]. This study describes the use of this tool and reports its application outcomes.
Materials and Methods
1. Participant
This retrospective, single-institution, observational study included 23 consecutive patients who underwent single-level PLIF for isthmic or degenerative lumbar spondylolisthesis treatment using new reduction tools from April 2018 to May 2020. The average age of patients was 63.3 years (range, 50–79 years), with 11 males and 12 females. Degenerative spondylolisthesis was diagnosed in 17 patients and isthmic spondylolisthesis in 11 patients. The surgery levels were L3–L4 (two patients), L4–L5 (17 patients), and L5–S1 (four patients). The follow-up period was 24–49 months with an average of 29.3 months.
All operations were performed by a single surgeon (J.Y.), who designed the new reduction tool. The study was approved by the institutional review board of Dankook University College of Medicine (approval no., 2021-11-07-002), and informed consent was obtained from the study participants.
2. Reduction tool
This tool is designed similarly to the tool made by Suh et al. [10]. The reduction tool was designed to have three parts: a grip handle (length: 90 mm), a shaft (length: 110 mm; diameter: 6.0 mm), and a distal bar (length: 50 mm; diameter: 6.0 mm). The distal bar joins to the shaft at a right angle. It was made in pairs to engage both screws on both sides (Fig. 1).
3. Reduction technique
(1) After segmentally inserting the pedicle screws, the distal bar of a T-shaped tool is loosely secured to the heads of the polyaxial pedicle screws using set screws in the same way as positioning the rod (Figs. 2A, 3B). One T-shaped tool is applied on one side pedicle screws, and the other on the other side pedicle screws. (2) The handles of the two T-shaped tools are levered caudally simultaneously for lumbar spondylolisthesis reduction (Fig. 3B), in such a manner that the cranial pedicle screws are pulled up as the caudal pedicle screws are pushed down (Fig. 2B). (3) The set screws are tightened to temporarily hold the reduction. (4) Reduced state is checked using lateral C-arm fluoroscopy (Fig. 3C). (5) After achieving adequate reduction, the two T-shaped tools are sequentially replaced with the final rods, thereby maintaining reduction. (6) The reduction is finally checked using lateral C-arm fluoroscopy (Fig. 3D) and/or lateral radiography (Fig. 3E).
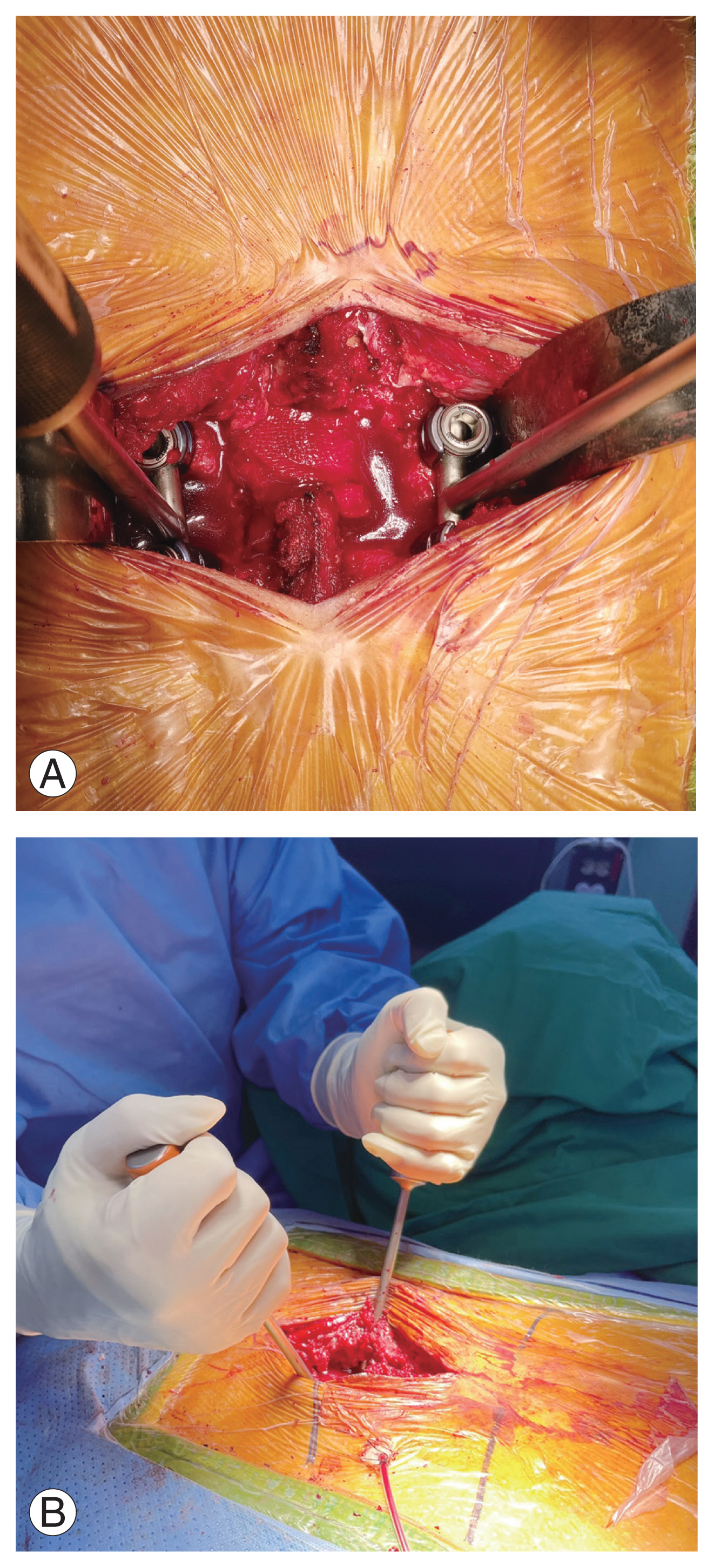
(A) The tool is loosely secured to the heads of pedicle screws with set screws before reduction. (B) During reduction, the handle is levered caudally, such manner that the cranial pedicle screws are pulled up as the caudal pedicle screws are pushed down.

Images of a technique for reducing spondylolisthesis using two T-shaped tools. (A) Lateral radiograph shows isthmic spondylolisthesis of L5 on S1 in a patient. (B) In the lateral fluoroscopic image, the tool is loosely secured to the heads of pedicle screws with set screws before reduction. (C) After reduction maneuver, the spondylolisthesis is reduced. (D) The fluoroscopic image showing the two T-shaped tools which were replaced with two final rods. (E) A postoperative lateral radiograph showing remarkable reduction.
4. Brief surgical procedure
All patients underwent laminectomy, which involves the lower half of the laminae of the cephalad vertebra or complete removal of the floating laminae, medial facetectomy, and foraminotomy. A rectangular annular incision was made after the medial retraction of the nerve roots. The disc space contents were then completely removed and the cartilaginous end plates were removed by curettage. An autogenous local bone graft (morselized posterior elements) was packed into the disc space. Then, polyetheretherketone cages filled with local bone were inserted and pedicle screws were introduced. Spondylolisthesis reduction was performed using T-shaped tools as described in the section above. Finally, the pedicle screws were tightened and compressed. Bilateral posterolateral fusion was added after decorticating residual posterior elements.
5. Data analysis
Data analysis was independently performed by two experienced spinal surgeons with more than a decade of experience who were not involved in patient care. Demographic, clinical, and surgical data, which had been routinely collected in a database, were analyzed. Patients completed preoperative and postoperative surveys recording the intensity of back pain and pain radiating to the lower extremity based on a 10-point Visual Analog Scale (VAS) and Oswestry Disability Index (ODI).
6. Radiologic evaluation
Radiography was checked preoperatively, immediately postoperatively, and every time the patient visited the clinic. The Taillard method was used to measure the degree of listhesis on the lateral radiographs [11]. Computed tomographic (CT) images were obtained 12 months postoperatively to evaluate fusion status. The presence of bone bridging through the cage or external to it on sagittal and coronal reconstructed CT scans, as demonstrated in the slices, was assessed as a bone union.
7. Statistical analysis
Paired t-tests were used for all analyses. The IBM SPSS software ver. 20.0 (IBM Corp., Armonk, NY, USA) was used to perform analyses, and a two-sided p-value of <0.05 was considered statistically significant.
Results
1. Reduction of listhesis using the new tools
The immediate postoperative lateral radiographs revealed a reduced preoperative slip from 36.9%±9.6% to 1.2%±1.9%, showing a correction rate of 96.7%. The final follow-up radiographs revealed the mean final slip of 2.6%±2.7%, showing a correction rate of 93.0%. Immediately after and the last slip revealed a statistically significant difference from the preoperative slip (p<0.001, respectively).
2. Union
Bone union was achieved in 19 patients (86%). Nonunion was observed in three patients.
3. Clinical outcome
At the last follow-up, preoperative VAS scores for back pain were improved from 5.6±1.7 to 2.1±1.9 (p<0.001). Radiating pain intensity scoring of the lower extremities was improved from 7.1±2.8 to 1.9±2.6 at the last follow-up (p<0.001). ODI scores revealed a marked improvement from 54.6±16.4 to 22.3±14.8 (p=0.001).
4. Complications
A case of a back-out of the pedicle screw occurred during levering of T-shaped tools in a patient with osteopenia who underwent L4–L5 degenerative spondylolisthesis reduction. We reinserted the pedicle screw after adjusting its convergence angle and tried the same technique which resulted in a successful reduction.
Of the three cases of nonunion, re-slip occurred in only one case (0% on immediate postoperative, but 9% on 26 months postoperative). However, no significant deterioration of symptoms was found in the case.
Discussion
The efficacy of surgical reduction of slipped vertebrae remains controversial regarding surgical lumbar spondylolisthesis treatment. Slipped vertebrae reduction results in a recovery of sagittal imbalance and restoration of the original neuroforaminal morphology. Several studies evaluating the effect of the slippage reduction revealed no correlation between radiological and clinical outcomes and claimed that radiological outcomes by intentional reduction may not proportionally indicate better clinical outcomes [12,13]. However, Wegmann et al. [14] revealed that spondylolisthesis reduction is associated with a significantly better quality of life. Kawakami et al. [15] reported that the sagittal deformity correction by spondylolisthesis reduction may be important in a long-term period by preventing the disc degeneration of an adjacent level.
Currently known surgical techniques to reduce spondylolisthesis, including Harrington rod distraction using additional sacral bar fixation [6], sacral hook plate and double threaded pedicle screws [7], and assembly of the complicated reduction instrument [8,9], require extensive incisions, special complicated tools, or extra-cost of implants. Our new technique does not need additional cost except for the initial production cost of the T-shaped tool, and additional incision or bone fixation. It does not cost much to produce the T-shaped tool compared to producing other surgical instruments. Assembling the T-shaped tools into the pedicle screws is not difficult because it does not require more space. Strong forces can be applied because two of the T-shaped tools are simultaneously applied on the bilateral pedicle screws. Using this tool, the reduction was almost complete with a correction rate of 96.7%, which is higher than other studies ranging from 51.6% to 95% [8,9,16].
This study used this tool only for spondylolisthesis reduction. However, retrolisthesis and rotational deformity reduction are also possible according to the authors’ experience depending on the direction of levering. This technique may be used for severe spondylolisthesis once the facet joints are released enough and discectomy is performed, thereby easily achieving a reduction. We did not use preliminary traction after decompression; however, it may be useful in very narrow disc spaces. The same maneuver may be utilized with two strong clamps fixed to the rods if the T-shaped tools are not available. However, clamps are usually bulky compared to T-shaped tools and could be disassembled during the maneuver.
Suh et al. [10] have reported a tool with no financial restriction. Our tool works on the same principle as that of the study by Suh et al. [10] but is different in size and location of usage.
All the included patients in this study were surgically reduced without difficulty. A case of a back-out of the pedicle screw occurred during tool levering. However, the successful reduction was achieved after trying the same technique after reinserting that screw.
Therefore, the biggest advantage of the newly designed T-shaped tool is that it provides a simple, convenient, precise, and safe method of reducing any type of spondylolisthesis.
The limitation of our study is the small number of cases and the retrospective design. We did not analyze the correlation between lumbar lordosis and pelvic incidence. Analysis of the types of spondylolisthesis has not been conducted. Quantitative analysis of postoperative slippage was not performed because the follow-up period is not consistent. This is a task to be solved in future prospective studies that include many cases.
Conclusions
We describe the use of a simple T-shaped tool to facilitate lumbar spondylolisthesis reduction during PLIF. This tool allowed for controlled reduction with a correction rate of 96.7% without difficulty or complications.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
All the work was done by Jemin Yi.

