Introduction
C2 segmental screws can be placed in the pedicle, pars, or lamina. In most cases, two pedicle or laminar screws can be placed, which can provide sufficient C2 fixation. However, multiple screw placement in the C2 vertebra, that is, the placement of three or four screws in C2, may be considered or required in several situations, as follows. First, it may be considered in some cases during occipitocervical fixation and fusion (
Fig. 1). Occipitocervical fixation and fusion, using an occipital plate and cervical screws, may need to be extended to the subaxial spine to enhance the stability of the construct. This extension is particularly required in selected cases, including patients with severe osteoporosis, those undergoing complex revisions with loosening of previously placed screws, those with bone defects or screw cutout resulting in weak anchor points, those with small bone dimensions that cannot accommodate adequately sized C2 pedicle screws, and those with anterior column defects. However, the number of fusion levels should be minimized whenever possible. Additionally, extending the fusion caudally below the C2 vertebra would necessitate detaching the major neck extensor muscles from the C2 spinous process, which could increase neck pain and kyphosis and limit movements [
1]. Therefore, ideally, occipitocervical fusion should be limited to the C2 vertebra and above. This can be achieved by reinforcing fixation with multiple (three or four) screw fixation in C2. Second, the placement of three or four screws in C2 may prove beneficial even during C1–C2 fusion in specific cases, such as severe osteoporosis or revision cases where previously inserted C2 screws have become loose (
Fig. 2). This is particularly relevant when C2 pedicle screws are not feasible. Third, a long fusion extending from C2 or above to a level far below C2 may require additional fixation to ensure adequate stabilization in some cases, such as osteoporosis, cerebral palsy, and complex reconstructive or revision surgery (
Fig. 3). A possible alternative for stabilization augmentation in these situations is the placement of laminar screws at C2 [
2] and C7 [
3] and/or upper thoracic levels [
4], along with interconnection between them. This approach also requires multiple screw fixation in C2.
In these unique situations, we have been placing multiple (three or four) screws in C2 for several cases since 2007. We have presented our principles and cases at many international and domestic conferences and instructional course lectures. Meanwhile, several case reports on placing multiple screws for C2 fixation have been published [
5–
9]. However, to the best of our knowledge, no reports have analyzed the feasibility of multiple screw fixation in C2. Therefore, this study aimed to investigate the anatomical feasibility of achieving multiple fixation points in C2 using a combination of pedicle and laminar screws.
Materials and Methods
1. Selection criteria
This study was approved by the institutional review board of Seoul National University Bundang Hospital (B-1303/194-105). Computed tomography (CT) scans of the cervical spine with an interval of 1 mm, taken in a single institution (Mx8000 IDT 16; Philips Medical System, Best, The Netherlands) from June 2009 to February 2013, were initially included in this study for analysis. The exclusion criteria were as follows: (1) CT scans of patients under the age of 20 years; (2) those with unsatisfactory imaging of C2, such as those with severe metal artifacts caused by dental implants; (3) congenital anomalies, infection, tumors, and fractures involving C2; and (4) postoperative CT scans. Among those fulfilling the selection criteria, an equal number of consecutive patients were selected for each sex.
2. Computer simulation and screw trajectories
The analyses were performed using computer simulation with three-dimensional (3D) screw trajectory simulation software (Vworks, Cybermed Inc., Reston, VA, USA). This software allowed the reconstruction of a 3D model, along with coronal and sagittal images, from axial CT scan images of the cervical spine taken at 1.0-mm intervals. Screw insertion was simulated simultaneously using these images as reference (
Fig. 4). The software facilitated the determination of the entry point, trajectory, diameter, and length for each screw.
The diameter of all screws was set at 3.5 mm, considering its common usage in real surgery. C2 pedicle screws were directed approximately 30°–40° medially on the axial plane, toward the anterior–superior end of the superior articular process of C2 or just below it, along the superomedial margin of the pedicle [
10] (
Fig. 4A). The entry point was positioned 3–7 mm caudal to the C1–C2 facet joint and 3–7 mm lateral to the medial border of the pars to accommodate the described trajectory. The entry point for a C2 laminar screw was at the junction of the spinous process and lamina [
2] (
Fig. 4B). To prevent collision between the two laminar screws, the entry points were adjusted cranially and caudally, respectively. Each laminar screw was aligned along the slope of the contralateral laminar surface, avoiding breaches of either the anterior or posterior cortices of the lamina and collisions between the bilateral laminar screws and between the pedicle and laminar screws.
3. Feasibility evaluation
Two types of analyses were conducted. First, the anatomical feasibility of placing both pedicle and laminar screws on the same side was evaluated for each side. “Cortical breach” was defined as any violation of the outer margin of the cortical bone. The anatomical feasibility of the pedicle or lamina to accommodate a 3.5-mm screw without cortical breach was assessed for each screw. The “success” of screw placement was defined as placement without cortical breach. Second, when both pedicle and laminar screws were feasible on the same side, the 3D distance between their entry points was measured to evaluate whether the distance is sufficient to allow screw placement without collision between the heads of the ipsilateral pedicle and laminar screws.
Results
1. Patient demographics
CT scans of 100 patients, including 50 consecutive patients for each sex, who fulfilled the selection criteria were analyzed in this study. The mean age of the patients was 50±9 years (range, 25–77 years). We simulated insertion of 200 pedicle and 200 laminar screws.
2. Anatomical feasibility of multiple screw placement in C2
In 85 of the 100 patients, both pedicle and laminar screws were feasible, bilaterally permitting the insertion of four screws into C2 (
Table 1). Among the remaining 15 patients, 11 could accommodate both screws on one side and only one screw on the contralateral side at C2 (permitting the insertion of three screws): two pedicle and one laminar screws in four patients and one pedicle screw and two laminar screws in seven patients. The other four patients could accommodate only one screw on each side (permitting only two screws): one pedicle screw on each side in one patient, one laminar screw on each side in two patients, and one pedicle screw on one side and one laminar screw on the contralateral side in one patient.
As shown in
Table 2, pedicle screws were feasible in 187 of 200 sides, and the upper and lower laminar screws were feasible in 96 and 98 of 100 sides, respectively. On the upper laminar screw side, the placement of both laminar and pedicle screws was feasible in 89 of the 100 patients, and the mean distance between the entry points of both screws was 19.0±1.6 mm with a minimum of 16.1 mm. On the lower laminar screw side, the placement of both laminar and pedicle screws was feasible in 92 of the 100 patients, and the mean distance between the entry points of both screws was 21.1±3.0 mm with a minimum of 16.8 mm. Overall, the minimum distance between the entry points of the ipsilateral pedicle and laminar screws was 16.1 mm, which was sufficient to prevent collision between the heads of the ipsilateral pedicle and laminar screws.
Discussion
Strong posterior fixation of C2 can be achieved by bilateral pedicle screw placement in most cases. However, in some cases, bilateral pedicle screws are not feasible, and multiple screw placement is required or beneficial, as described in the Introduction section. The corresponding author has presented his experience of multiple C2 screw placement in many meetings, and we believe that this technique is becoming increasingly popular. However, we could not find a study analyzing the feasibility of multiple screw fixation in C2. Therefore, we conducted this study to analyze the anatomical feasibility of pedicle and laminar screws and the distance between the heads of the two ipsilateral screws to assess the frequency of collision between them.
This study demonstrated that in 85% of cases, both pedicle and laminar screws were feasible bilaterally, allowing for the insertion of four screws. In 11% of cases, two screws were feasible on one side, and only one screw was feasible on the other side, allowing for the insertion of three screws. Of the 200 sides analyzed, 181 permitted the placement of both pedicle and laminar screws, with a minimum distance of 16.1 mm between the entry points of the two screw types. Therefore, the distance was sufficient to prevent collisions between the screw heads on all 181 sides. Consequently, in 96% of cases, the placement of 3 (11%) or 4 (85%) screws in C2 was feasible.
Similar to any other study, this study had several limitations. First, this study was based on computer simulation, which is not as realistic as real surgery. As previously mentioned, we have been placing multiple screws in C2 for several cases since 2007, and we are planning to report our clinical results of this technique in another paper.
Second, we have not analyzed the feasibility of screw and rod assembly. It is mostly determined by the mobility of screw heads and the versatility of accessories for connection, such as lateral extenders and crosslinks.
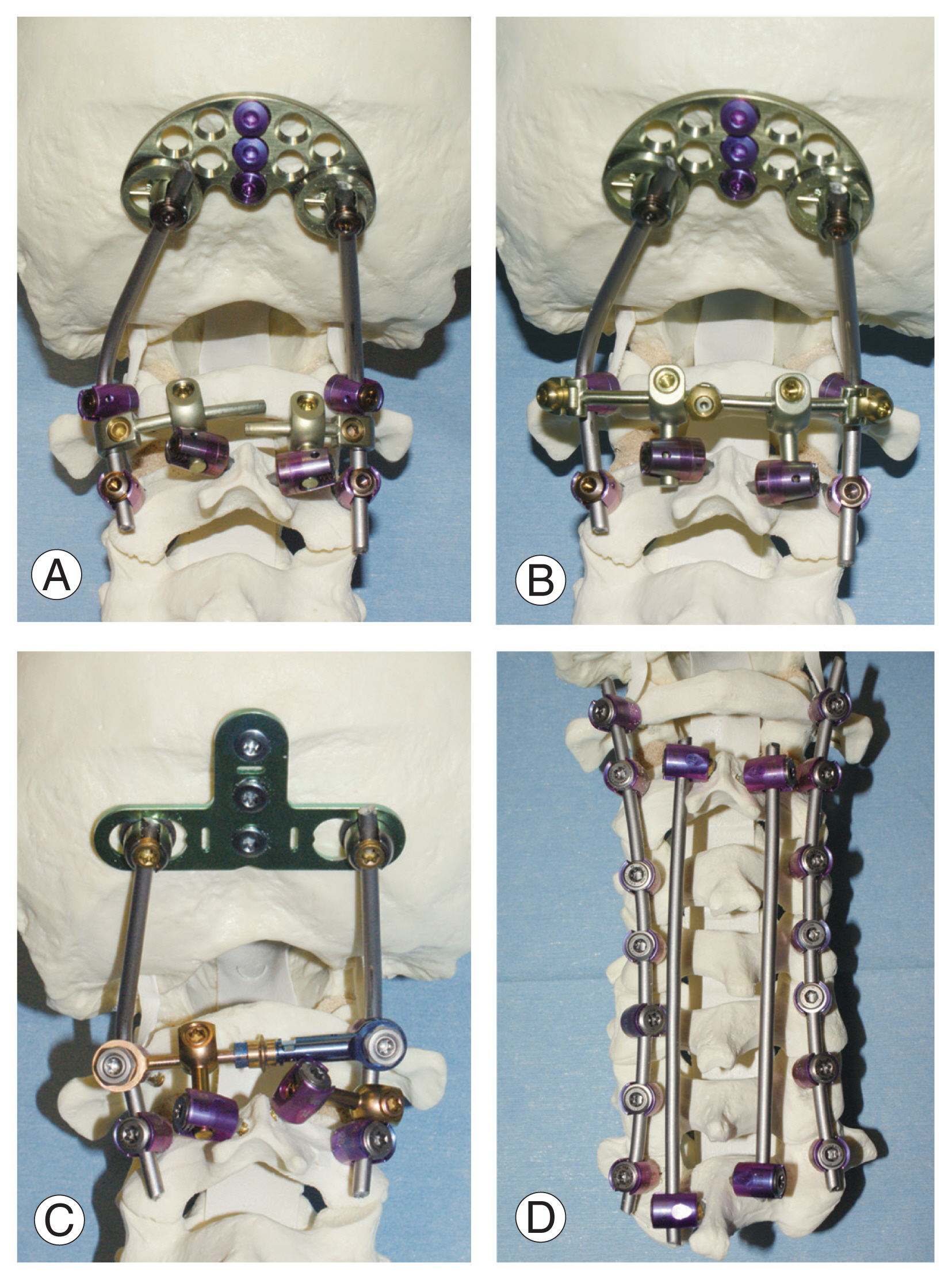
Fig. 5 shows several examples of screw–rod assembly. Among our clinical experience of several hundreds of cases, we have experienced less than five cases where assembly was impossible. Of note, another issue is bone graft placement through the crowded connecting accessories. We recommend placing bone grafts before the assembly of the last laminar screw.
Third, we have not analyzed the biomechanical advantages of placing multiple screws in C2. Considering that multiple screw placement is required only in unusual and unique situations, we believe that conducting this kind of study with reliable statistical analysis would not be feasible.
Conclusions
This study aimed to analyze the feasibility of achieving multiple (three or four) screw fixation points in C2 using a combination of pedicle and laminar screws. We found that in 85% of cases, both pedicle and laminar screws could be placed on both sides, allowing for the insertion of four screws. In 11% of cases, two screws could be placed on one side, whereas only one screw was feasible on the other side, resulting in the placement of three screws. Across all 181 sides where both pedicle and laminar screws could be inserted, the distance between the entry points of the two screw types exceeded 16.1 mm, which was sufficient to prevent collisions between the screw heads. Consequently, in 96% of cases, the placement of 3 (11%) or 4 (85%) screws in C2 was feasible.
Acknowledgments
This study was supported by a research grant of Seoul National University Bundang Hospital (grant number: 02-2014-060).
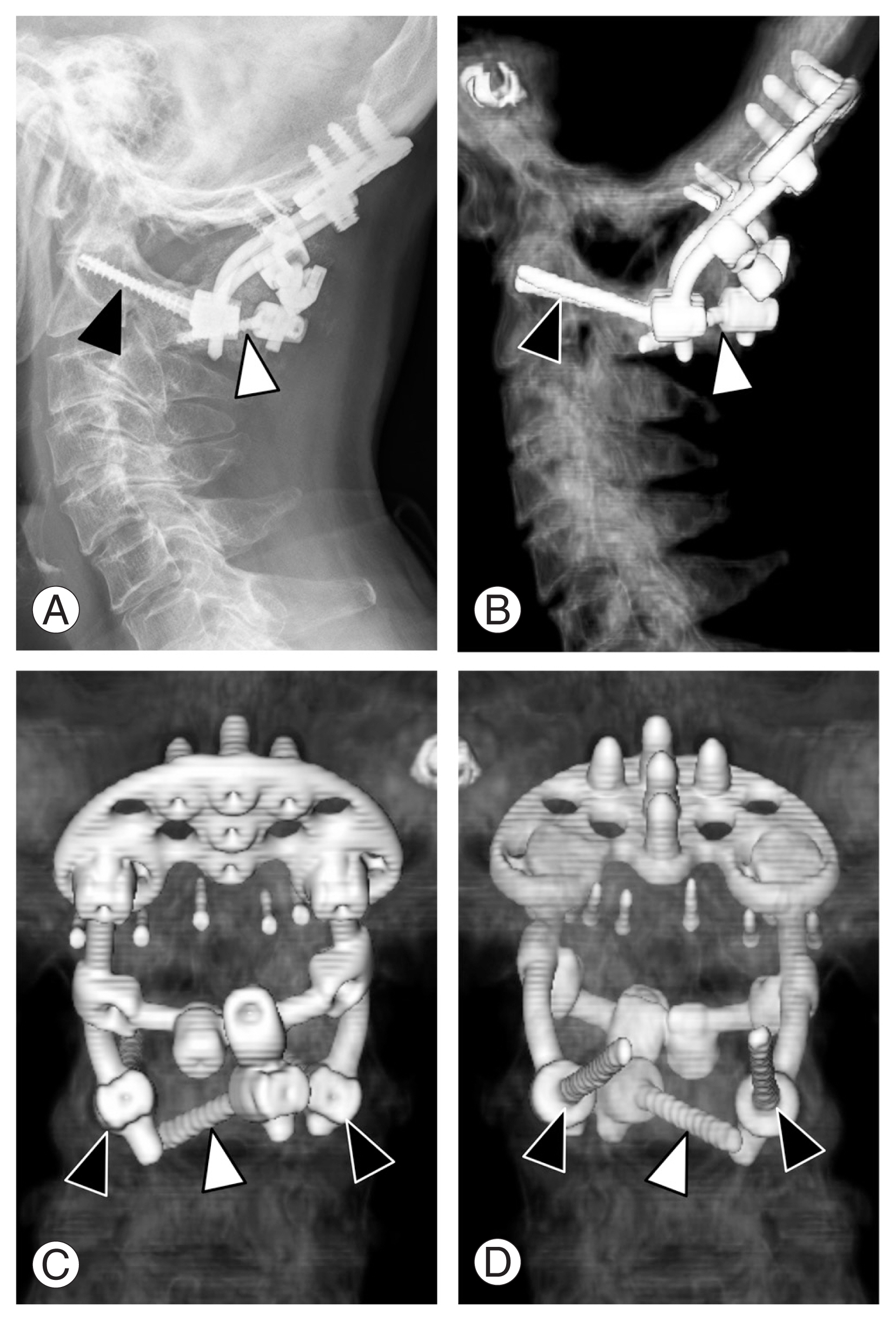
Fig. 1
(A–D) In this case with occiput-C2 fusion, C2 fixation was carried out using two pedicle screws (black arrowheads) and a laminar screw (white arrowhead).
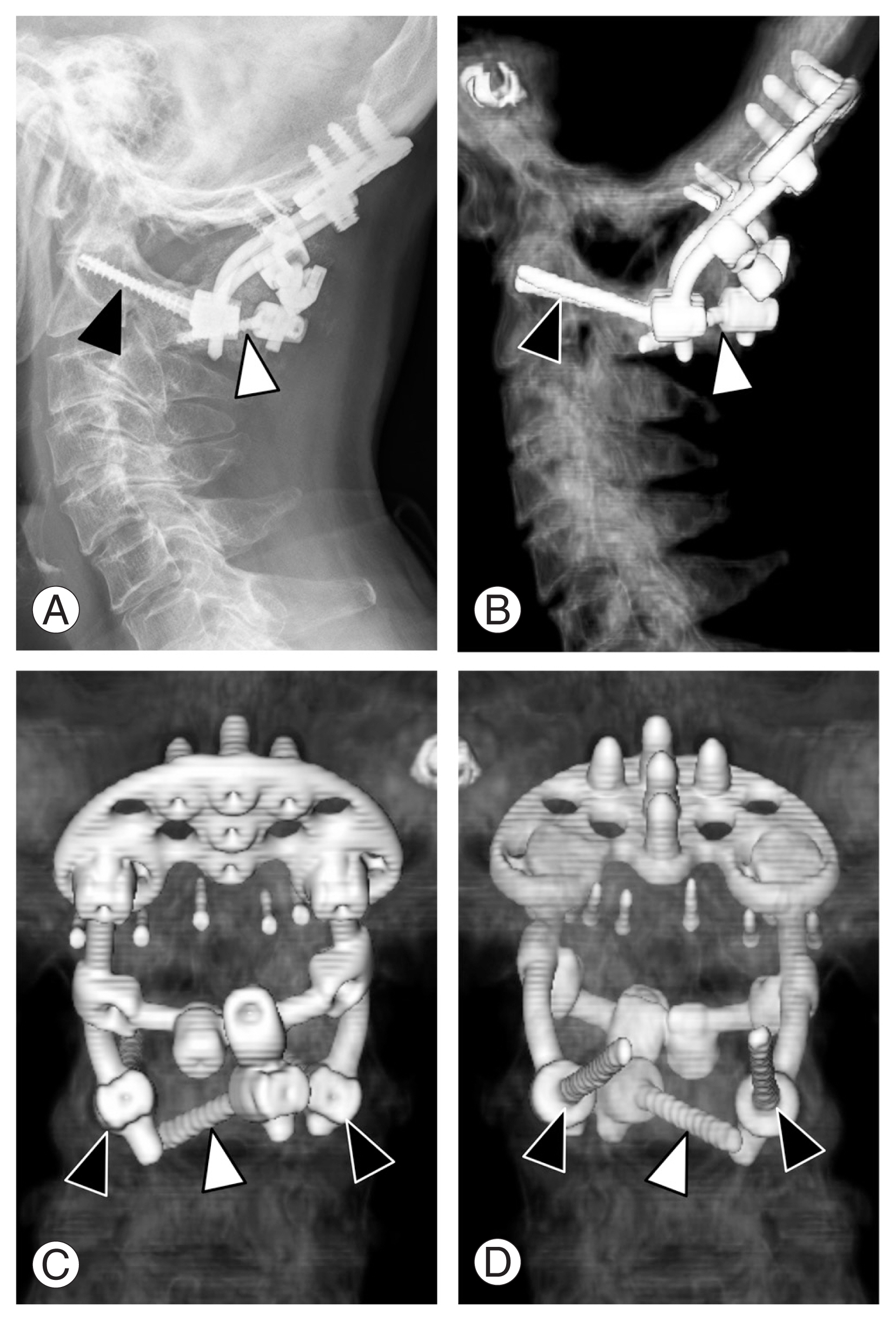
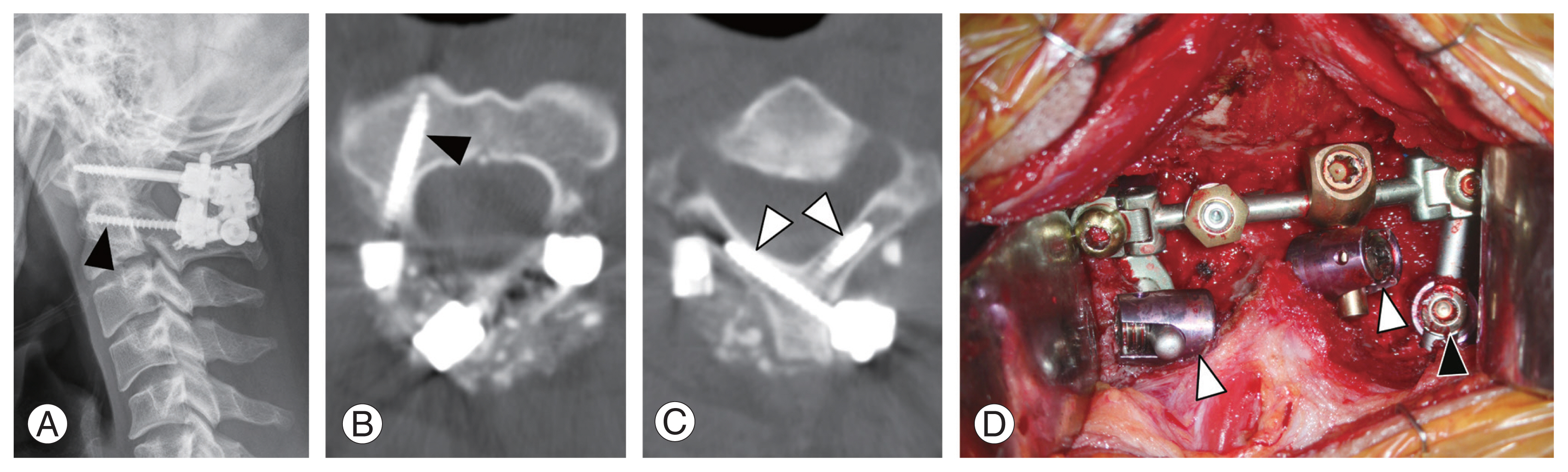
Fig. 2
(A–D) In this case with C1–C2 fusion, a pedicle screw (black arrowhead) and two laminar screws (white arrowheads) were used for C2 fixation.
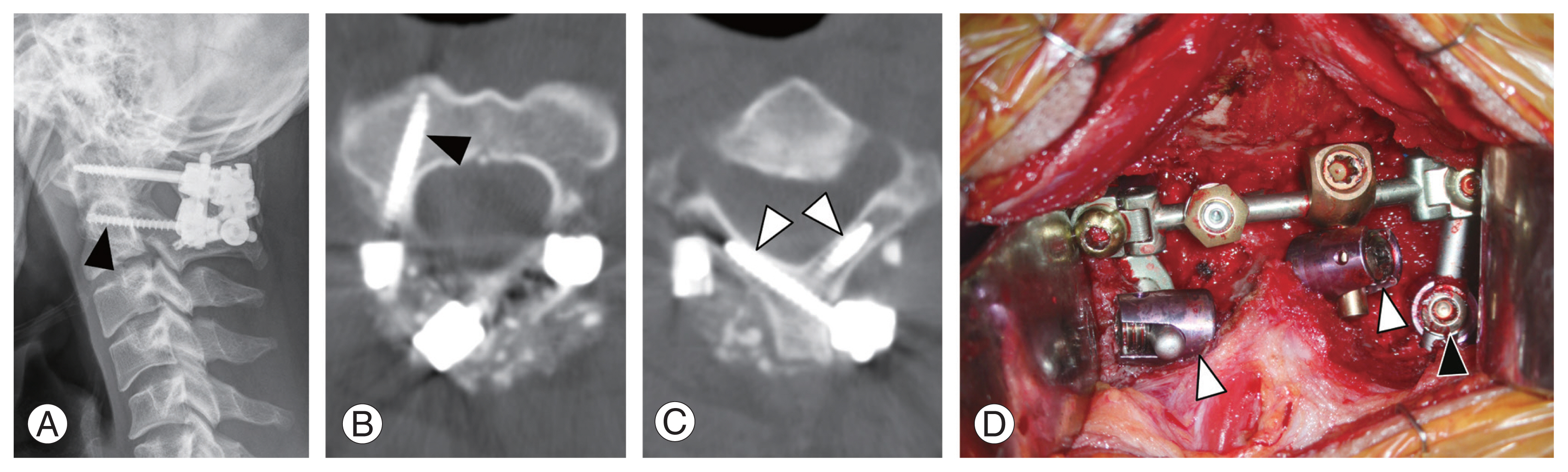
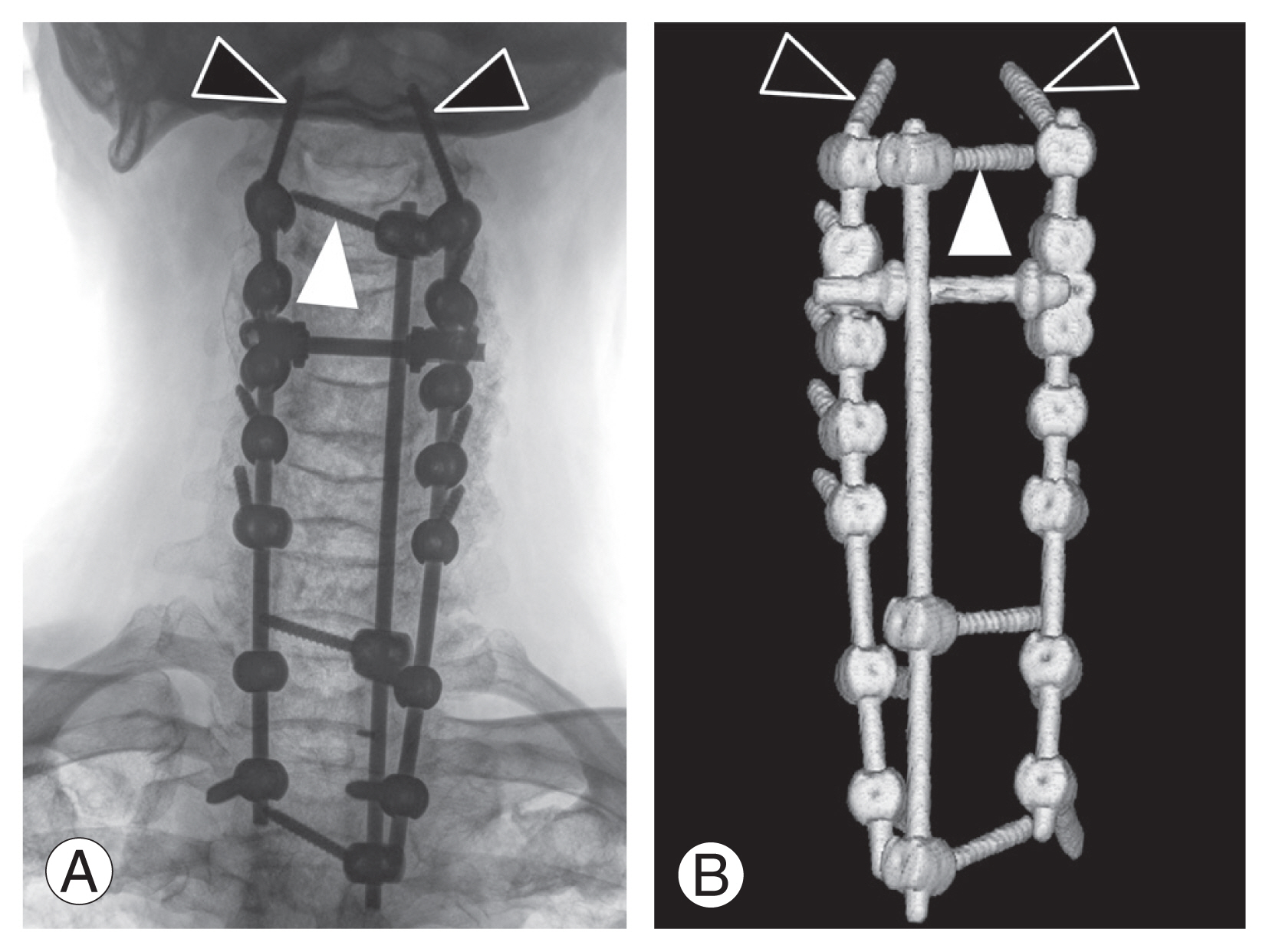
Fig. 3
(A, B) C2–T2 fusion was augmented using a third rod connecting C2, C7, and T2 laminar screws. At C2, two pedicle screws (black arrowheads) and a laminar screw (white arrowhead) were placed.
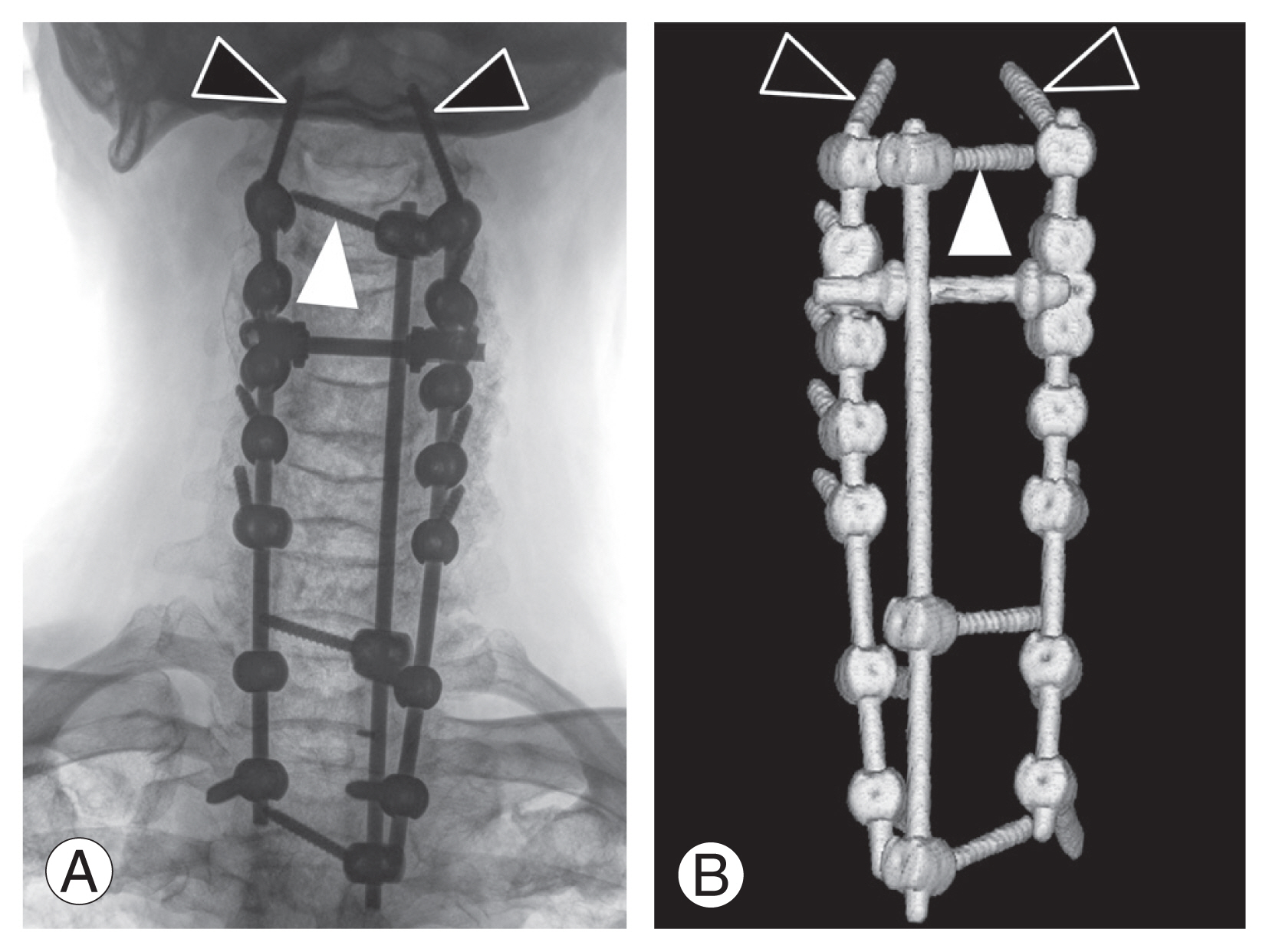
Fig. 4
(A, B) Simulation for the pedicle (black arrowhead) and laminar (white arrowhead) screw placement using three-dimensional simulation software and CT scan images is shown.

Fig. 5
Examples of screw-rod assembly for occipito-cervical fixation (A–C) and for additional fixation for a long fusion (D) are shown.
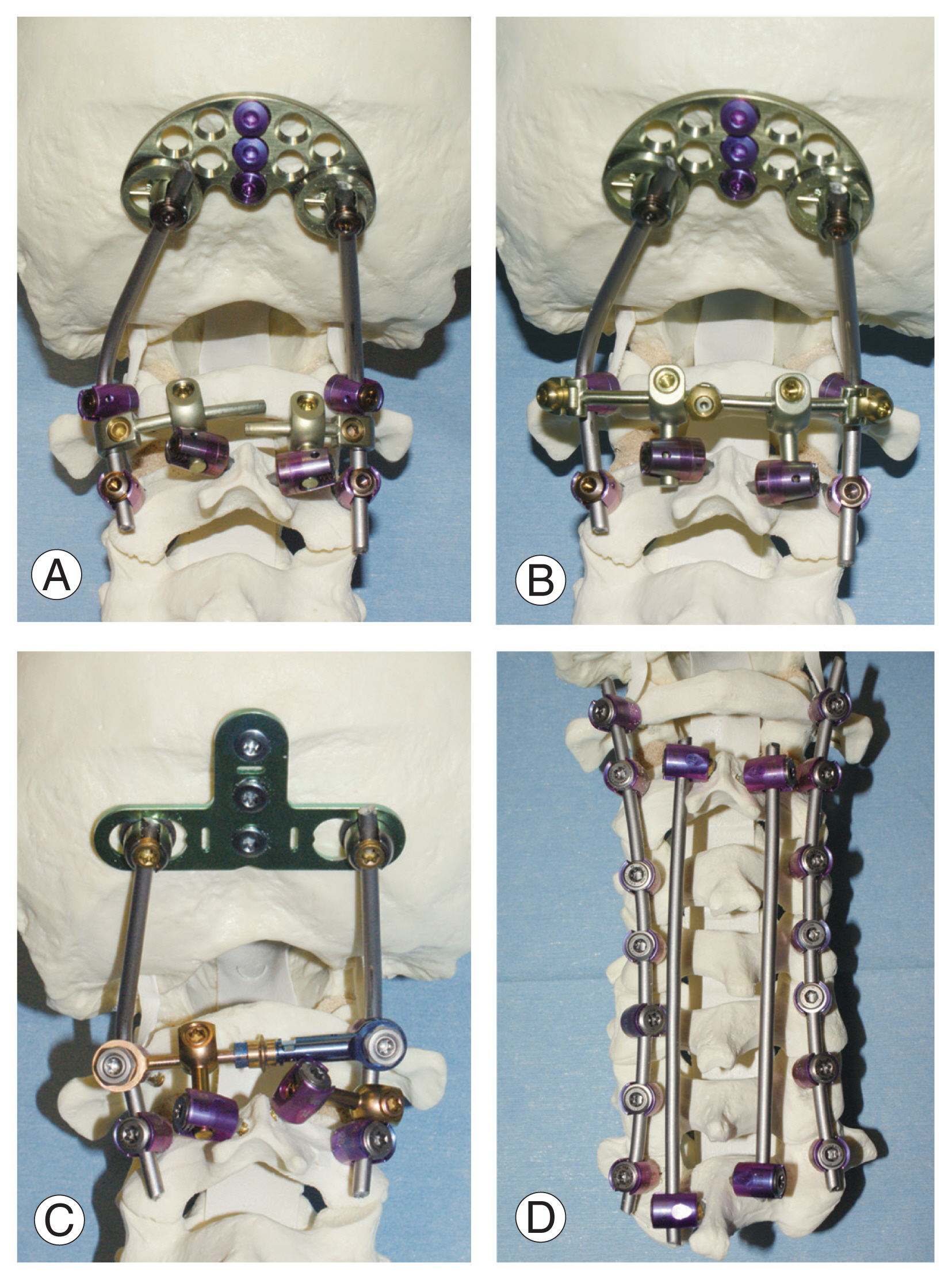
Table 1
Feasibility of 3.5 mm C2 pedicle and laminar screw placement without cortical violation
|
Feasibility |
No. of cases |
|
Men |
Women |
Total |
|
Both screws are feasible bilaterally |
45 |
40 |
85 |
|
Both screws are feasible only unilaterallya)
|
|
|
|
|
2 pedicle and 1 laminar screws are feasible |
1 |
3 |
4 |
|
1 pedicle and 2 laminar screws are feasible |
3 |
4 |
7 |
|
Only 1 screw is feasible on each side |
|
|
1 |
|
1 pedicle screw on each side |
0 |
1 |
|
|
1 laminar screw on each side |
1 |
1 |
2 |
|
1 pedicle screw and 1 laminar screw |
0 |
1 |
1 |
|
Total |
50 |
50 |
100 |
Table 2
Distance between the entry points of ipsilateral laminar and pedicle screws
|
Distance 1a) (n=89)c)
|
Distance 2b) (n=92)c)
|
|
Mean±STD (mm) |
19.0±1.6 |
21.1±3.0 |
|
Maximum (mm) |
21.4 |
28.8 |
|
Minimum (mm) |
16.1 |
16.8 |
References
1. Shiraishi T, Kato M, Yato Y, et al. New techniques for exposure of posterior cervical spine through intermuscular planes and their surgical application. Spine (Phila Pa 1976) 2012;37:E286–96.


2. Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech 2004;17:158–62.

3. Shin SI, Yeom JS, Kim HJ, Chang BS, Lee CK, Riew KD. The feasibility of laminar screw placement in the subaxial spine: analysis using 215 three-dimensional computed tomography scans and simulation software. Spine J 2012;12:577–84.


4. Alfonso Padua MR, Yeom JS, Thong Em H, et al. The Feasibility of Laminar Screw Placement in the Upper Thoracic Spine: Analysis Using 3D-CT Simulation. Spine (Phila Pa 1976) 2013;38:1146–53.

5. Houten JK, Kinon MD, Weinstein GR. 4-Point C2 Fixation for Occipitocervical Fusion: Technical Case Report. World Neurosurg 2021;148:38–43.


9. Formentin C, deAndrade EJ, Maeda FL, Ghizoni E, Tedeschi H, Joaquim AF. Axis screws: results and complications of a large case series. Rev Assoc Med Bras 1992 2019;65:198–203.


10. Yeom JS, Buchowski JM, Park KW, Chang BS, Lee CK, Riew KD. Undetected vertebral artery groove and foramen violations during C1 lateral mass and C2 pedicle screw placement. Spine (Phila Pa 1976) 2008;33:E942–9.


11. Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech 2004;17:158–62.