Immediate Closed Reduction Technique for Cervical Spine Dislocations
Article information
Abstract
Study Design
Retrospective study.
Purpose
This research aimed to assess the clinical outcomes of patients with traumatic cervical spine dislocation who underwent closed reduction employing our approach.
Overview of Literature
Bedside closed reduction is the quickest procedure for repairing traumatic cervical spine dislocations; nevertheless, it also possesses the risk of neurological deterioration.
Methods
For closed reduction, the patient’s head was elevated on a motorized bed, the cervical spine was placed at the midline, traction of 10 kg was applied, the motorized bed was gradually returned to a flat position, the head was lifted off the bed, and the cervical spine was slowly adjusted to a flexed position. The weight of traction was elevated by 5-kg increments until the positional shift was attained. Subsequently, the bed was gradually tilted while traction was applied again to return the cervical spine to the midline position.
Results
Of the 43 cases of cervical spine dislocation, closed reduction was carried out in 40 cases, of which 36 were successful. During repositioning, three patients experienced a temporary worsening of their neck pain and neurological symptoms that enhanced when the cervical spine was flexed. Closed reduction was conducted while the patient was awake; nevertheless, sedation was needed in three cases. Among the 24 patients whose pretreatment paralysis had been characterized by American Spinal Injury Association Impairment Scale (AIS) grades A–C, seven patients (29.2%) demonstrated an enhancement of two or more AIS grades at the last observation.
Conclusions
Our closed reduction approach safely repaired traumatic cervical spine dislocations.
Introduction
High-energy and multiple traumas are commonly complicated by spinal injuries [1–3]. Among them, dislocation of the cervical spine needs aggressive treatment because it may cause the disruption of spinal support and neurological function which reduces the capacity to carry out daily activities. Cervical dislocations that injure the spinal cord and trigger neurological symptoms should be realigned promptly to relieve mechanical pressure on the spinal cord [4–8]. Non-operative closed reduction of cervical spine dislocations by cranial traction is the most immediate treatment [9–12]. Since the closed reduction of cervical spine dislocation may worsen the neurological symptoms resulting from herniated discs and other conditions, it must be securely conducted [13–15]. Conversely, there are presently no detailed reports on the optimal direction and weight of traction, cervical position, and angle for safe nonsurgical reduction of cervical spine dislocations. Direct cranial traction is the first treatment of choice in our hospital to relieve cervical spine dislocations safely and quickly while considering the position of the cervical spine. Here we define an approach for the noninvasive repair of cervical dislocations at Saitama Medical Center, Saitama Medical University and report its clinical outcomes.
Materials and Methods
1. Participants
This was retrospective observational research enrolling consecutive case series of traumatic cervical spine dislocation who underwent immediate closed reduction. The Ethical Committee of the Saitama Medical Center (approval no., 2021-0088) and performed following the ethical standards of our institutional and national research committees and the 1964 Declaration of Helsinki and its subsequent amendments or comparable ethical standards. Written consent was obtained from all patients.
The study included 43 patients with traumatic cervical spine dislocation treated at Saitama Medical Center, Saitama Medical University between April 2010 and December 2016. The closed repair was abandoned in patients whose fracture type made the use of traction unsafe. Closed reduction was followed by posterior cervical fixation with further posterior decompression when deemed essential. The success rate of closed reduction, time from injury to dislocation repair, complications, and recovery from paralysis were assessed. Continuous values are given as the mean±standard deviation.
2. Closed reduction methods
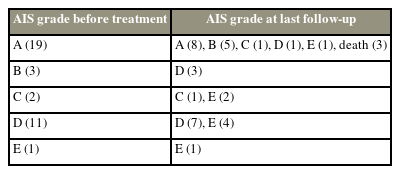
Closed reduction of cervical spine dislocation was carried out in the intensive care unit. The necessary medications and tracheal intubation equipment were prepared for emergency resuscitation, and the technique was carried out while monitoring the electrocardiography and oxygen saturation. The reduction was conducted while the patient was awake. A halo crown (ReSolve Halo System; Össur, Reykjavík, Iceland) was placed on the head while the patient was under local anesthesia in a supine position. A traction frame was positioned on the head of the bed. The following procedure was employed to track the cranium using a halo crown: (1) The patient’s head was raised on a motorized bed, the cervical spine was positioned in the middle position, and traction began at 10 kg irrespective of the patient’s body weight (Fig. 1A). (2) The electric bed was gradually returned to a flat position with the cranium in traction, the head was lifted off the bed, and the cervical spine was slowly shifted to a flexed position (Fig. 1B, C). (3) If the dislocation was not repaired after 2 minutes or 3 minutes of traction, the weight of the traction was increased by increments of 5 kg until repositioning was attained and verified by portable radiography (Fig. 2A–C). A maximum traction of 30 kg was applied. (4) After repositioning, the bed was steadily tilted again with traction to return the cervical spine to the mid position (Fig. 1D). (5) The traction was then slowly released, and plain radiographs of the lateral cervical spine collected in the intensive care unit using portable X-rays verified that the newly acquired position was retained (Fig. 2D).

Our method for closed reduction of cervical spine dislocations. (A) The patient’s head is elevated on a motorized bed, the cervical spine is placed along the midline, and direct traction is applied with a halo crown attached to the skull. (B) As the motorized bed gradually returns to a flat position, the head is lifted off the bed. The cervical spine slowly shifts to a flexed position. (C) The motorized bed is gradually tilted again with traction after repositioning of the cervical spine dislocation. Written informed consent for the publication of this image was obtained from the patient.
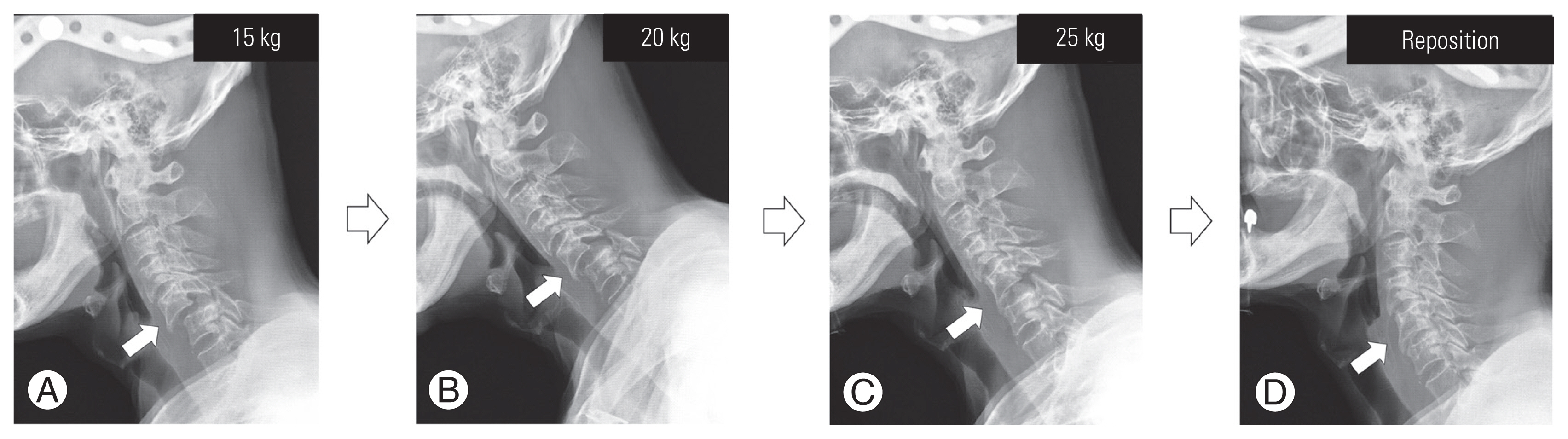
Plain X-ray lateral views of the cervical spine during closed reduction. The arrows on the radiographs indicate the site of cervical spine dislocation. The cervical spine is dislocated at C5–6. (A) The traction load was increased from 10 to 15 kg, but the dislocation was not repaired. (B) The traction load was increased from 15 to 20 kg, and the dislocation was reduced but not yet fully repaired. (C) When the traction load was increased from 20 to 25 kg, the dislocation was repaired. (D) After returning the cervical spine from flexion to the neutral position and releasing traction, the dislocated cervical spine returned to normal alignment.
During traction, the symptoms were monitored, and if observed to be worsening, the traction was lowered, or the cervical flexion angle was modified. Minimal sedation was carried out if muscle tension inhibited the reduction of the dislocation.
3. Treatment following closed reduction
All patients underwent closed reduction followed by posterior cervical fixation. Surgery was conducted through a posterior median incision, and posterior fixation of the dislocation site was carried out. One intervertebral fixation was employed; nevertheless, the range of fixation was extended when a fracture was detected in the intervertebral facet joint.
In cases of paralysis, decompression surgery using open-door laminoplasty was performed. The spinal level of decompression was identified by the extent of spinal cord compression on cervical magnetic resonance imaging (MRI) that was conducted promptly following the reduction of the dislocation. When compression factors such as disc herniation or spinal stenosis were observed, decompression was carried out to the extent that the compression factor was released. In severe cases of paralysis, more extensive decompression was performed, taking into account the swelling of the spinal cord.
Patients with American Spinal Injury Association Impairment Scale (AIS) grades A–C underwent surgery within 24 hours of injury, and patients with grades D or E underwent surgery within a few days.
Results
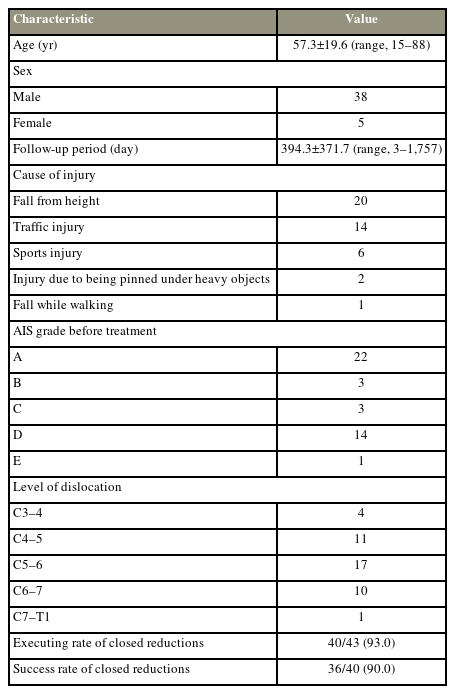
Table 1 summarizes the patients’ demographics. The patient’s average age (38 men, five women) was 57.3±19.6 years (range, 15–88 years). The mean follow-up period was 394.3±371.7 days (range, 3–1,757 days). The follow-up period was short, particularly for patients who died (three patients: 3 days, 130 days, and 141 days). Cause of the injuries comprised 20 falls from heights, 14 traffic accidents, six sports accidents, two being pinned under heavy objects, and one falling while walking. The severity of paralysis was 22, three, three, 14, and one for AIS grades A, B, C, D, and E, respectively. The dislocation sites were C3–4 in four cases, C4–5 in 11 cases, C5–6 in 17 cases, C6–7 in 10 cases, and C7–T1 in one case. In two of the 43 cases, closed reduction was not carried out due to the high instability at the fracture site. In another case, cranial traction could not be performed because of a concomitant skull fracture. The remaining 40 patients underwent preoperative closed reduction with cranial traction, which was successful in 36 patients and failed in four patients. In patients with successful reduction, subsequent MRI demonstrated enhanced spinal canal alignment (Fig. 3A). In patients with failed reduction, subsequent MRI revealed remaining compression of the spinal cord (Fig. 3B). The time from injury to repair of the dislocation was 4.9±2.2 hours (range, 2.0–9.5 hours). The time required for repair was 4.9±2.1 minutes (range, 2.0–9.5 minutes). The time from closed reduction to the initiation of surgery was 8.5±6.8 hours (range, 2.0–21.0 hours) for patients with AIS grades A–C and 16.2±22.9 hours (range, 2.0–69.0 hours) for patients with AIS grades D or E. Adverse events involved one case of halo crown displacement during traction and three cases with worsening neck pain and neurological symptoms during reduction. In the three cases in which symptoms worsened during reduction, the symptoms enhanced when the cervical spine was returned to the flexed position. Sedation was employed in three cases, and the dislocation was successfully repaired in two of them. In the three cases in which sedation was utilized, there was no worsening of paralysis. In 20 patients, spinal cord compression persisted after repair of the dislocation on MRI, and decompression surgery with laminoplasty or laminectomy was carried out. The causes of spinal cord compression in these patients were a herniated disc in seven patients and spinal stenosis owing to bulging ligamentum flavum, mild intervertebral misalignment, or a combination of factors in 13 patients. Table 2 summarizes AIS grade alterations for the 36 patients who underwent successful closed reduction. Time from injury to repair of dislocation was 4.7±2.1 hours (range, 2.0–8.5 hours). Of the patients with AIS grade A, three died during follow-up. Of the 24 patients with pretreatment AIS grades A–C, seven patients (29.2%) portrayed an improvement of two or more grades.
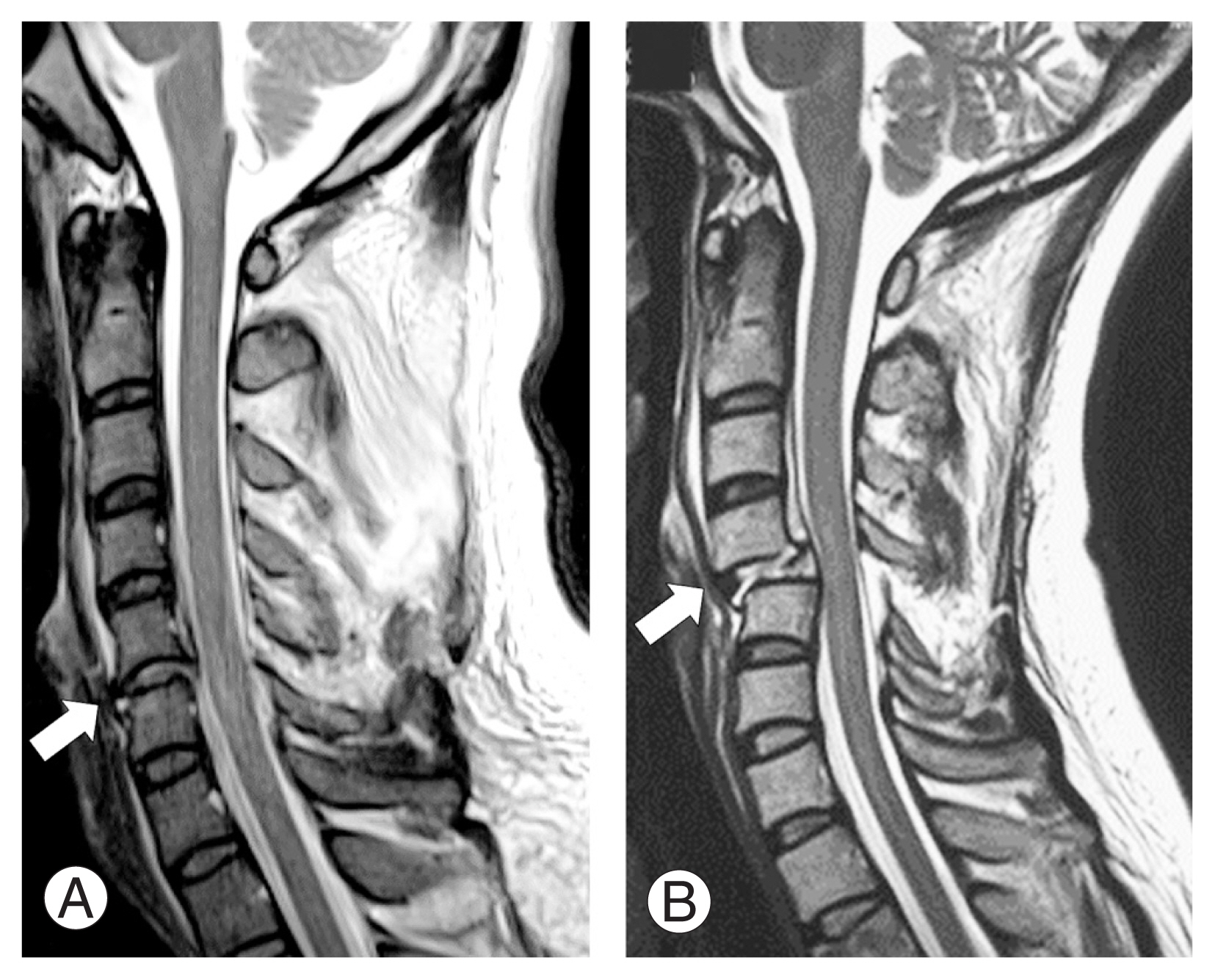
Sagittal T2-weighted images of cervical spine magnetic resonance imaging immediately after closed reduction. The arrows indicate the site of cervical spine dislocation. (A) A case of successful repositioning. Dislocation is well repaired and spinal alignment is improved. (B) A case of poor repositioning. Cervical spine dislocation and spinal cord compression remain.
Discussion
Out of the 43 patients treated for traumatic cervical spine dislocation at our hospital during the study period, 40 underwent preoperative closed reduction with cranial traction, and of these, 36 were treated successfully. Three patients suffered worsening neck pain and neurological symptoms during the reduction procedure; nevertheless, these enhanced when the cervical spine was returned to the flexed position, and the neurological symptoms did not worsen with closed reduction. Among patients who underwent successful closed reduction, 29.2% with pretreatment AIS grades A–C showed an improvement by two or more AIS grades at the last observation.
Severe paralysis following spinal cord injury has been considered to bear a poor functional prognosis because of low improvement. In a prognostic study of 1,436 cervical cord injury patients in the US National Spinal Cord Injury Database, Marino et al. [16] stated that approximately 70% of AIS grade A patients remained of grade A after 1 year, and approximately 7% enhanced to AIS grade D. Recently, however, it has been reported that early decompression of the spinal cord stimulates the improvement of paralysis, and the effectiveness of early decompression has been revealed. Fehlings et al. [17] described that, regarding the timing of decompression of cervical spinal cord injury, significantly more patients (19.8%) improved their AIS score by ≥2 grades in the “earlier” group (treated within 24 hours) than those in the “later” group (8.8%). Chikuda et al. [18] also observed that spinal cord decompression within 24 hours expedited an improvement in motor scores in a randomized clinical trial of cervical spinal cord injury with pretreatment AIS grade C and pre-existing canal stenosis. Badhiwala et al. [6] reported that decompression surgery within 24 hours of spinal cord injury induced the recovery of sensory-motor function, with a head starts at 36 hours. Therefore, in patients with spinal cord compression and neurological symptoms, early decompression may enhance the neurological prognosis. In cervical spine dislocation, the spinal cord is mechanically compressed by the displaced spinal canal, and mending the dislocation can decompress the spinal cord. A systematic review offered reasonable evidence that patients with acute traumatic cervical spinal cord syndrome caused by vertebral fracture, dislocation, traumatic disk herniation, or instability exhibit better outcomes with early surgery (<24 hours) [5]. The closed reduction has the advantage benefit of repairing dislocations earlier than surgery. Newton et al. [19] stated that among eight patients whose cervical spines were dislocated owing to rugby trauma and who had their dislocation repaired by closed reduction within 4 hours, five had a complete recovery from paralysis of Frankel grade A before treatment.
Although closed reduction can accomplish the repair of dislocations faster than surgery, it also possesses the risk of deteriorating neurological symptoms [13–15]. To avoid this, the closed reduction should be conducted with the patient is awake. In this research, three patients experienced worsened neck pain and neurological symptoms during reduction; yet, because the patients were awake, the worsening of the symptoms was detected early, and the symptoms were improved by cervical repositioning. Worsening of the neurological symptoms owing to closed reduction may result from herniated disks, edema of the spinal cord, or tuck of the ligamentum flavum. Wimberley et al. [20] reported that in a case of cervical dislocation with ossification of the posterior longitudinal ligament, the neurological symptoms exacerbated when the cervical spine was returned from flexion to extension following the reduction of dislocation and improved when the cervical spine was returned to flexion again. Sugimoto et al. [21] also described two cases of cervical dislocation with worsening paralysis after posterior fixation, which the authors accredited to the tucking of the yellow ligament owing to extension fixation of the neck. Therefore, in closed reduction, the position of the cervical spine after dislocation has been repositioned must be monitored. If the patient is awake, and the dislocation cannot be repositioned, the next step is the reduction of the dislocation under sedation. There are prior reports of successful closed reduction of cervical spine dislocations under general anesthesia without complications such as worsening neurological symptoms [22,23]. Nevertheless, carrying out closed reduction under sedation bears risks because the neurological symptoms cannot be monitored, and worsening of the symptoms cannot be observed. The dislocation should be immediately repaired surgically, without any further forceful reduction in cases where it cannot be promptly repaired with closed reduction under sedation.
The timing of MRI is also diverse among several studies. Some reports have suggested that MRI should be carried out before reduction to prevent the worsening of neurological symptoms during the reduction of dislocation due to disk herniation [13,15]. Nevertheless, there is little information that can be gotten from MRI before reconstruction, and considering the time needed to acquire an MRI, we believe it is better to repair the dislocation promptly [24]. In this research, MRI was carried out after dislocation repair to assess spinal cord compression lesions and help identify the surgical approach. Vaccaro et al. [25] conducted MRIs before and after closed reduction and discovered disk herniations before the reduction in 18% and after the reduction in 56% of the cases; still, there was no worsening of the neurological symptoms due to repair. Darsaut et al. [26] also carried out MRI before the closed reduction in 17 patients with cervical spine dislocation and reported that 15/17 (88.2%) had ruptured disks and 4/17 (23.5%) had herniated disks. However, the repair did not exacerbate their neurological symptoms, and all patients had these disk abnormalities resolved following the reduction [26]. A previous systematic review also noted that neurological worsening after spinal realignment with cranial-cervical traction was rare [27]. In this research, there were no cases of permanent worsening of the neurological symptoms owing to closed reduction, and we believe that this procedure can be carried out safely. Thus, we prioritize highly prompt dislocation repair, followed by an MRI assessment. Our cranial traction dislocation repair method is simple and safe. Dislocation is repaired by tilting the motorized bed and slowly flexing the cervical spine while applying constant traction. During the reduction using our technique, sustained longitudinal traction on the cervical spine may lower the risk of disk herniation prolapse.
This study has some limitations. The effect of closed reduction on recovery from paralysis is unclear, as there was no comparison made with paralyzed patients who did not receive a closed reduction. As recovery following spinal cord injury differs extensively from patient to patient, large randomized controlled trials are required to depict the effects of acute treatment interventions. Additionally, in this research, surgery was carried out immediately after a closed reduction in paraplegic patients with AIS grades A–C. Moreover, some patients demonstrated clear improvement in paralysis immediately following closed reduction; however, time constraints precluded an accurate assessment of AIS grade immediately after closed reduction. Thus, it was impossible to differentiate the effects of closed reduction from those of surgery. However, this research portrayed that closed reduction of cervical spine dislocations could be carried out safely with our method. More case data are required to verify the safety of our method for repairing cervical spine dislocations.
Conclusions
Closed reduction of cervical spine dislocations employing our research was successful in 36 of 40 patients (90%). In three patients, the symptoms worsened during the repair but were rapidly resolved by returning the cervical spine to flexion. Our technique can safely and promptly repair cervical spine dislocations.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
All authors contributed to the study design, data collection, data interpretation, and critical revision of the manuscript.