Preoperative Low Back Pain Affects Postoperative Patient Satisfaction Following Minimally Invasive Transforaminal Lumbar Interbody Fusion Surgery
Article information
Abstract
Study Design
A single-center retrospective study.
Purpose
To research the predictive factors associated with postoperative patient satisfaction 1 year after minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF), a minimally invasive procedure for lumbar degenerative disease.
Overview of Literature
There have been reports of numerous variables influencing patient satisfaction with lumbar surgery; however, there have been few investigations on MIS are limited.
Methods
This study included 229 patients (107 men and 122 women; mean age, 68.9 years) who received one or two levels of MIS-TLIF, and the patient’s age, gender, disease, paralysis, preoperative physical functions, duration of symptom(s), and surgery-associated factors (waiting for surgery, number of surgical levels, surgical time, and intraoperative blood loss) were studied. Radiographic characteristics and clinical outcomes such as Oswestry Disability Index (ODI) scores and Visual Analog Scale (VAS; 0–100) ODI scores for low back pain, leg pain, and numbness were studied. One year following surgery, patient satisfaction (defined as satisfaction for surgery and for present condition; 0–100) was assessed using VAS and its relationships with investigation factors were examined.
Results
The mean VAS scores of satisfaction for surgery and for present condition were 88.6 and 84.2, respectively. The results of multiple regression analysis showed that preoperative adverse factors of satisfaction for surgery were being elderly (β=−0.17, p=0.023), high preoperative low back pain VAS scores (β=−0.15, p=0.020), and postoperative adverse factors were high postoperative ODI scores (β=−0.43, p<0.001). In addition, the preoperative adverse factor of satisfaction for present condition was high preoperative low back pain VAS scores (β=−0.21, p=0.002), and postoperative adverse factors were high postoperative ODI scores (β=−0.45, p<0.001) and high postoperative low back pain VAS scores (β=−0.26, p=0.001).
Conclusions
According to this study, significant preoperative low back pain and high postoperative ODI score after surgery are linked to patient unhappiness.
Introduction
Leg pain, back or buttock pain, and walking ability are predicted to improve temporarily or permanently after lumbar degenerative disease surgery [1]. Recently, Numerous minimally invasive surgeries (MISs) have been reported [2]. Specifically, Foley et al. [2] described MIS transforaminal lumbar interbody fusion (MIS-TLIF) approach, using a muscle-splitting strategy as an alternate surgery to the traditional open approach, which minimizes tissue injury, muscle retraction, and skin incisions. The risks connected with open lumbar spinal fusion surgery are also decreased by MIS-TLIF [3–5]. MIS-TLIF was found to have reduced intraoperative blood loss, immediate postoperative pain, hospitalization stay, and infection rate when compared to open TLIF [3–5]. At 6 months, 12 months, and 36 months postoperatively following surgery, MIS-TLIF patients reported less back pain and higher Oswestry Disability Index (ODI) ratings than open TLIF patients [6]. Thus, many studies have reported favorable results for MIS-TLIF surgery.
Patient satisfaction has been a commonly used outcome criterion and is regarded as an important complementary measure of healthcare quality [7]. The factors that affect patient satisfaction after spine surgery are probably complex and not always linked to reductions in leg or back pain and improvement of walking ability. The patient’s preoperative expectations, psychological distress, preoperative health, obesity, spinal canal shape, and other intrinsic patient characteristics, on the other hand, may have an impact on patient satisfaction [8–11]. The majority of patients who underwent surgery to cure central spinal stenosis say they are happy with the results [11,12]. However, nearly one-third of patients undergoing surgery for lumbar degenerative disorders reported being unhappy with the surgery and its postoperative clinical results [13]. Therefore, it is critical to identify the reasons behind patients’ discontent with MIS-TLIF [3–6]. However, the surgical techniques mentioned in numerous research pertaining to patient satisfaction are frequently inconsistent, and only a small number of studies have focused solely on MIS-TLIF alone. The purpose of this study was to investigate the prognostic factors that affect short-term postoperative satisfaction with MIS-TLIF.
Materials and Methods
1. Study design
We followed the guidelines of the Declaration of Helsinki when conducting this study. The Institutional Review Board (IRB) of Anshin Hospital examined and approved the study’s protocol (IRB approval no., 116). Patients expressed their agreement after being informed that their data will be utilized for clinical research. We looked back at prospectively gathered data on patients who underwent primary MIS-TLIF from the database of Anshin Hospital between March 2017 and June 2018 with a minimum 1-year follow-up. Patients who had undergone prior spine surgery on the surgical level were not included. Additionally, we disregarded reoperation cases within a year after surgery because of disorder in the same segment or adjacent segment. The target diseases were lumbar degenerative diseases, including lumbar disc herniation (LDH), lumbar spinal stenosis (LSS) with lumbar degenerative spondylolisthesis (DS), LSS without DS, and ischemic spondylolisthesis (IS). There were either one or two-level that were operational. If a patient responded to the satisfaction survey 1 year after surgery as a respondent.
Four cases of the 243 patients who underwent MIS-TLIF for lumbar degenerative disease, required reoperation within a year due to adjacent segment disease (ASD). and 10 cases had missing values in the investigation factors or could not be followed up for a year. Finally, this study examined 229 cases.
2. Surgery
Prior to surgery, all patients completed at least 3 months of nonsurgical, conservative treatment, including medication, physical therapy, and pain block. After the conservative treatment course of treatment failed, surgical surgery was explored. The indication for MIS-TLIF was meeting one of the following conditions: (1) LSS with Meyerding classification grade 1 or 2 DS and IS; (2) LSS or LDH with severe intervertebral disc degeneration; and (3) LSS with foraminal stenosis [14]. The surgery was performed in 85 single institution by two senior surgeons. General anesthesia was used to position the patients in the prone position while preoperatively marking was carried out with an image intensifier. The surgeon stood on the more symptomatic side, and an approximate 3 cm incision was made at the level of the facet joint to be resected. A 26 mm tubular retractor was used to bluntly slice the soft tissue to see the facet joint complex. The inferior facet was removed using a high-speed burr after the facet capsule was opened. Then, the superior facet is resected from the tip to the superior border of the pedicle. After that, the ligamentum flavum was resected from the cartilage lateral to the medial side to expose the disc within the foramen. The ligamentum flavum was removed, exposing the disc to the spinal canal floor. Then, the nucleus pulposus and cartilage endplates were completely removed to expose the bony endplates. The anterior portion of the discectomy space was then filled with the morselized bone transplant. One of two structural implants of the proper size was impressed into the discectomy space and then filled with an extra bone graft. When necessary, the contralateral ligamentum flavum was resected to expose the exiting and traversing nerve roots. The slip was then rectified as necessary using the percutaneous pedicle screws (PPS) system before instrumentations, including PPS and rods, were introduced. The rods were then tightened using the set screws.
On the day after surgery, patients were allowed to get out of bed for postoperative rehabilitation, and the epidural drainage tube was removed 2 days later. Patients wore a rigid corset for 2 months and underwent supervised physical treatment by trained physiotherapists.
3. Collection of patient demographic data
Information was got from medical records, intraoperative notes, and radiographs. Patient demographics included age, sex, body mass index, smoking history (Brinkman index ≥400), comorbidities including diabetes mellitus, hypertension and cancer (limited to patients without spinal metastases), occupation status, disease (LSS without DS or LDH, LSS with DS, IS), the type of neurologic sympatoms (cauda equina syndrome, mixed type, radiculopathy), paralysis (manual muscle testing of any lower limb ≤3), preoperative physical role evaluation (10 m walking time and knee extension muscle strength), and duration of symptom(s). Other surgical-related factors included waiting for surgery, the number of surgical levels, surgical time, and intraoperative blood loss preoperative epidural and selective nerve root block history.
4. Clinical outcomes and radiographic measurements
For clinical results, we assessed ODI scores and Visual Analog Scale (VAS) scores for low back pain, leg pain, and numbness prior to surgery and 1 year afterward. (VAS is graded as ‘0’ for no pain or numbness to ‘100’ points for maximal pain or numbness.) We assessed pelvic incidence minus lumbar lordosis (PI–LL) and pelvic tilt (PT) as radiographic parameters both before and a year after surgery [15]. Using computed tomography scans, we also looked at how often bones fuse within a year. To binarize the factors, we defined the cut-off value of the duration of symptoms and waiting for surgery as 20 months and 36 days respectively using the median value. Based on the findings of Schwab et al. [15], we also established the cut-off values of PI–LL and PT as 10° and 20°, respectively.
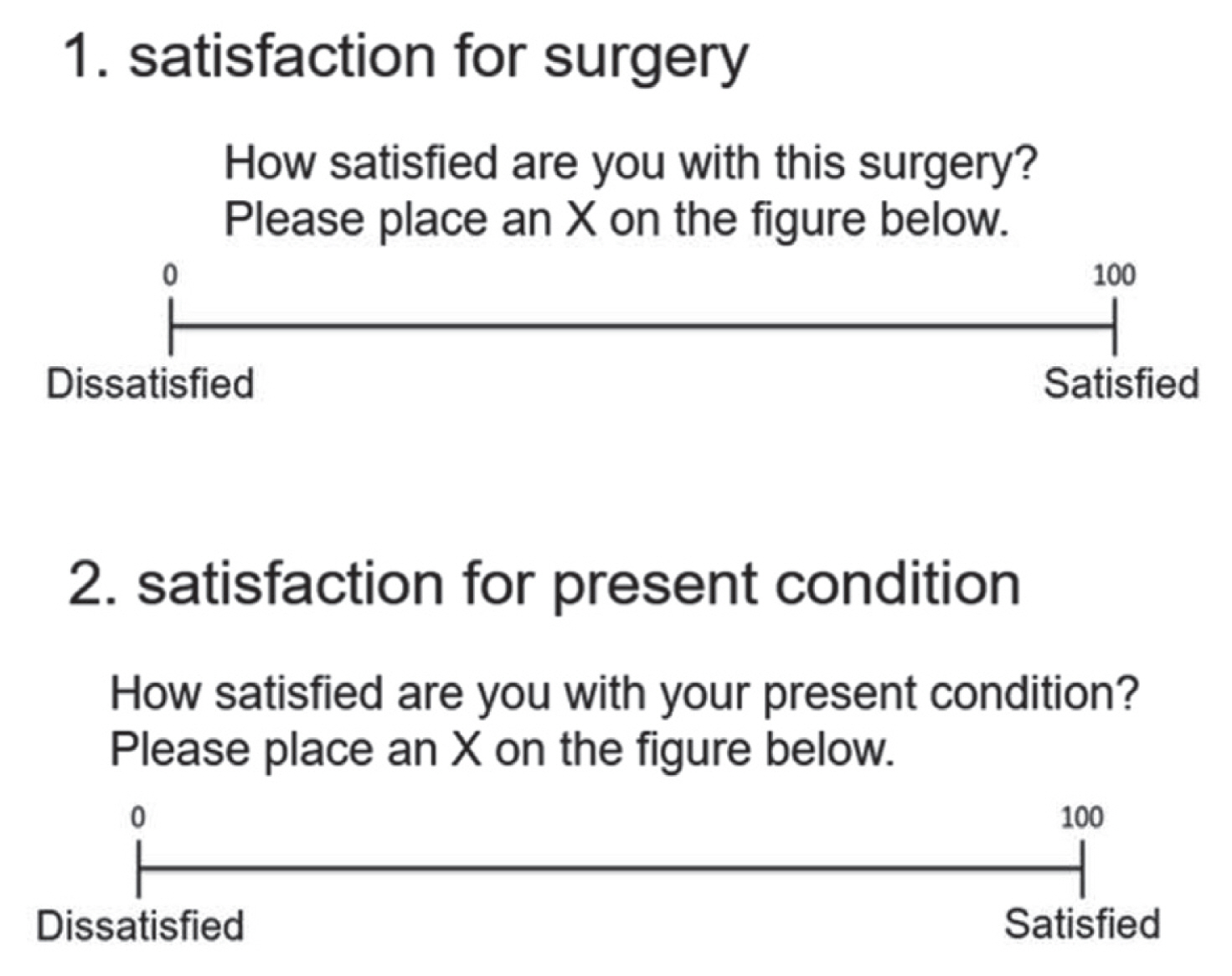
Postoperative satisfaction was assessed using the VAS scores (rated from ‘0’ for unsatisfied to ‘100’ for highly satisfied) 1 year after surgery. The following two criteria were assessed for patient satisfaction scores: satisfaction for surgery and satisfaction for present condition (Fig. 1).
5. Statistical analysis
Using the statistical analysis program IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA), the gathered data were examined. The mean±standard deviation of the data is displayed. The paired t-test was used in statistical analysis to compare preoperative and postoperative ODI scores, as well as VAS scores for low back pain, leg pain, and numbness. In addition, utilizing the Mann-Whitney U test for binary data, the Kruskal-Wallis test for ternary variables, and simple linear regression analysis for continuous variables the correlations between each investigation element and postoperative patient satisfaction were separately examined. The factors with major differences (p<0.05) were divided into preoperative and perioperative factors and postoperative factors, and independent factors impacting postoperative patient satisfaction were examined separately using multiple regression analysis. All statistical tests were two-sided. Statistical significance was evaluated as p<0.05.
Results
1. Patients
There were 107 male and 122 female patients, and the average patient age at surgery was 68.9 years (range, 43–85 years). Thirteen patients had IS, 61 patients had LSS without DS, and 155 patients had LSS with DS The follow-up rate was 95.8%.
2. Clinical outcome measures
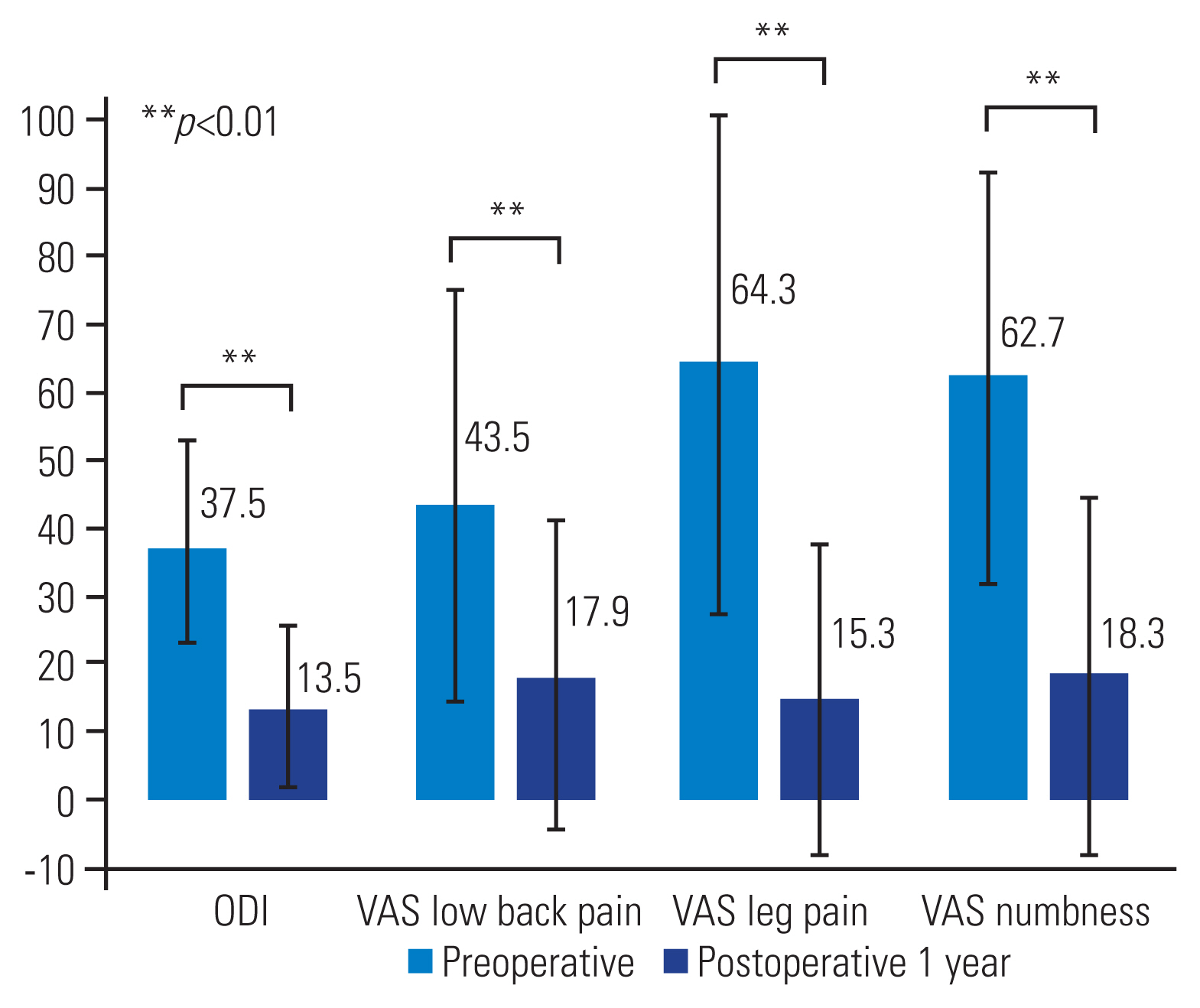
ODI scores and VAS scores for low back pain, leg pain, and numbness showed noteworthy improvement from preoperative to a year after surgery scores, respectively (ODI: 37.5±15.5 → 13.5±12.5; low back pain VAS: 43.5±30.4 → 17.9±22.6; leg pain VAS: 64.3±37.5 → 15.3±22.3; numbness VAS: 62.7±29.0 → 18.3±26.6; all p<0.001) (Fig. 2).
3. Comparison of satisfaction Visual Analog Scale scores for investigation factors
The mean satisfaction VAS score for surgery was 88.6±16.6 and the mean satisfaction VAS score for present condition was 84.2±19.5. Analyzing the relationships between each investigation factor for binary and ternary variables and satisfaction, the factors that showed a statistically significant difference for poor satisfaction for surgery were being elderly (p=0.008), two-level surgery (p=0.041), unemployment (p=0.011), high preoperative low back pain VAS score (p=0.015), and postoperative PT≥20° (p=0.017). However, preoperative PI–LL and PT and postoperative PI–LL were not significantly correlated with satisfaction for surgery. Bone union rates were also not significantly correlated with satisfaction for surgery. For satisfaction for present condition, being elderly (p=0.010), female (p=0.030), unemployment (p=0.009), and high preoperative low back pain VAS score (p=0.019) showed significant difference for poor satisfaction for present condition. Pre- and postoperative PI–LL and PT were not significantly correlated with satisfaction for present condition. Bone union rates were similarly not significantly correlated with satisfaction for present condition (Table 1).
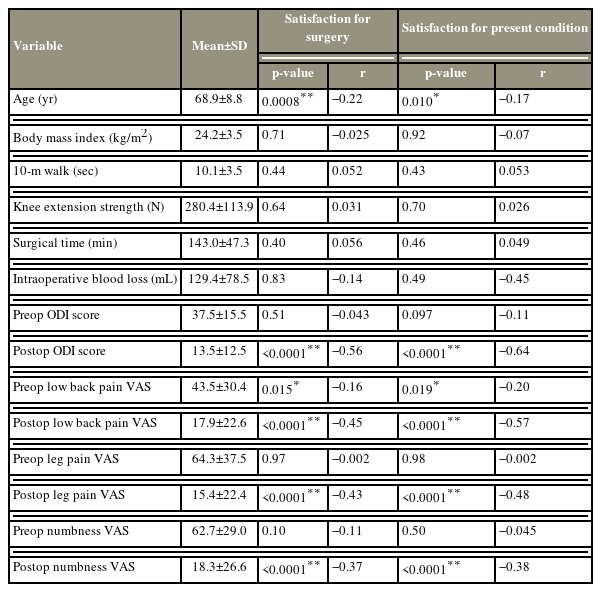
Analyzing the relationships between each investigation factor of continuous variables and satisfaction, the factors that showed a statistically significant correlation with poor satisfaction for surgery were high postoperative ODI scores (p<0.0001) and high postoperative low back pain, leg pain, and numbness VAS scores (p<0.0001, p<0.0001, p<0.0001, respectively). For satisfaction for present condition, high postoperative ODI scores (p<0.0001) and high postoperative low back pain, leg pain, and numbness VAS scores (p<0.0001, p<0.0001, p<0.0001, respectively) showed a significant correlation with poor satisfaction for present condition. Intraoperative factors such as blood loss and surgical time were not significantly correlated with postoperative satisfaction (Table 2).
In addition, a single linear regression analysis showed that satisfaction for surgery had significant moderate negative correlations with postoperative ODI scores, postoperative low back pain and leg pain VAS scores (r=−0.56, r= −0.45, r=−0.43, respectively) and significant weak negative correlations were observed with age, and preoperative low back pain and postoperative numbness VAS scores (r=−0.22, r=−0.16, r=−0.37, respectively). The satisfaction for present condition had moderate negative correlations with postoperative ODI scores, and postoperative low back pain and leg pain VAS scores (r=−0.64, r=−0.57, r=−0.48, respectively), and significant weak negative correlations were observed with preoperative low back pain and postoperative numbness VAS scores (r=−0.20, r=−0.38, respectively) (Fig. 3).
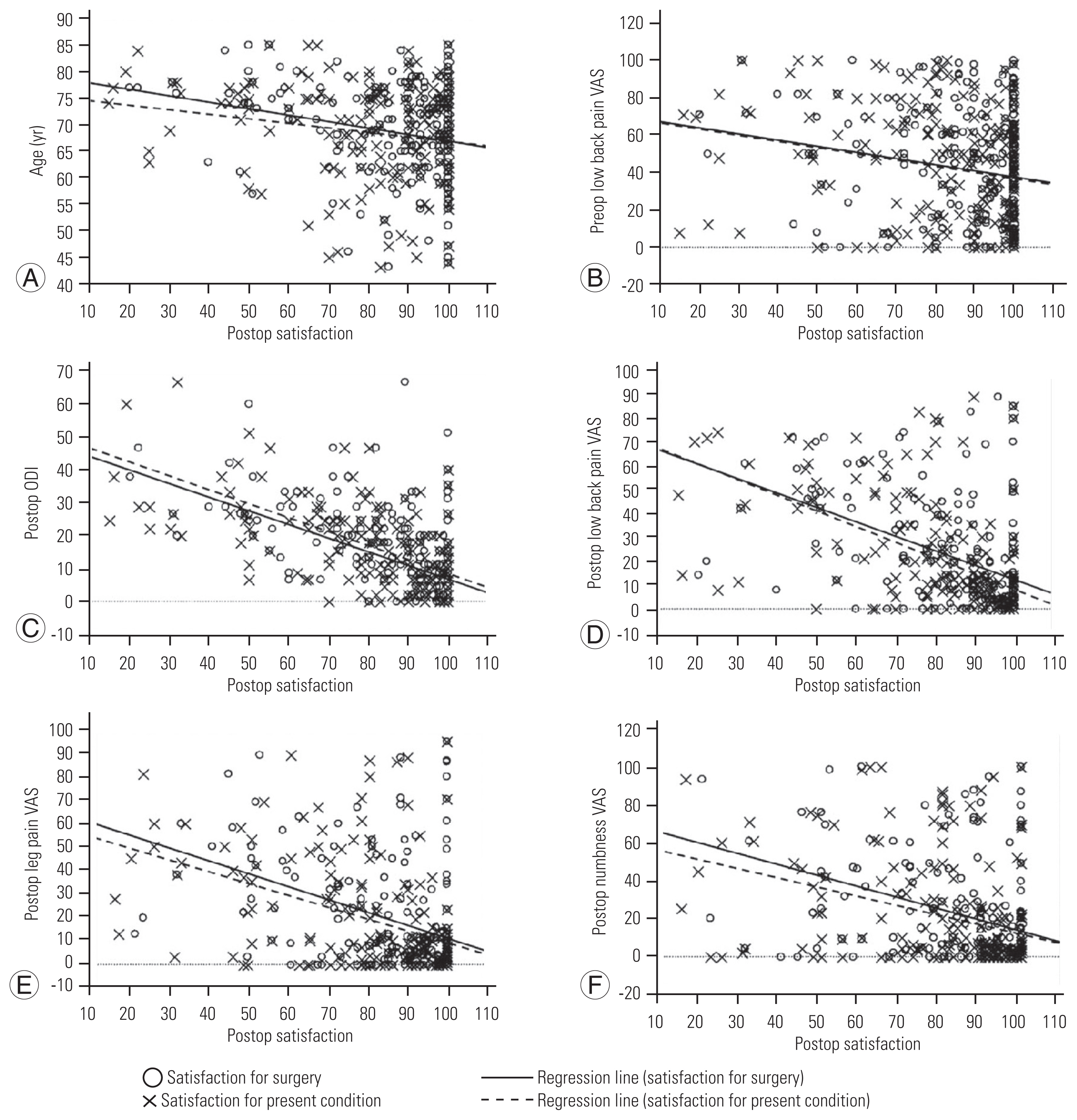
Simple regression analysis of continuous variables and patient satisfaction. (A–F) These six graphs show significant negative correlations with patient satisfaction (both satisfaction for surgery and satisfaction for present condition). Preop, preoperative; Postop, postoperative; VAS, Visual Analog Scale; ODI, Oswestry Disability Index.
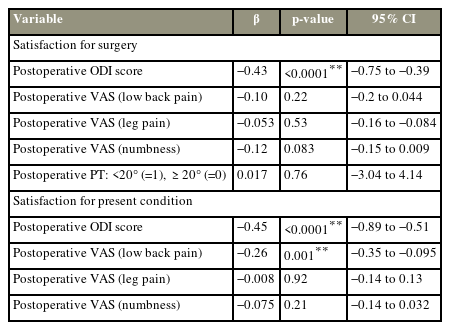
4. Multiple regression analysis for preoperative, intraoperative, and postoperative factors
The above factors with statistically significant differences (p<0.05) were divided into preoperative and intraoperative factors and postoperative factors, and multiple regression analyses were individually performed. As a result, the preoperative poor factors of satisfaction for surgery were being elderly (β=−0.17, p=0.023) and high preoperative low back pain VAS scores (β=−0.15, p=0.020) (Table 3), and the postoperative poor factor of satisfaction for surgery was high postoperative ODI scores (β=−0.43, p<0.001). The preoperative poor factors of satisfaction for present condition were high preoperative low back pain VAS scores (β=−0.21, p=0.002), and the postoperative poor factors of satisfaction for present condition were high postoperative ODI scores (β=−0.45, p<0.001) and high postoperative low back pain VAS scores (β=−0.26, p=0.001) (Table 4). As a result, the independent factors affecting patient dissatisfaction were preoperative high low back pain VAS scores and high postoperative ODI scores.
5. Complications
In this investigation, intraoperative complications were not noted. Four patients who were not included in the study had postoperative complications. For ASD, revision surgery was necessary for all four patients required. There were no implant failures requiring additional surgery, postoperative epidural hematomas, or surgical site infections. A year following revision surgery, three out of four patients can be monitored. One year after revision surgery, two patients had good postoperative outcomes (mean satisfaction for surgery, 90; for present condition, 84), whereas one patient had a poor postoperative outcome (satisfaction for surgery, 65; for present condition, 48).
Discussion
According to this study, ODI and VAS (low back pain, leg pain, and numbness) scores, showed considerable symptom and function improvements following MIS-TLIF surgery, as well as high postoperative satisfaction rates. In addition, the study’s most important findings were that low back pain prior to surgery and postoperative high ODI scores were independent factors that negatively impacted both surgical satisfaction for surgery and satisfaction for present condition 1 year after MIS-TLIF.
The predictors of patient satisfaction with surgery for lumbar degenerative disease have been the subject of several research. According to Lim et al. [16], the only significant predictor of postoperative patient satisfaction with TLIF surgery was preoperative leg pain. Smoking, long duration of leg pain, and malignant and neurological symptoms were all linked to patient unhappiness after decompression surgery for LSS according to Paulsen et al. [17]. A significant Swedish study found that factors decreasing postoperative satisfaction for central spinal stenosis were previous spine surgery, smoking, unemployment, long-term back pain, and back pain predominance [18]; in contrast to other reports, smoking, the length or kind of the symptom, paralysis, unemployment, or the time spent waiting for the surgery had no appreciable impact on postoperative satisfaction. However, despite significant improvement in low back pain, leg pain, and numbness, our key finding was that severe preoperative low back pain was linked to patient satisfaction.
It is critical to identify tissue such as the intervertebral disc, facet or sacroiliac joints, myofascial tissues, nerve roots, and ligaments from which the low back pain is coming. Degenerative alternations in these tissues are a major contributor to many occurrences of low back pain because the spine includes several joints [18]. Lumbar fusion surgery may therefore reduce discopathy and facet joint pain at the surgical level, but it is unlikely to alleviate symptoms brought by other tissues. In addition, Waddell et al. [19] observed that psychological factors play a role in the persistence of back pain and the outcome of back pain treatment. Since several criteria are only marginally improved by surgical intervention, it should be possible to increase patient satisfaction by focusing on reducing low back pain prior to surgery. Specifically, physiotherapy and exercise therapy are effective for symptoms caused by myofascial tissues, and the effectiveness of psycho-behavioral approaches, such as cognitive behavioral therapy, has been reported for psychosocial factors [20].
Additionally, Henrotin et al. [21] demonstrated patient knowledge and understanding of their illness can be improved by back pain education using booklets. To help patients comprehend the surgical technique and postoperative course of MIS-TLIF when we get surgical informed consent, our hospital has developed a film about them. Creating booklets about detailed surgical procedures and postoperative courses may be effective because they can be consulted by the patients as many times as they want. We think that by combining preoperative therapies with surgical care in a multidisciplinary manner preoperative low back discomfort may be reduced, and improve patient satisfaction.
Postoperative satisfaction may be closely tied to a patient’s expectations for surgery, which are unrelated to age, sex, marital status, or ethnicity [22,23]. The prevailing consensus is that better postoperative outcomes result from higher preoperative expectations [24]. Gepstein et al. [25] noted that older patients frequently have high preoperative expectations, which might cause a mismatch between the postoperative state and lower satisfaction. According to the study’s findings, getting older was an independent factor in patients’ low satisfaction with their surgery. The authors advise that in order to close the gap between expectations and postoperative outcomes and increase patient satisfaction, more precise information regarding surgical outcomes should be provided before surgery.
Sagittal spinal alignment has been increasingly important in recent years, for lumbar degenerative disorders [26]. LSS causes low back pain, leg pain, neurogenic intermittent claudication, bladder, and rectal disorders, all of which have an impact on one’s quality of life (QOL) in terms of health (health-related quality of life [HRQOL]). One of the most popular surgical procedures for LSS is MIS-TLIF, which typically reduces neurogenic claudication, leg pain, and, eventually, QOL. Studies have demonstrated a correlation between pain, function loss, and low HRQOL and high sagittal vertical axis (SVA) values, high PT, or high PI–LL are correlated with pain, loss of function, and poor HRQOL [27]. Preoperative PT and PI–LL were not connected with patient satisfaction in our investigation, despite the fact that SVA was not evaluated in all patients and hence could not be included in the survey. To put it another way, even while pelvic retroversion, and loss of lumbar lordosis were seen in lumbar degenerative patients before surgery, they would not have an impact on pre-or postoperative patient satisfaction at least not in the near term.
It is thought that the finding that postoperative ODI scores had an impact on postoperative satisfaction reflects the features of ODI, a patient-based evaluation method. The ODI is great because it may assess social loss, pain, and physical dysfunction, including leg pain, in addition to low back pain [28,29]. The results of this study showed that the ODI is a reliable indicator of patient satisfaction as well as a clinical evaluation index.
In this research, we assessed two parameters of postoperative patient satisfaction, satisfaction for surgery, and satisfaction for present condition. Patients frequently give more thought to their current health and symptoms when questioned about their postoperative satisfaction, than on how their symptoms changed as a result of the procedure. Therefore, to evaluate patient satisfaction in more detail, patients were asked separately for satisfaction for surgery and satisfaction for present condition. The questionnaire was gathered by the physiotherapist in order to conduct a less biased satisfaction assessment since when the surgeon evaluates patient satisfaction, patients may claim more pleasure than they truly perceive [30].
The study’s limitations include the inability to analyze variables such as education level, preoperative expectations, and psychological distress that are thought to affect patient satisfaction [8–10]. In addition, other assessments of the quality of life connected to health that may impact patient satisfaction were not looked into in this study. Furthermore, we only used 1-year outcome scores because this study was a pilot study to evaluate predictive characteristics linked to patient satisfaction. Therefore, we intend to keep tracking these patients prospectively to see if these features will hold over a longer period.
Conclusions
According to the study findings, poor postoperative patient satisfaction is linked to severe preoperative low back pain. The findings imply that initiatives to lessen low back discomfort before surgery can enhance postoperative patient satisfaction.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Study design: YH, SM, KT; data correction: SI, MR; interpretation of data: KK, TY; supervision: KK, TY; drafting of the manuscript: YH, SM; and all authors reviewed the manuscript.