 |
 |
- Search
| Asian Spine J > Volume 17(4); 2023 > Article |
|
Abstract
Purpose
To understand the prevalence of persistent orthostatic hypotension (POH), as well as its risk factors and cardiovascular pathology, in patients receiving surgery for the adult spinal deformity (ASD).
Overview of Literature
Although reports of the incidence of and risk factors for POH in different spinal disorders have recently been published, we are not aware of the comprehensive evaluation of POH following surgery for ASD.
Methods
We examined medical records from a single central database for 65 patients receiving surgical treatment for ASD. Statistical comparisons were made between patients who experienced postoperative POH and those who did not, by examining patient and operative characteristics, such as age, sex, comorbidities, functional status, preoperative neurological function, vertebral fractures, three-column osteotomy, total operative time, estimated blood loss, length of stay, and radiographic parameters. The determinants of POH were assessed using multiple logistic regression.
Results
We showed that postoperative POH was a complication of ASD surgery, with a 9% incidence rate. Patients with POH were statistically considerably more likely to require supported walkers due to partial paralysis and to have comorbidities including diabetes and neurodegenerative disease (ND). Furthermore, ND was an independent risk factor for postoperative POH (odds ratio, 4.073; 95% confidence interval, 1.094–8.362; p=0.020). Moreover, perioperative evaluation of the inferior vena cava showed that patients with postoperative POH had preoperative congestive heart failure and had hypovolemia lower postoperative diameter of the inferior vena cava than patients without POH.
Adult spinal deformity (ASD) is widespread; its prevalence was approximately 70% in one healthy, older adult population [1]. Surgical treatment of ASD is related to major complications, which can lead to deterioration of health-related quality-of-life results [2]; perioperative complication rates in older patients treated for ASD range from 37% to 71% [3,4]. Inadequate neurological function [5], proximal and distal junctional failure [6], and medical consequences such as pneumonia] are examples of such issues [7]. However, to our knowledge, there has been no thorough evaluation of postoperative persistent orthostatic hypotension (POH) among patients surgically treated for ASD.
POH is defined as a persistent (a week or longer) decrease in systolic blood pressure (BP) of at least 20 mm Hg or a decrease in diastolic BP of at least 10 mm Hg within 3 minutes of testing while standing up or on a tilt table without noticeably low hemoglobin levels [8]. Patients may have related symptoms in the form of orthostatic intolerance, although such is not necessary for diagnosis. POH is a typical postoperative phenomenon in different surgical disciplines [9]. Among spinal diseases, POH is related to spinal cord injury [10], cervical, dorsal hemangioblastomas [11], and cervical myelopathy [12]. Symptomatic POH can be distressing to patients with ASD and limit their participation in postoperative rehabilitation, potentially delaying their recovery after surgery. This study sought to identify the prevalence of POH following ASD surgery, as well as its risk variables and cardiovascular pathology.
After obtaining the institutional review board’s approval, all patients who had received surgery for ASD with fusion at more than five levels from 2016 to 2021 were shortlisted from our institutional database. Shortlisted patients were classified into two groups according to postoperative POH diagnosis. Daily postural BP measures taken during physiotherapy sessions the week after surgery are used to diagnose POH. All patients underwent preoperative tests for brain natriuretic peptide (BNP) concentrations, as well as pre- and postoperative computed tomography (CT) to determine the length of the minor axis of the inferior vena cava (IVC) at the thoracolumbar level. The study was performed following the Declaration of Helsinki and ethical guidelines for medical and health research involving human subjects. The study protocol was approved by the Ethics Committee and Institutional Review Board of Kitasato Institute Hospital (approval number: 19027). All patients gave their informed consent, knowing that they could withdraw it by visiting the hospital website.
Inpatient records were retrospectively examined for patient characteristics, such as age, sex, body mass index (BMI), the presence of medical comorbidities (diabetes mellitus [DM], hypertension, ischemic heart disease, stroke, and Parkinson’s disease [PD]), premorbid mobility status, the presence of old vertebral fractures, and the preoperative American Spinal Injury Association (ASIA) grade, which reflects motor and sensory function, as previously reported [12]. The performance of a three-column osteotomy (including the replacement of the front vertebral body), the number of levels fused, the length of the operation, and the anticipated blood loss were all factors that were identified during the study of the surgical notes. For each patient, we collected standard, perioperative, spinopelvic alignment parameters (the coronal curve magnitude, C7–central sacral vertical line, pelvic incidence, pelvic tilt, lumbar lordosis, sagittal vertical axis, T10–L2 thoracolumbar kyphosis, and T4–12 thoracic kyphosis). Perioperative changes were calculated as the distances between the pre- and postoperative measurements. Statistical analysis was done to determine the importance of between-group variations in the aforementioned parameters.
Statistical analysis was conducted using GraphPad Prism ver. 9.0 (GraphPad Software, San Diego, CA, USA), and all significance tests were two-sided with a 5% significance level. Data normality was assessed using the Kolmogorov-Smirnov normality test. For continuous variables, the Student t-test (for normally distributed data) or the Mann-Whitney U test (for skewed data) was used to measure statistical significance. For categorical variables, the chi-square or Fisher’s exact test was used. Multiple logistic regression analysis was employed to determine the predictors of POH. An assessment of the goodness-of-fit was made on the model fit. Along with the odds ratios, the 95% confidence intervals (CIs) are presented.
A total of 65 consecutive patients met our inclusion criteria, of whom 6 (9%) experienced POH postoperatively. The patients had a mean age of 73.9 years (standard deviation=6.3 years; range, 52–85 years), and 46 (71%) were women. No statistically significant between-group differences were found for age; sex; BMI; the frequencies of hypertension, ischemic heart disease, cerebrovascular accidents, or old vertebral fractures; the number of levels fused, the total operative time, or the predicted blood loss (Table 1). Patients with POH were considerably more likely to have DM (p=0.032) and neurodegenerative disease (ND) (p<0.001). Furthermore, patients using walking aids and those with an ASIA grade D were substantially more likely to have POH than those who did not use walking aids (p=0.001) and those with an ASIA grade E (p<0.001), respectively. Radiographic analysis showed no significant differences between the two groups in terms of ASD features before and after surgery (Table 2). Furthermore, patients with POH had a substantially longer mean hospital stay than those without (71.2 days versus 51.8 days, p=0.030). The patients with POH may have experienced secondary problems, which may have contributed to the extended hospital stay (Table 3). They were given amezinium metilsulfate and midodrine hydrochloride to increase BP, and sodium chloride to retain body fluid in the postoperative period. As a result of serious secondary problems, they needed more invasive operations.
Multiple logistic regression analysis was used to examine the predictors (DM, ND, mobility, and ASIA grade) of postoperative POH that had been discovered with univariate significance testing (Table 4). After adjusting for DM, ND, mobility level, and ASIA grade, only ND was found to be an independent predictor of postoperative POH. In this research, we treated five patients with ND, including four patients with PD and one with multiple system atrophy (MSA); two patients with PD and one with MSA developed POH postoperatively. The chance of developing POH was almost 4.073 times higher in patients with NDs (95% CI, 1.094–8.362; p=0.020).
To elucidate the pathophysiology of postoperative POH, we compared the hemodynamic parameters of the pre- and postoperative IVC via CT imaging. Patients with and without POH had significantly different pre- and postoperative minor axis of the IVC lengths (Fig. 1A–C). The preoperative IVC in patients with postoperative POH was considerably larger than that in patients without postoperative POH. However, compared to patients without POH, those with POH had considerably smaller postoperative IVCs. Furthermore, the evaluation of the IVC dimensions based on the operative approach revealed that there was no significant difference in the perioperative IVC dimensions between the only posterior approach and the lateral and posterior approach (Table 5). We measured the BNP content in the patients before surgery to check for any indications of heart failure. Patients with POH and those without had similar BNP concentrations, with no discernible difference (Fig. 1D).
Postoperative POH is a well-documented phenomenon in patients with spinal cord injuries [13]. Illman et al. [14] found that postural changes during physiotherapy and mobilization induce clinically significant hypotensive episodes in 73.6% of patients, with symptoms of POH experienced by 58.9%. Furthermore, Ong et al. [12] found that postoperative POH occurred in 11.6% of patients who received cervical spinal surgery, with a poor preoperative ASIA grade being a risk factor. The mechanisms underlying POH in patients with the spinal disease are multifactorial. The sympathetic nervous system dysfunction, reduced baroreceptor sensitivity, inactive skeletal muscle pumps, cardiovascular deconditioning, and an altered salt and water balance are among the physiological anomalies that are hypothesized to be responsible for POH in these patients [15–17].
Well-established general risk factors for POH include age, cardiovascular diseases, and ND, such as diabetic autonomic neuropathy, MSA, and PD [18–20]. According to reports, POH affects between 9.6% and 65% of PD patients and between 54% and 81% of MSA patients [21,22]. Interestingly, Klanbut et al. [23] showed that older patients with PD should be closely assessed for the presence of symptomatic POH and advised to change positions slowly, particularly those involving a vertical orientation. Matinolli et al. [24] reported that patients with POH also had a statistically significantly increased postural sway when standing than did patients without POH. According to these data, people with ND who undergo corrective spinal surgery for ASD have a higher risk of developing POH.
Cardiovascular assessment in the current study indicated a reduction in blood flows through the IVC after the operation, with a subsequent reduction in the cardiac output, which may have induced POH. The collapse of the IVC is well-known to be associated with hypotension in women during late pregnancy [25,26] because the gravid uterus compresses the IVC when they are in the supine position, leading to dramatic hemodynamic changes. In addition, certain authors reported that measurement of the IVC diameter was very useful for the estimation of hemodynamic changes in patients with orthostatic intolerance [27,28]. Although our results imply that cardiovascular dysautonomia rather than mechanical compression brought on by spinal adjustment may have contributed to the IVC’s collapse following ASD surgery [29], further research into these issues is necessary.
Regarding the external validity of our findings, we think that our sample is representative of postoperative patient populations encountered in the same clinical setting. Our study has several drawbacks because of its retrospective nature. First, it is well-recognized that several variables, including the usage of medications, temperature, and the interval since the last meal, might affect the likelihood of POH [30]. The residual effects of these factors might have contributed to postoperative POH in our patients. Second, at our institution, postural BP is only assessed at the initiation of rehabilitation. Only in situations of severe or symptomatic POH was routine monitoring carried out. The low frequency and delay in measurement following surgery mean that we probably underestimated the incidence of POH, particularly in asymptomatic patients with transient or intermittent POH. Last, although our results showed that patients with POH had longer hospital stays, we also found that those with POH tended to use walkers and had poorer ASIA scores. POH and low amounts of activities of daily living may be both attributed to the longer hospital stay, rather than POH being the cause of both the longer hospital stay and the low amounts of activities of daily living.
This study has several limitations. First, this was not a prospective randomized control trial but a retrospective comparative study. Our results must be confirmed in prospective research. Second, it is unclear whether any uncommon causes, such as adrenal disease and amyloidosis, other than autonomic disturbances in diabetes and ND, are associated with this type of orthostatic hypotension.
We showed that POH is a potential complication of ASD surgery. The most pertinent risk factor thereof is having an ND. Given the deleterious effects associated with postoperative POH, we recommend that postural BP should be routinely monitored in patients with NDs, for the early intervention and effective rehabilitation of patients with POH.
Notes
Author Contributions
MT designed the study and wrote the initial draft of the manuscript. TI and TH contributed to analysis and interpretation of data and assisted in the preparation of the manuscript. MT was responsible for this submission, as corresponding author. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Fig. 1
Comparisons of cardiovascular parameters. (A, B) Representative preoperative (Preop) and postoperative (Postop) computed tomographic images of the thoracolumbar level of patients with persistent orthostatic hypertension (OH) (POH). The images reveal the remarkable postoperative collapse of the inferior vena cava (IVC) (arrowhead, IVC; double-headed arrow, the length of the minor axis). (C) The length of the minor axis of the IVC. There was a significant difference in the length of the minor axis of the IVC in patients before and after the operation (***p<0.001; by paired t-test). While the preoperative IVC in patients with POH was significantly larger than that in patients without POH, the postoperative IVC in patients with POH was significantly smaller than that in patients without POH (*p<0.05, **p<0.01; by unpaired t-test). (D) There was no significant difference in the preoperative brain natriuretic peptide (BNP) concentration between patients with and those without POH (mean, 62.1 pg/mL vs. 62.7 pg/mL; p=0.237). NS, not significant.
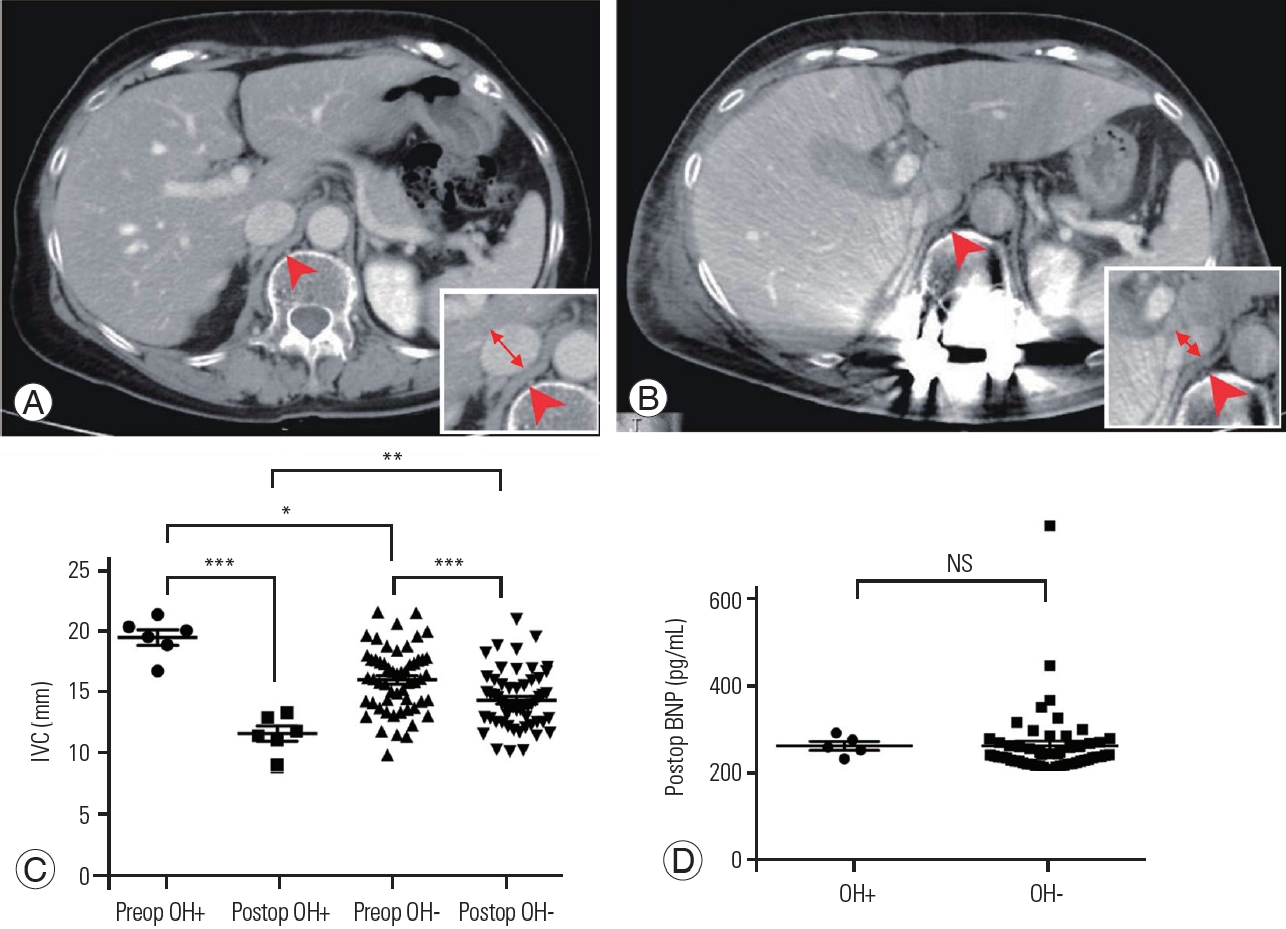
Table 1
Baseline characteristics and clinical profile
Table 2
Radiographic characteristics
Table 3
Secondary complications due to orthostatic hypotension
| Complication | With orthostatic hypotension (n=6) |
|---|---|
| Rehabilitation delay | 6 |
| Dizziness | 6 |
| Syncope | 3 |
| Bedsore | 1 |
| Implant infection | 1 |
| Inferior vena cava thrombosis | 1 |
| Acute cholecystitis | 1 |
Table 4
Multiple logistic regression analyses
References
1. Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005 30:1082–5.


2. Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2007 32:2764–70.


3. Acosta FL Jr, McClendon J Jr, O’Shaughnessy BA, et al. Morbidity and mortality after spinal deformity surgery in patients 75 years and older: complications and predictive factors. J Neurosurg Spine 2011 15:667–74.


4. Smith JS, Shaffrey CI, Glassman SD, et al. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine (Phila Pa 1976) 2011 36:817–24.

5. Yagi M, Michikawa T, Hosogane N, et al. Risk, recovery, and clinical impact of neurological complications in adult spinal deformity surgery. Spine (Phila Pa 1976) 2019 44:1364–70.


6. Berjano P, Damilano M, Pejrona M, Langella F, Lamartina C. Revision surgery in distal junctional kyphosis. Eur Spine J 2020 29(Suppl 1): 86–102.



7. Jain A, Hassanzadeh H, Puvanesarajah V, et al. Incidence of perioperative medical complications and mortality among elderly patients undergoing surgery for spinal deformity: analysis of 3519 patients. J Neurosurg Spine 2017 27:534–9.


8. Freeman R, Abuzinadah AR, Gibbons C, Jones P, Miglis MG, Sinn DI. Orthostatic hypotension: JACC state-of-the-art review. J Am Coll Cardiol 2018 72:1294–309.

9. Feldstein C, Weder AB. Orthostatic hypotension: a common, serious and underrecognized problem in hospitalized patients. J Am Soc Hypertens 2012 6:27–39.


10. Krassioukov A, Eng JJ, Warburton DE, Teasell R, Spinal Cord Injury Rehabilitation Evidence Research Team. A systematic review of the management of orthostatic hypotension after spinal cord injury. Arch Phys Med Rehabil 2009 90:876–85.



11. Hocker S, Hoover JM, Puffer RC, Meyer FB. Orthostatic hypotension following resection of a dorsal medullary hemangioblastoma. Neurocrit Care 2012 16:306–10.



12. Ong ET, Yeo LK, Kaliya-Perumal AK, Oh JY. Orthostatic hypotension following cervical spine surgery: prevalence and risk factors. Global Spine J 2020 10:578–82.




13. McKinley WO, Tewksbury MA, Godbout CJ. Comparison of medical complications following nontraumatic and traumatic spinal cord injury. J Spinal Cord Med 2002 25:88–93.


14. Illman A, Stiller K, Williams M. The prevalence of orthostatic hypotension during physiotherapy treatment in patients with an acute spinal cord injury. Spinal Cord 2000 38:741–7.



15. Faghri PD, Yount JP, Pesce WJ, Seetharama S, Votto JJ. Circulatory hypokinesis and functional electric stimulation during standing in persons with spinal cord injury. Arch Phys Med Rehabil 2001 82:1587–95.


16. Wecht JM, De Meersman RE, Weir JP, Spungen AM, Bauman WA. Cardiac autonomic responses to progressive head-up tilt in individuals with paraplegia. Clin Auton Res 2003 13:433–8.



17. Stjernberg L, Blumberg H, Wallin BG. Sympathetic activity in man after spinal cord injury: outflow to muscle below the lesion. Brain 1986 109(Pt 4): 695–715.


18. Hanada M, Tawara Y, Miyazaki T, et al. Incidence of orthostatic hypotension and cardiovascular response to postoperative early mobilization in patients undergoing cardiothoracic and abdominal surgery. BMC Surg 2017 17:111.




19. Sun Z, Jia D, Shi Y, et al. Prediction of orthostatic hypotension in multiple system atrophy and Parkinson disease. Sci Rep 2016 6:21649.




20. Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS. Orthostatic hypotension in older adults: the Cardiovascular Health Study. CHS Collaborative Research Group. Hypertension 1992 19(6 Pt 1): 508–19.


21. Senard JM, Rai S, Lapeyre-Mestre M, et al. Prevalence of orthostatic hypotension in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1997 63:584–9.



22. Pavy-Le Traon A, Piedvache A, Perez-Lloret S, et al. New insights into orthostatic hypotension in multiple system atrophy: a European multicentre cohort study. J Neurol Neurosurg Psychiatry 2016 87:554–61.


23. Klanbut S, Phattanarudee S, Wongwiwatthananukit S, Suthisisang C, Bhidayasiri R. Symptomatic orthostatic hypotension in Parkinson’s disease patients: prevalence, associated factors and its impact on balance confidence. J Neurol Sci 2018 385:168–74.


24. Matinolli M, Korpelainen JT, Korpelainen R, Sotaniemi KA, Myllyla VV. Orthostatic hypotension, balance and falls in Parkinson’s disease. Mov Disord 2009 24:745–51.


25. Lanni SM, Tillinghast J, Silver HM. Hemodynamic changes and baroreflex gain in the supine hypotensive syndrome. Am J Obstet Gynecol 2002 187:1636–41.


26. Humphries A, Mirjalili SA, Tarr GP, Thompson JM, Stone P. Hemodynamic changes in women with symptoms of supine hypotensive syndrome. Acta Obstet Gynecol Scand 2020 99:631–6.



27. Fujii Y, Ishizaki Y, Kino M, Taniuchi S, Kobayashi Y, Kaneko K. Two types of orthostatic dysregulation assessed by diameter of inferior vena cava. Pediatr Int 2011 53:162–7.









