Does Baseline Severity of Arm Pain Influence Outcomes Following Single-Level Anterior Cervical Discectomy and Fusion?
Article information
Abstract
Study Design
Retrospective cohort.
Purpose
To assess preoperative arm pain severity influence on postoperative patient-reported outcomes measures (PROMs) and minimal clinically important difference (MCID) achievement following single-level anterior cervical discectomy and fusion (ACDF).
Overview of Literature
There is evidence that preoperative symptom severity can affect postoperative outcomes. Few have evaluated this association between preoperative arm pain severity and postoperative PROMs and MCID achievement following ACDF.
Methods
Individuals undergoing single-level ACDF were identified. Patients were grouped by preoperative Visual Analog Scale (VAS) arm ≤8 vs. >8. PROMs collected preoperatively and postoperatively included VAS-arm/VAS-neck/Neck Disability Index (NDI)/12-item Short Form (SF-12) Physical Composite Score (PCS)/SF-12 mental composite score (MCS)/Patient-Reported Outcomes Measurement Information System physical function (PROMIS-PF). Demographics, PROMs, and MCID rates were compared between cohorts.
Results
A total of 128 patients were included. The VAS arm ≤8 cohort significantly improved for all PROMs excepting VAS arm at 1-year/2-years, SF-12 MCS at 12-weeks/1-year/2-years, and SF-12 PCS/PROMIS-PF at 6-weeks, only (p≤0.021, all). The VAS arm >8 cohort significantly improved for VAS neck at all timepoints, VAS arm from 6-weeks to 1-year, NDI from 6-weeks to 6-months, and SF-12 MCS/PROMIS-PF at 6-months (p≤0.038, all). Postoperatively, the VAS arm >8 cohort had higher VAS-neck (6 weeks/6 months), VAS-arm (12 weeks/6 months), NDI (6 weeks/6 months), lower SF-12 MCS (6 weeks/6 months), SF-12 PCS (6 months), and PROMIS-PF (12 weeks/6 months) (p≤0.038, all). MCID achievement rates were higher among the VAS arm >8 cohort for the VAS-arm at 6-weeks/12-weeks/1-year/overall and NDI at 2 years (p≤0.038, all).
Conclusions
Significance in PROM score differences between VAS arm ≤8 vs. >8 generally dissipated at the 1-year and 2-year time-point, although higher preoperative arm pain patients suffered from worse pain, disability, and mental/physical function scores. Furthermore, clinically meaningful rates of improvement were similar throughout the vast majority of timepoints for all PROMs studied.
Introduction
Patients with cervical spine degenerative disc disease (DDD) refractory to conservative measures were proven to substantially benefit upon receiving anterior cervical discectomy and fusion (ACDF), considered traditionally to be the gold standard of operative management [1]. Patients undergoing ACDF have demonstrated significant improvements in neck pain (measured by Visual Analog Scale [VAS] neck), arm pain (measured using VAS arm), physical function (measured using 12-item Short Form [SF-12] Physical Composite Score [PCS]), and disability (measured using Neck Disability Index [NDI]) [2]. Concomitant or isolated radicular arm pain is not uncommon while patients may initially present with axial neck pain [3]. It has been conventional wisdom that patients with radicular pain are more likely to require surgery compared with those suffering from primary axial pain [3]. To our knowledge, no study has evaluated outcomes based on stratified levels of radicular arm pain at initial presentation, whereas some studies have evaluated the influence of differing ratios of neck/arm pain on postoperative outcomes following ACDF [2–4]. The present study aimed to determine the effect of baseline arm pain severity on patient-reported outcome measures (PROMs) and minimal clinically important difference (MCID) achievement following ACDF.
Materials and Methods
1. Patient population
Institutional Review Board (IRB) approval was obtained from Rush University Medical Center before study (ORA #14051301). Informed consent was obtained from all individual participants included in the study. A retrospective attending spine surgeon database, which was prospectively maintained, was searched to determine patients undergoing ACDF at a single-level. Patients undergoing ACDF for herniated nucleus pulposus (HNP), DDD, and/or central or foraminal cervical stenosis were selected. Individuals missing preoperative VAS arm data were excluded. Subjects receiving ACDF for infection, trauma, or malignancy were also excluded. In patients meeting the selection criteria, a preoperative VAS arm score representing the 75th percentile (8) as the cutoff was used to divide the patients into two groups: VAS arm ≤8 versus VAS arm >8. This percentile was used because it allowed for a more prominent separation of preoperative arm pain data (versus using median/mean score) while permitting an adequate sample size (n>30) within the VAS arm >8 group. Neuropathy data (i.e., radiculopathy, myelopathy, and myeloradiculopathy) were not used as selection criteria; however, among included patients who did have neuropathy data, rates of myelopathy, radiculopathy, and myeloradiculopathy in the total cohort and within each group were reported.
2. Data collection
The following demographic characteristics were collected: age, body mass index (BMI), gender, ethnicity, diabetic status, smoking status, hypertensive status, American Society of Anesthesiologists classification, Charlson comorbidity index score, and insurance status. Preoperative spinal pathology, neuropathy data (myelopathy, radiculopathy, and myeloradiculopathy), operative time, estimated blood loss, length of stay, postoperative day (POD) 0/1 VAS pain, POD 0/1 narcotic consumption (in oral morphine equivalents [OME]), and 1 year arthrodesis rates (among patients with available radiographic data) were also collected. Preoperative and postoperative (6 weeks, 12 weeks, 6 months, 1 year, and 2 years) PROMs were collected for VAS neck/arm, NDI, SF-12 PCS, mental composite score (MCS), and Patient-Reported Outcomes Measurement Information System physical function (PROMIS-PF).
3. Data analysis
Stata ver. 16.0 (Stata Corp., College Station, TX, USA) was used for all data analysis. Descriptive statistics were performed among demographic/perioperative characteristics, with intergroup differences evaluated using Student t-test for independent samples (for continuous variables) and chi-square test for categorical variables. Paired samples t-tests were performed to determine improvement significance from preoperative to each postoperative timepoint within groups. Student t-test for samples was utilized to evaluate intergroup differences in mean PROM ratings. MCID achievement was defined by the following established thresholds for delta PROMs: VAS neck [5]=2.6, VAS arm [5]=4.1, NDI [6]=8.5, SF-12 PCS [5]=8.1, SF-12 MCS [5]=4.7, and PROMIS-PF [6]=4.5. Intergroup differences in MCID attainment rates were evaluated using chi-square tests.
Results
1. Descriptive analysis
A total of 128 patients were selected for inclusion in this study, with 97 patients in the VAS arm preoperative ≤8 group and 31 patients in the VAS arm >8 group. The mean age was 47.2 years, and the mean BMI was 30.0 kg/m2 with most subjects being males (63.3%). No significant differences were observed in demographic characteristics between the VAS arm groups (Table 1). HNP was the most common presenting spinal pathology, present in 92.2% of the total cohort. The majority of patients (84.6%, n=107) presented with myeloradiculopathy among patients with available neuropathy data, followed by radiculopathy only (14.1%, n=18), and myelopathy only (1.2%, n=2). Mean operative duration (50.2 minutes) and length of stay (11.4 hours) did not significantly differ among groups, along with POD0/1 VAS pain scores and POD0 narcotic consumption. Estimated blood loss was significantly higher in the VAS arm ≤8 group (29.2 versus 24.2, p=0.013), whereas POD1 narcotic consumption was significantly higher in the VAS arm >8 group (14.0 OME versus 5.5 OME, p=0.012). The 1-year arthrodesis rates in the total cohort and within each group were identical (94.7%) (Table 2).
2. Primary outcome measures
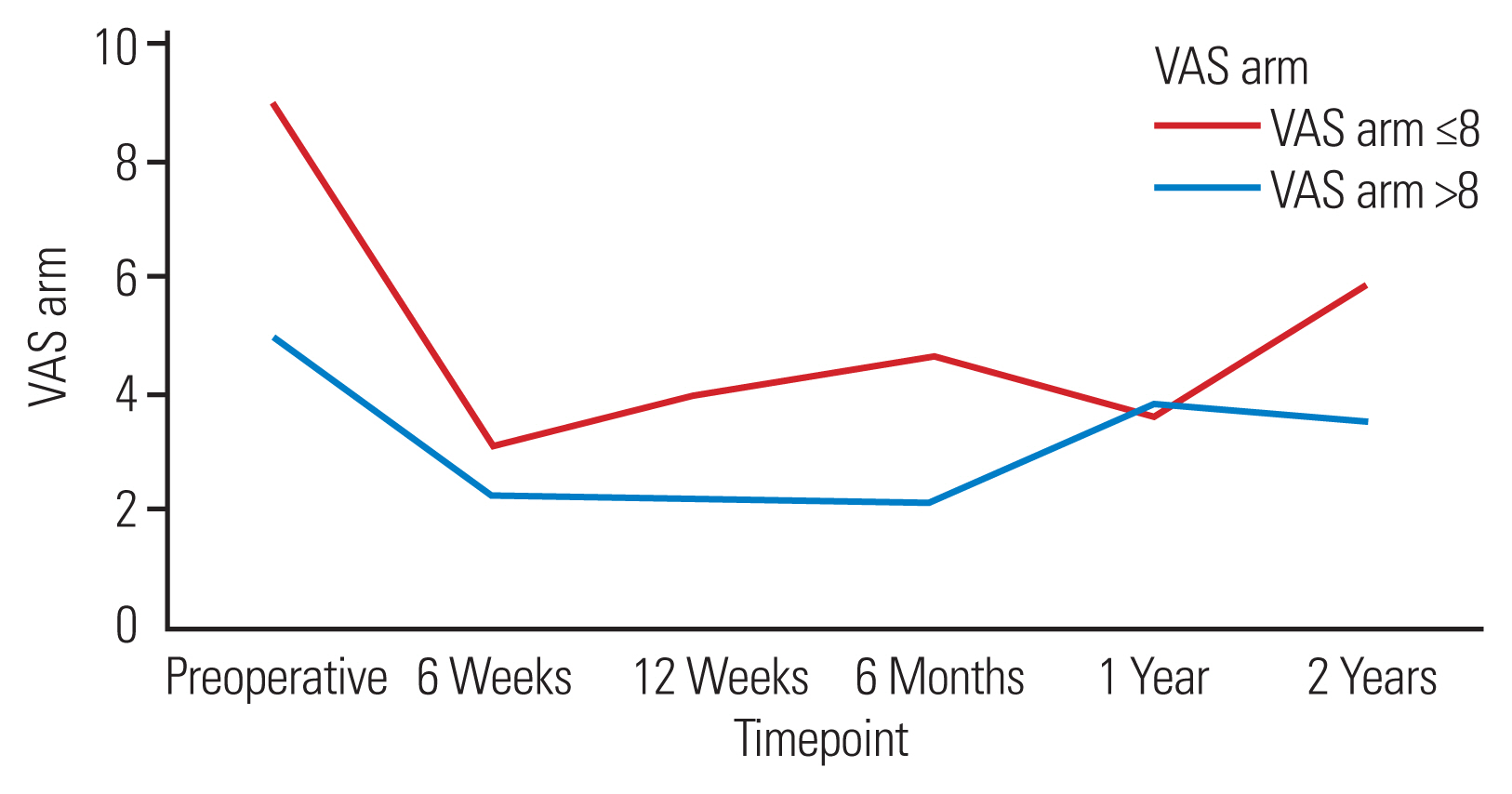
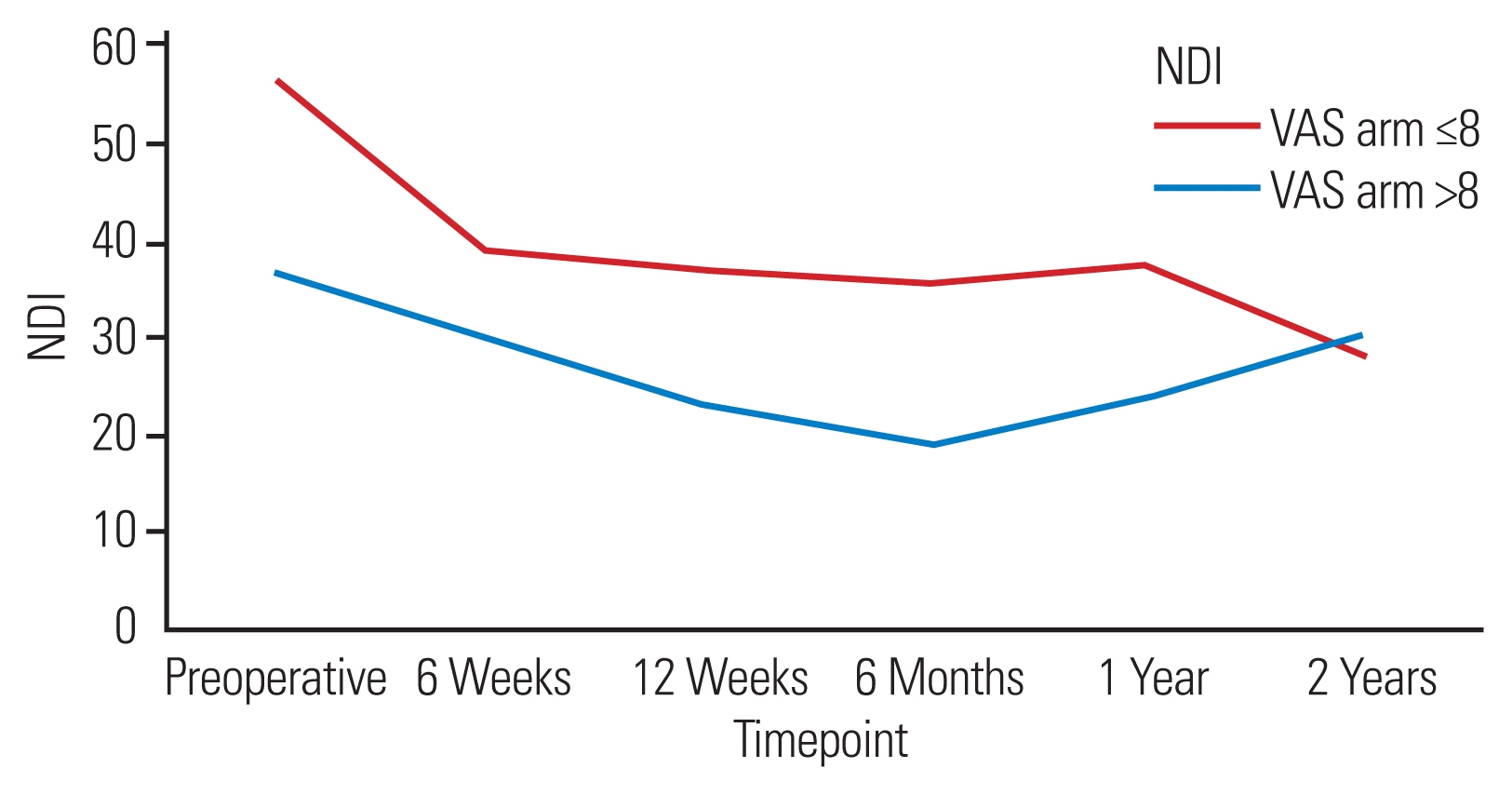
Patients in the VAS arm ≤8 group demonstrated significant improvements for all PROMs except VAS arm at 1 year/2 years, SF-12 MCS at 12 weeks/1 year/2 years, and SF-12 PCS and PROMIS-PF at 6 weeks (p≤0.021, all). Patients in the VAS arm >8 group demonstrated significant improvements for VAS neck in the entire postoperative period, VAS arm from 6 weeks till 1 year, NDI from 6 weeks till 6 months, and SF-12 MCS/PROMIS-PF at 6 months, only (p≤0.038, all). The VAS arm >8 group reported significantly higher VAS neck (at preoperative/6 months), VAS arm (at the preoperative/12 weeks/6 months), NDI (from preoperative to 6 months), and significantly lower SF-12 MCS (from preoperative to 12 weeks), SF-12 PCS (at 6 months), and PROMIS-PF (preoperative/12 weeks/6 months) (p≤0.048, all) (Table 3). Mean PROM scores by group over the timepoints studied have also been depicted via line graphs (Figs. 1–6). MCID achievement rates for the VAS arm at 6 weeks/12 weeks/1 year and overall, and NDI at 2 years were significantly higher in the VAS arm >8 cohort (p≤0.038, all). MCID attainment rates for VAS neck, SF-12 MCS, SF-12 PCS, and PROMIS-PF did not significantly differ at any postoperative timepoint (p≥0.050, all) (Table 4).

Mean 12-item Short Form Mental Composite Score (SF-12 MCS) scores by group. VAS, Visual Analog Scale.

Mean 12-item Short Form Physical Composite Score (SF-12 PCS) scores by group. VAS, Visual Analog Scale.

Mean Patient-Reported Outcomes Measurement Information System physical function (PROMIS-PF) scores by group. VAS, Visual Analog Scale.
Discussion
ACDF remains the gold standard for operative treatment of cervical degenerative pathology causing persistent neck and/or arm pain from nerve root compression with 137,000 procedures performed between 2006 and 2013 [7]. PROM questionnaires have been increasingly used by spinal surgeons to evaluate the postoperative quality-of-care and cost-effectiveness of this procedure [7]. PROMs are surveys administered to patients to monitor their pain (i.e., VAS neck/arm), disability (i.e., NDI), physical function (i.e., SF-12 PCS and PROMIS-PF), and mental health (i.e., SF-12 MCS) following surgery. Determination of MCID achievement is useful to ascertain if clinically meaningful improvement has been reached, whereas PROMs provide meaningful data from the patient’s perspective [8].
Many studies have used preoperative PROMs to predict and assess correlations with postoperative recovery. Nevertheless, as per our knowledge, the effect of preoperative VAS arm scores on postoperative outcomes has not been studied [2,9,10]. Therefore, the present study aimed to analyze the influence of baseline arm pain severity on PROM scores (VAS neck/arm, SF-12 MCS/PCS, and PROMIS-PF) and MCID achievement among recipients of single-level ACDF.
1. Pain
Pain has been proven to stand as a strong predictor for surgical outcomes regarding ACDF procedures [11]. Our analysis demonstrated that both neck and arm pain showed a significant reduction from preoperative to postoperative scores, which is in line with previous studies [7,12]. Expectedly, preoperative VAS arm and VAS neck scores were significantly greater in the VAS arm >8 cohort upon the comparison of preoperative VAS scores between both cohorts. Acute postoperative pain scores (although not reaching significance) and day 1 narcotic consumption were also slightly higher for this cohort. Importantly, this trend of worsened pain for this cohort persisted in postoperative VAS pain values up to 6 months following surgery for both neck and arm pain. Mean neck/arm pain scores were still generally higher at 1 year/2 years following ACDF for the VAS arm >8 cohort, whereas postoperative values after 6 months did not show a significant difference between the groups, suggesting the lack of statistical significance may have been due to restricted sample size at the 1- and 2-year timepoints due to being lost to follow-up.
No significant differences were observed for the achievement of VAS neck throughout the postoperative period upon the comparison of MCID attainment rates. Meanwhile, a higher MCID achievement rate was observed for arm pain within the VAS arm >8 versus ≤8 cohorts. This concurs with previous study findings in which higher preoperative pain scores have been associated with higher rates of clinical improvements [10].
Ultimately, our findings indicate that higher preoperative arm pain scores may lead to worsened pain perception, especially in the months following ACDF, but possibly even at longer-term follow-up (1 year/2 years following surgery). Meanwhile, other literature suggests that higher preoperative pain levels may not compromise postoperative pain outcomes albeit commenting primarily on the influence of preoperative neck pain [10,13]. Further studies are necessary to illustrate its longitudinal impact on postoperative pain as arm pain investigation as a postoperative outcome predictor remains in its infancy. Nonetheless, ACDF candidates with higher preoperative arm pain should expect equivocal rates of clinically significant improvements in neck pain. Furthermore, this patient population can be assured that clinically meaningful improvements in arm pain will likely not be compromised by preoperative pain status and may be even more likely among those presenting with higher VAS arm.
2. Disability
One of the most commonly used PROMs in cervical procedures is NDI [14]. The instrument’s high reliability and clinical applicability make it a vital tool for measuring patient disability, which is an important prognosticating factor [15]. Thus, it is imperative to determine whether variance in levels of preoperative arm pain influences postoperative disability.
The VAS arm ≤8 cohort showed significant improvements from preoperative to postoperative mean NDI scores at all timepoints of this study, whereas the VAS arm >8 cohort only exhibited significant improvements until 6 months. The VAS arm >8 cohort preoperative NDI scores were significantly higher when comparing disability scores between cohorts, a trend which continued until 6 months postoperatively. Cha et al. [9] have shown that higher preoperative NDI scores have been noted to hinder improvements in pain scores. We have similarly found that higher preoperative VAS arm scores appear to have similar effects on reducing the potential for NDI score improvement after surgery in the present analysis. Fortunately, the significance of this effect persisted only in the short-term period, suggesting that baseline arm pain severity may not significantly alter neck-related disability in the years following ACDF. Notably, MCID achievement rates also did not differ significantly at most timepoints or during the overall follow-up period. The authors similarly discovered that improvements in disability were not influenced by pain level at presentation while Stull et al. [10] evaluated the influence of preoperative neck and not arm pain. Patients suffering from higher arm pain levels at presentation should be counseled on evidence-based trends suggesting that while greater disability may be experienced in the months following ACDF, this trend will likely dissipate by 1–2 years following fusion and does not appear to influence rates of clinically meaningful disability-related improvements.
3. Physical function
Understanding a patient’s physical function preoperatively can help guide an individualized treatment strategy and quantity of a patient’s postoperative recovery progress. A few studies have directly linked the effects of varying severity of arm pain on physical function scores following ACDF, whereas previous studies have shown a relationship between preoperative PROMIS-PF scores and postoperative outcomes in arm and neck pain [2,16]. This study assessed the postoperative values of both PROMIS-PF and SF-12 PCS physical function questionnaires to help monitor functionality.
The preoperative VAS arm ≤8 cohort showed significant improvements from preoperative to postoperative values from 12 weeks to 2 years for both PROMIS-PF and SF-12 PCS. Meanwhile, the VAS arm >8 cohort only improved significantly for PROMIS-PF at 6 months and did not improve for SF-12 PCS at any postoperative timepoint. Furthermore, the VAS arm >8 cohort generally reported significantly inferior physical health scores through the 6-month follow-up period when comparing mean PROM scores between the VAS arm ≤8 and >8 cohorts. This association of higher pain with a lower physical function was previously described by Parrish et al. [17], in which patients with lower PROMIS-PF suffered from higher pain levels preoperatively and postoperatively. A study by Hermansen et al. [18] also commented on the close relationship between pain and physical function among ACDF candidates, stating that neck-specific function was closely tied to pain levels. Nevertheless, 1- and 2-year scores did not differ between groups for either PROMIS-PF or SF-12 PCS in our findings, and MCID achievement results were largely comparable throughout the entire postoperative period. Surgeons should counsel individuals concerned about physical functioning that while higher arm pain severity may interfere with recovery in the weeks to months following cervical fusion, 1- and 2-year clinical outcomes and meaningful improvement rates are unlikely to be affected. The healthcare team may enable the patient’s expectations to be more in tune with the probable recovery trajectory by including this information as part of the preoperative planning process.
4. Mental health
The SF-12 MCS questionnaire has been shown to be an acceptable screening tool for both active and recent depressive disorders in the general population regarding mental health [19]. Both cohorts in our study generally demonstrated sparse improvements from preoperative to postoperative scores. Notably, however, patients found with higher preoperative arm pain (VAS arm >8) generally reported lower mental health scores throughout the entire postoperative period when comparing mean PROM values between the two cohorts, albeit significance was only reached from preoperative through 12 weeks following fusion. Previous papers have reported mixed results when examining the influence of preoperative mental health on postoperative pain following ACDF [20–22]. Goh et al. [20] found no difference in pain improvements, satisfaction, or expectation fulfillment upon stratification of cohorts by preoperative SF-36 MCS score, whereas Jenkins et al. [22] illustrated higher Patient Health Questionnaire-9 at baseline was associated with higher pain scores. As our analysis reports on the inverse, namely, preoperative pain’s influence on postoperative mental health scores, our observed lower mental functioning trend among those with higher baseline arm pain is important for surgeons to be aware of. Nevertheless, it should be noted that MCID achievement results were similar throughout the entire follow-up period, supporting the notion that while higher initial arm pain severity may result in poorer mental functioning scores (especially within the early postoperative period) clinically meaningful improvements may not be impacted.
Although the MCID findings of our study are encouraging, this should not diminish the importance of postoperative mental health monitoring and management, as patients who presented with higher pain may require greater support. Furthermore, numerous studies have shown that poor mental health in vulnerable populations was strongly associated with increased difficulty recovering from various surgical procedures and increased risk for suicidal ideations and behavior, which cannot be taken lightly [23–25]. Healthcare professionals should employ mental health assessment and screening tools preoperatively and postoperatively and inform patients of presented trends to align patients’ expectations with likely outcomes.
5. Limitations
This was presented with several limitations. First, all procedures were conducted by a single attending spinal surgeon at a single academic institution, restricting the generalizability of our results. Second, response bias may have skewed our results due to the subjective nature of patient-reported outcome questionnaires. Response bias may have skewed achievement rates as well as MCID achievement is calculated from delta PROMs. Additionally, variances in the literature on MCID calculation thresholds pose challenges to the interpretation of this clinical outcome measure. Furthermore, as the lower preoperative VAS arm cohort experienced significantly higher intraoperative blood loss, this may have contributed to confounder bias in our findings. Finally, loss to follow-up may have provided selection bias, especially to our 1- and 2-year results as this is a retrospective cohort study with a follow-up period extending until 2 years.
Conclusions
Surgical ACDF candidates presenting with higher preoperative arm pain suffered from inferior baseline pain, disability, and mental/physical function scores prior to surgery, with poorer postoperative PROMs primarily in the early and intermediate postoperative period and higher narcotic consumption on POD1. Despite these differences, 1- and 2-year PROMs were generally equivalent irrespective of presenting arm pain severity. Overall, MCID achievement for arm pain was significantly higher in the VAS arm >8 cohort, suggesting that this group was more likely to experience clinically meaningful benefits for radicular pain relief. Nonetheless, differing levels of baseline arm pain generally did not influence overall rates of clinically meaningful improvements as MCID attainment rates were largely equivalent between groups for VAS neck, NDI, SF-12 MCS, SF-12 PCS, and PROMIS-PF.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: MRP, KCJ, KS; formal analysis: MRP, KCJ, KS; methodology: MRP, KCJ, FAC, AWP, KS; data curation: NNV, HP, MCP; project administration: MRP, KCJ, KS; visualization: MRP, KCJ, KS; writing-original draft: MRP, KCJ, FAC, AWP, KS; writing-review & editing: MRP, KCJ, FAC, AWP, NNV, HP, MCP, KS; and final approval of the manuscript: all authors.