Introduction
More than 84% of the human population experience low back pain during their lives due to various pathologies [
1,
2]. Up to 25% of low back pain can come from the sacroiliac joint (SIJ), and SIJ fusion can be conducted if conservative treatment fails [
3]. SIJ fusion is a minimally invasive or open surgery used to treat SIJ pain from degeneration if all conservative treatments have been exhausted [
4-
6]. The diagnosis of SIJ pain is difficult, as patients present with low back and/or lower extremity pain, which could be linked to discogenic disease. However, the SIJ has been identified as a pain generator in 13%–30% of patients with chronic low back pain [
3,
5-
8]. Also, prior lumbosacral fusion can lead to low back pain, potentially increasing SIJ mobility and stress [
9-
12]. This increase in SIJ mobility or instability influences post-fusion (L5–S1) low back pain, leading to diagnoses of SIJ dysfunction and/or degeneration [
9-
13]. Often, an infra-adjacent segment disease such as SIJ dysfunction is a complication associated with lumbosacral fusion [
13]. In such cases, unilateral trans-articular sacroiliac fixation is often used to facilitate SIJ fusion.
The pelvis is a ring-like structure composed of two SIJs and the pubic symphysis [
6]. Based on the nature of its ring structure, hypermobility or stabilization of one SIJ can lead to changes in stresses or range of motion (ROM) of the contralateral SIJ [
14]. Biomechanical studies have demonstrated that unilateral stabilization significantly reduces fixated joint ROM, and that bilateral stabilization provides the most stability in flexion-extension (FE), lateral bending (LB), and axial rotation (AR) [
15-
17]. However, only one study has investigated the contralateral SIJ ROM following unilateral SIJ stabilization using three triangular titanium plasma spray implants. Lindsey et al. [
18] found that contralateral SIJ ROM did not significantly decrease for FE, LB, and AR. This lack of significant reduction in contralateral SIJ ROM could be attributed to the mobility of the pubis symphysis [
18].
Ivanov et al. [
19] showed that lumbar fusion increases the angular motion across the SIJ. Ha et al. [
9] reported that 75% of patients with lumbosacral fusion developed SIJ degeneration with a higher incidence of SIJ degeneration in those with fusions to S1 than to L5. This increase in joint mobility and degeneration results in pain followed by additional SIJ unilateral or bilateral fusion. Unilateral stabilization following lumbosacral fusion reduced ROM in the fixated SIJ [
15]; however, effects on the contralateral SIJ are still unknown. Therefore, this study evaluated the effect of unilateral SIJ stabilization with and without L5–S1 fixation on the contralateral SIJ by measuring ROM. The authors hypothesized that unilateral SIJ stabilization with L5–S1 fixation results in contralateral joint instability or hypermobility.
Materials and Methods
1. Specimen preparation
Seven human cadaveric lumbopelvic spines from L3 to pelvis were used (four males, three females; mean age, 53±11 years old). Specimens were confirmed to be devoid of degeneration and osteophytes by anteroposterior and lateral radiographs, and were stored at −20°C in double plastic bags until the testing day. Dissection at L3 and the pelvis was performed without disrupting critical structures, such as spinal ligaments, joint capsules, joints, and disks. Each specimen was fixed proximally at L3 and distally at the ischium of the pelvis with screws using a 3:1 mixture of Bondo Autobody Filler (Bondo/MarHyde Corp., Atlanta, GA, USA) and fiberglass resin (Home Solutions All Purpose, Bondo/MarHyde Corp.). Consequently, the sacrum and pubic symphysis were free to move. Normal saline (0.9%) was applied to specimens throughout testing to maintain viscoelastic tissue properties [
20].
2. Ethics statement
As this study did not involve human subjects, Institutional Review Board approval was not necessary for this study, and therefore was not sought for the research documented in this manuscript. The device(s)/drug(s) is/are US Food and Drug Administration-approved or approved by corresponding national agency for this indication.
3. Flexibility testing
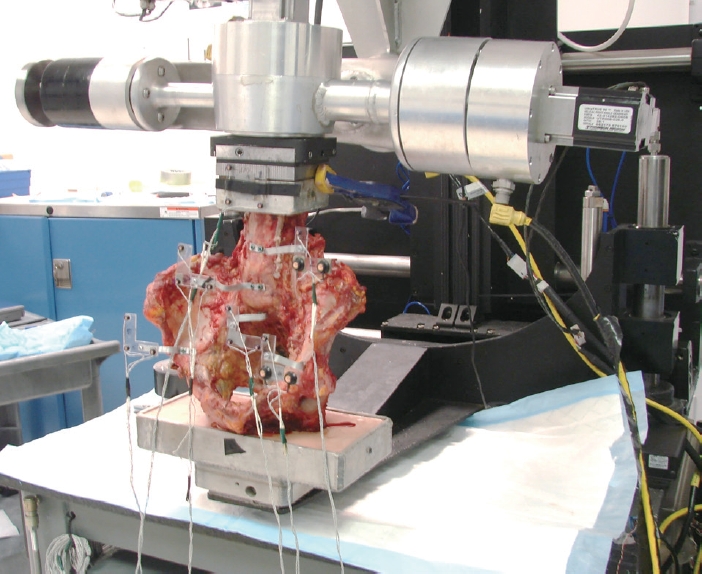
Spine specimens were affixed to a six-degrees-of-freedom testing apparatus by magnetization, and pure unconstrained bending moments were applied in three physiological rotation axes: FE, LB, and AR [
21]. This system used three cephalad stepper motors (Harmonic Drive Systems Inc., Tokyo, Japan) to apply a pure moment at L3 at a rate of 1.5°/sec to a maximum moment of ±8.5 Nm [
22]. Three load/unload cycles were performed for each direction, with data analysis based on the final cycle to account for the tissue viscoelasity.
The resultant three-dimensional ROM of the left and right SIJ was tracked using an Optotrak Certus (NDI Inc., Waterloo, ON, Canada) motion analysis system. Plexiglas markers with three infrared light-emitting diodes were secured rigidly to L3, L4, L5, sacrum, left iliac crest, and right iliac crest via bone screws, and applied perpendicular to the sagittal plane (
Fig. 1). Optotrak Certus software (NDI Inc.) inferentially superimposes the coordinate systems of two adjacent rigid bodies to determine relative Eulerian rotation in each of the three planes with noise measured to approximately 0.04° [
23].
4. Surgical stabilization groups
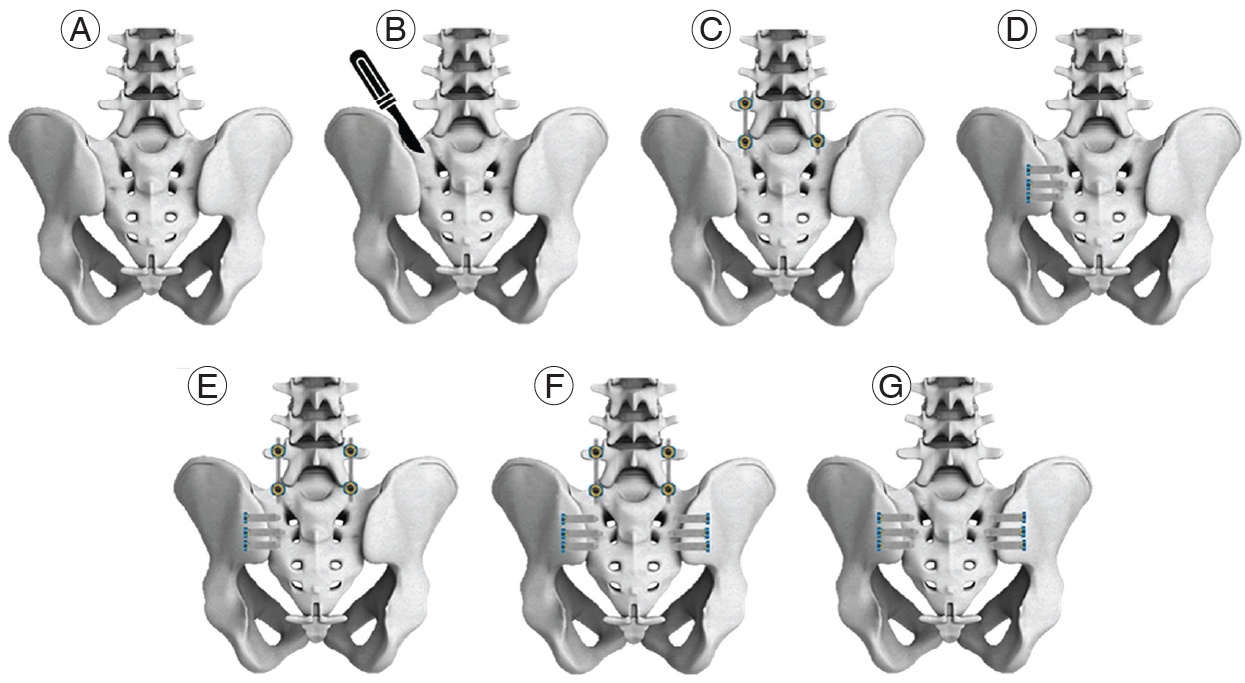
Each cadaveric specimen was sequentially tested as follows (
Fig. 2): (1) intact; (2) left-side posterior and iliosacral ligaments injury (injury); (3) L5–S1 instrumentation (L5–S1 rods); (4) three unilateral (left-side) SIJ screws (three SIJ screws); (5) L5–S1 fixation+three unilateral (left-side) SIJ screws (L5–S1 rods+three SIJ screws); (6) L5–S1 fixation+six bilateral SIJ screws (L5–S1 rods+six SIJ screws); and (7) six bilateral SIJ screws (six SIJ screws).
All specimens were tested in the intact state before any ligamentous injuries were made. The ligamentous injury group modeled the SIJ unstable condition, which is found before surgical stabilization. Both left-sided iliosacral and posterior ligaments injury was created by the insertion of the scalpel into the entire junction of the posterior iliac crest and sacrum from its most cephalad to its most caudal border, transecting all transverse and oblique attachments down to the joint. All left-side ligament injuries were made before ROM testing with hardware in place.
The REVERE Stabilization System (Globus Medical Inc., Audubon, PA, USA) was used for the 5.5-mm-diameter rigid titanium rod construct for lumbosacral fixation. The SI-LOK SIJ Fixation System (Globus Medical Inc.) was used for all lateral SIJ screws for SIJ fixation. Slotted and fixation SIJ screws were used for all constructs. Screws were 10 mm in diameter and 30–45 mm in length, depending on anatomy. Three screws were implanted into the left SIJ for unilateral stabilization and three screws in both the left and right SIJ for bilateral stabilization. All screws were placed across the SIJ under fluoroscopic guidance. Radiographs showed that SIJ screws started in the iliac crest lateral cortex and crossed the joint, with the screw tip within the sacrum, with intact neural foramen.
5. Data analyses
Left and right SIJ ROM were recorded for intact, ligamentous injury, and stabilization groups. Normalized ROM for all stabilization groups was calculated with respect to the ligamentous injury state since this modeled the unstable SIJ before stabilization. ROM of each joint was normalized to its respective joint in the injury state (i.e., left to left and right to right). Normal data distribution was verified using the Shapiro-Wilk test of normality (IBM SPSS ver. 22.0; IBM Corp., Armonk, NY, USA). A repeated-measures analysis of variance was performed with a within-subjects factor of treated condition (construct) and a between-subjects factor of joint side (left or right) for each loading direction. Post hoc comparisons were analyzed using Bonferroni adjustment (p<0.05).
Results
No specimens were excluded from the analysis because of slippage or fixation failure. Intact ROM was not significantly different between left and right SIJ for FE (p=0.991), LB (p=0.939), and AR (p=0.983). Mean magnitudes for intact ROM for all directions were less than 1° for both left and right SIJ, with the lowest magnitude of ROM observed in LB. The addition of ligament injury and L5–S1 fixation increased ROM for both left and right SIJ in all directions; however, there were no statistically significant differences between left and right SIJ (p>0.850).
There were no statistical differences between left and right SIJ for all bilateral stabilization groups with and without L5–S1 fixation in all loading directions: FE (
p>0.965), LB (
p>0.901), and AR (
p>0.796) (
Fig. 3). Likewise, there were no significant differences between left (fixated) and right (no fixation) SIJ for all unilateral stabilization groups in all loading directions: FE (
p=0.994), LB (
p=0.761), and AR (
p=0.899) (
Fig. 2). L5–S1 fixation in addition to unilateral SIJ fixation did not significantly increase or decrease the contralateral (right) SIJ ROM in all loading directions (
p>0.893). Contralateral (right) SIJ ROM for both unilateral and bilateral stabilization groups with and without L5–S1 fixation was not significantly different from injury for all loading directions (
p>0.696). Right SIJ ROM following bilateral stabilization with and without L5–S1 fixation was smaller than the right SIJ of injury for FE (25% and 25%), LB (44% and 37%), and AR (35% and 32%). In FE, the right SIJ ROM for unilateral stabilization groups was smaller than the right SIJ of injury by 11% with L5–S1 fixation and 16% without L5–S1 fixation (
Table 1). Similarly, for LB and AR, ROM for the right SIJ following the unilateral stabilization group was smaller than the right SIJ of injury by 21% and 20%, respectively, with L5–S1 fixation and 12% and 17%, respectively, without L5–S1 fixation (
Figs. 4,
5).
No significant differences were observed between the ROM of the right (nonfixated) SIJ in the unilateral stabilization group and the right SIJ of the bilateral stabilization group for all loading directions (p>0.178). This finding was true for groups with and without L5–S1 fixation. However, ROM in the right SIJ of the bilateral stabilization group was smaller than right SIJ of the unilateral stabilization group, both with L5–S1 fixation, by 18% in FE, 41% in LB, and 23% in AR. Similarly, in the groups without L5–S1 fixation, the right SIJ ROM of the bilateral stabilization group compared to the unilateral stabilization group was smaller by 13% in FE, 40% in LB, and 21% in AR.
Discussion
This study quantified contralateral SIJ motion following unilateral SIJ stabilization with and without lumbosacral fixation. It was hypothesized that unilateral SIJ stabilization with L5–S1 fixation would result in hypermobility of the contralateral SIJ; however, there was no difference in SIJ ROM between fixated (left) and contralateral (right) joints in any loading direction (FE, LB, or AR). Unilateral SIJ stabilization without L5–S1 fixation did not increase contralateral SIJ ROM. Similarly, no difference in motion was observed in contralateral SIJ following unilateral stabilization compared to injury SIJ ROM and bilateral stabilization SIJ ROM. However, the fixated right SIJ of the bilateral stabilization group consistently had smaller ROM than the contralateral nonfixated right SIJ of the unilateral stabilization group in all loading directions with or without L5–S1 fixation. The reduction in ROM following bilateral stabilization compared to injury and unilateral stabilization is intuitive, as both the left and right SIJ are fixated.
Small magnitudes of SIJ ROM were observed for all loading directions, where the smallest ROM was observed in LB at approximately 0.2°. This further confirms the theory that the SIJ is inherently a stable joint [
24]; therefore, motion reduction by large magnitudes would unfeasible. The joint’s inherent stability may be a reason why no significant difference was observed between stabilization groups. Prior studies have shown a reduction in fixated joint ROM following unilateral stabilization than a destabilized state in FE, LB, and AR [
17,
25]. However, contralateral (right) nonfixated SIJ ROM following unilateral stabilization was not significantly reduced compared to intact and not significantly different to that of the right fixated SIJ of the bilateral stabilization group for all loading directions [
18], which are findings similar to that of this study. Notably, Lindsey et al. [
18] used different SIJ fixation implants than those in this study (dowels versus screws), tested in single-leg stance, and did not model a destabilized SIJ state. Despite the differences in testing methods between studies, the reported statistical findings and magnitudes (<3° in FE, <1° in LB, and <2° in AR) of contralateral SIJ ROM following unilateral stabilization were similar.
ROM reduction of the contralateral nonfixated (right) SIJ was similar to that of the fixated (left) SIJ; however, this was not as comparable to the amount of reduction of the fixated (right) SIJ, following bilateral stabilization (
Table 1). This lack of hypermobility in the contralateral nonfixated (right) SIJ compared to the fixated (left) SIJ, following unilateral stabilization may result from ROM increase at L5–S1. However, the L5–S1 ROM following unilateral stabilization without L5–S1 fixation only increased by approximately 5% in all loading directions, agreeing with previous literature that SIJ fusion minimally affects adjacent lumbar segment motion [
16]. The fusion of the fixated SIJ may affect the ROM of the contralateral SIJ; however, this study measured immediate postoperative stability. Additionally, the cutting of the iliosacral and posterior ligaments on the left-side increased motion compared to intact in both the left and right SIJ. Once the left SIJ was fixated, the motion in both the fixated (left) and nonfixated (right) SIJ decreased by approximately equal amounts in FE, LB, and AR. This may allude to the fact that SIJ ROM was mirrored between the two joints, and that stabilization of one joint does not necessarily lead to hypermobility of the contralateral joint. This study shows that biomechanics may not explain the instability found in the contralateral SIJ following unilateral stabilization, and there may be other lumbopelvic factors (demographic, clinical, or radiographic) that may lead to contralateral SIJ dysfunction.
This study’s originality includes measuring the effect of lumbosacral fusion with unilateral stabilization on contralateral SIJ ROM. Lumbosacral fusion has been known to cause SIJ degeneration with a greater incidence of degeneration in those with fusion to S1 than those with fusion to L5 [
9,
13]. The SIJ is at the level adjacent to the L5–S1 fusion, causing adjacent level effects, such as increased stress, joint mobility, or the reported SIJ degeneration [
9,
10,
13,
19]. In support of the previously mentioned studies, this study showed an increase in SIJ ROM following L5–S1 fixation compared to the injury state in FE and AR. The addition of unilateral and bilateral SIJ stabilization to L5–S1 fixation reduced ROM for both left and right SIJ to equal to or lower than intact ROM for all loading directions. Lumbosacral fixation with unilateral SIJ stabilization did not lead to hypermobility in the contralateral nonfixated (right) SIJ. Moreover, ROM at L5–S1 was reduced by at least 50% in all loading directions with L5–S1 fixation. L5–S1 fixation effects were different in FE than LB and AR. In FE, unilateral and bilateral SIJ stabilization with L5–S1 fixation resulted in more SIJ ROM than without L5–S1 fixation, whereas the opposite was true for LB and AR. This may be due to the opposing forces in the sagittal plane of the rigid L5–S1 fixation and SIJ screws [
15]. The trends were similar to the left and right SIJ, showing mirrored ROM, even with lumbosacral fixation.
This study has notable limitations. Biological processes and joint fusion were not taken into account using cadaveric specimens. The fusion of SIJ and L5–S1 may result in different ROM trends and magnitudes of the contralateral SIJ following unilateral stabilization. It is known that fusion reduces motion and can change biomechanics; therefore, caution should be used in directly applying these results to clinical settings. Additionally, an injury model was used to replicate an increase in SIJ motion that may be observed before stabilization. However, this model of cut iliosacral and posterior ligaments does not represent all physiological causes of increased SIJ mobility, and other scenarios may result in different findings. As the average age of the cadaveric specimens used in this study is 53, with this age, SIJ arthrosis may have already developed, affecting the biomechanics of the interface. Therefore, further study is necessary to look into the effects of changing lubrication of the joint on the overall biomechanical behavior of the sacroiliac with or without lumbosacral fixation. Biomechanical studies using load control protocols consider the pelvis to be fixed with motion occurring above; however, this does not consider hip dynamics and pelvic retroversion, leading to increased or decreased motion at the contralateral joint.
In the authors’ past experience, there were mixed reports for the patient outcomes. Some patients expressed decreased pain on the contralateral side after unilateral fixation, while others ended with bilateral fixation due to increased pain on the contralateral side. A suggested mechanism to explain this mixed report is that if the pain from the operated SIJ is alleviated, the contralateral SIJ does not work sufficiently as before surgery, and the contralateral SIJ may elicit less pain. However, if the contralateral side’s degeneration was accelerated due to guarded weight bearing on the index-operated SIJ postoperatively, then the contralateral SIJ may become more symptomatic. In either case, unilateral fixation is a good option for treating SIJ dysfunction. The authors hope the biomechanical evidence presented here will provide a foundation for understanding the clinical sequela of unilateral SIJ fusion. However, a clinical study with long-term follow-up is necessary to understand the clinical sequela of unilateral SIJ fusion.
Conclusions
Unilateral reconstruction stabilized both the fixated and contralateral nonfixated SIJ than the injured SIJ in FE, LB, and AR. Lumbosacral fixation with unilateral SIJ reconstruction did not lead to hypermobility of the contralateral nonfixated SIJ. Bilateral reconstruction with and without lumbosacral fixation provided the most reduction in ROM for both SIJs. This biomechanical study suggests that unilateral SIJ reconstruction with and without lumbosacral fixation does not have a negative mechanical consequence on contralateral SIJ motion; however, there may be other lumbopelvic parameters that lead to SIJ dysfunction. Thus, future research is needed to clinically determine the factors that may lead to contralateral SIJ dysfunction/pain and how unilateral fusion affects contralateral SIJ. Additionally, the amount of immediate postoperative ROM reduction needed to support SIJ fusion is yet to be determined.
Acknowledgments
The authors would like to sincerely thank Mr. Howard Whitman BA for his help with editing, revising, and submitting the manuscript.
Fig. 1.
Test set up for a range of motion measurements with 6-degrees-offreedom testing apparatus and Plexiglas markers for motion tracking.
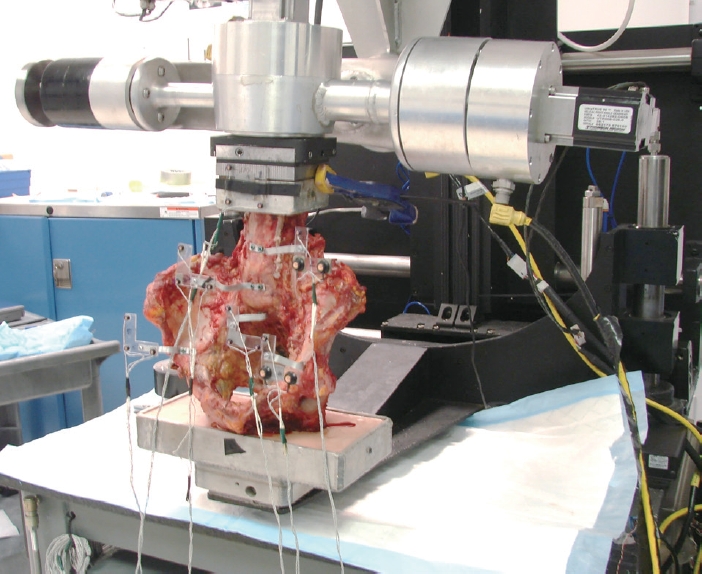
Fig. 2.
Schematic of the surgical constructs tested in this study. (A) Intact; (B) left-side posterior and iliosacral ligaments injury; (C) L5–S1 instrumentation; (D) 3 unilateral sacroiliac joint (SIJ) screws; (E) L5–S1 fixation+3 unilateral SIJ screws; (F) L5–S1 fixation+6 bilateral SIJ screws; and (G) 6 bilateral SIJ screws. Schematic not to scale.
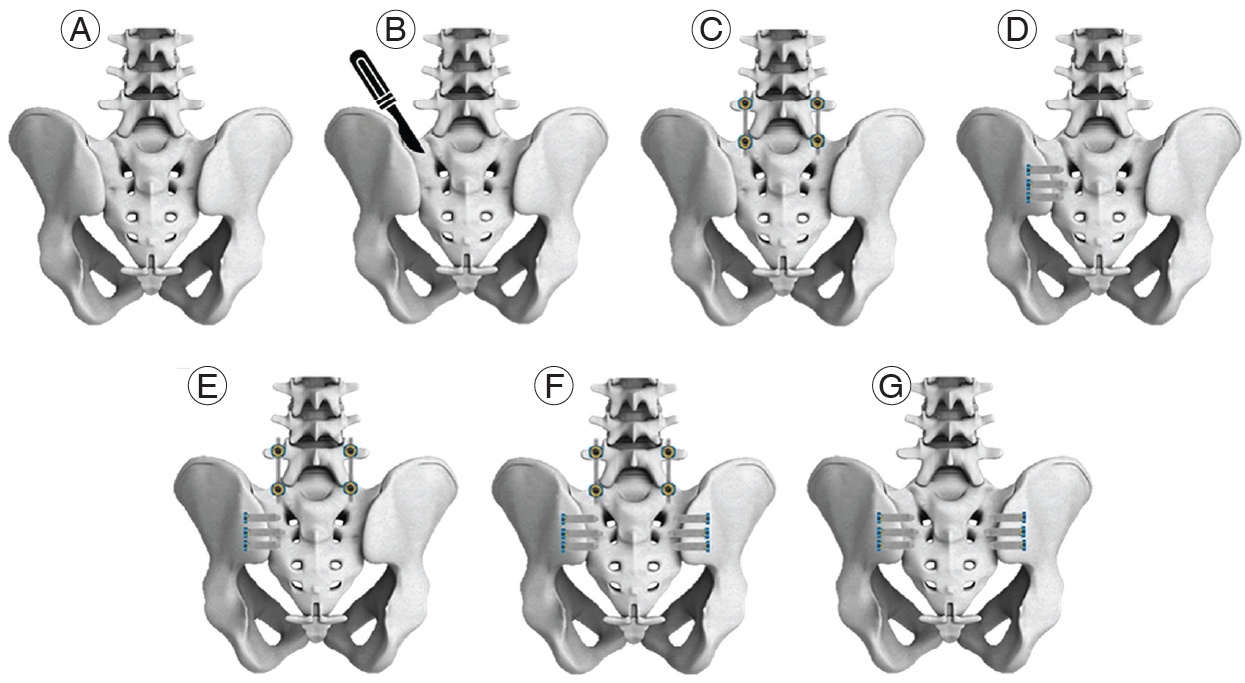
Fig. 3.
Mean±standard deviation range of motion in flexion-extension for left and right sacroiliac joint (SIJ) of intact, ligamentous injury, and SIJ reconstruction with and without L5–S1 fixation groups. No significant differences were observed (p>0.904).

Fig. 4.
Mean±standard deviation range of motion in lateral bending for left and right sacroiliac joint (SIJ) of intact, ligamentous injury, and SIJ reconstruction with and without L5–S1 fixation groups. No significant differences were observed (p>0.836).

Fig. 5.
Mean±standard deviation range of motion in axial rotation for left and right sacroiliac joint (SIJ) of intact, ligamentous injury, and SIJ reconstruction with and without L5–S1 fixation groups. No significant differences were observed (p>0.885).

Table 1.
Normalized ROM (%) relative to injury condition for all reconstructions and loading directions
|
Reconstruction groups |
Normalized ROM (% of injury)
|
Flexion-extension
|
Lateral bending
|
Axial rotation
|
|
Left |
Right |
Left |
Right |
Left |
Right |
|
L5–S1 fixation (bilateral) |
122±15.3 |
126±21.5 |
97.1±5.18 |
92.4±7.62 |
106±10.4 |
105±10.7 |
|
3 SIJ screws (left side) |
82.5±14.1 |
87.5±13.8 |
94.5±13.8 |
104±22.4 |
84.7±15.7 |
87.5±11.9 |
|
L5–S1 fixation+3 SIJ screws (left side) |
88.3±16.9 |
96.2±19.9 |
87.5±10.2 |
83.2±10.6 |
79.7±13.1 |
82.8±11.7 |
|
6 SIJ screws (bilateral) |
78.6±17.0 |
83.9±21.9 |
64.2±13.1 |
59.9±13.2 |
67.6±15.7 |
72.4±17.6 |
|
L5–S1 fixation+6 SIJ screws (bilateral) |
75.9±15.9 |
79.7±12.8 |
77.6±17.1 |
70.3±13.2 |
71.3±17.5 |
78.2±17.3 |
References
3. Sembrano JN, Polly DW Jr. How often is low back pain not coming from the back? Spine (Phila Pa 1976) 2009;34:E27–32.


4. Buchowski JM, Kebaish KM, Sinkov V, Cohen DB, Sieber AN, Kostuik JP. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J 2005;5:520–8.


5. Dreyfuss P, Dreyer SJ, Cole A, Mayo K. Sacroiliac joint pain. J Am Acad Orthop Surg 2004;12:255–65.


6. Foley BS, Buschbacher RM. Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil 2006;85:997–1006.

8. Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976) 1995;20:31–7.


9. Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine (Phila Pa 1976) 2008;33:1192–8.

10. Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech 2003;16:96–9.


11. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29:1938–44.


13. Nessim A, Cho W, Yang XA, et al. Infra-adjacent segment disease after lumbar fusion: an analysis of pelvic parameters. Spine (Phila Pa 1976) 2021;46:E888–92.

15. Dall BE, Eden SV, Cho W, et al. Biomechanical analysis of motion following sacroiliac joint fusion using lateral sacroiliac screws with or without lumbosacral instrumented fusion. Clin Biomech (Bristol, Avon) 2019;68:182–9.


17. Soriano-Baron H, Lindsey DP, Rodriguez-Martinez N, et al. The effect of implant placement on sacroiliac joint range of motion: posterior versus transarticular. Spine (Phila Pa 1976) 2015;40:E525–30.

18. Lindsey DP, Parrish R, Gundanna M, Leasure J, Yerby SA, Kondrashov D. Biomechanics of unilateral and bilateral sacroiliac joint stabilization: laboratory investigation. J Neurosurg Spine 2018;28:326–32.


19. Ivanov AA, Kiapour A, Ebraheim NA, Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine (Phila Pa 1976) 2009;34:E162–9.

20. Wilke HJ, Jungkunz B, Wenger K, Claes LE. Spinal segment range of motion as a function of in vitro test conditions: effects of exposure period, accumulated cycles, angular-deformation rate, and moisture condition. Anat Rec 1998;251:15–9.


21. Panjabi MM. Hybrid multidirectional test method to evaluate spinal adjacent-level effects. Clin Biomech (Bristol, Avon) 2007;22:257–65.


22. Goel VK, Panjabi MM, Patwardhan AG, Dooris AP, Serhan H, American Society for Testing and Materials. Test protocols for evaluation of spinal implants. J Bone Joint Surg Am 2006;88 Suppl 2:103–9.


23. Maletsky LP, Sun J, Morton NA. Accuracy of an optical active-marker system to track the relative motion of rigid bodies. J Biomech 2007;40:682–5.


24. Joukar A, Shah A, Kiapour A, et al. Sex specific sacroiliac joint biomechanics during standing upright: a finite element study. Spine (Phila Pa 1976) 2018;43:E1053–60.

25. Lindsey DP, Perez-Orribo L, Rodriguez-Martinez N, et al. Evaluation of a minimally invasive procedure for sacroiliac joint fusion: an in vitro biomechanical analysis of initial and cycled properties. Med Devices (Auckl) 2014;7:131–7.