The Use of High-Density Pedicle Screw Construct with Direct Vertebral Derotation of the Lowest Instrumented Vertebra in Selective Thoracic Fusion for Adolescent Idiopathic Scoliosis: Comparison of Two Surgical Strategies
Article information
Abstract
Study Design
This study was a retrospective case series.
Purpose
This study was designed to determine whether direct vertebral rotation (DVR) of the lowest instrumented vertebra (LIV) using a high-density (HD) construct can reduce fusion segments without increasing adverse outcomes in selective thoracic fusion (STF) for adolescent idiopathic scoliosis (AIS).
Overview of Literature
LIV DVR is used to maximize spontaneous lumbar curve correction and reduce adverse outcomes during STF for AIS. However, evidence is limited on whether LIV DVR can allow a proximally located LIV and reduce fusion segments without increasing adverse outcomes.
Methods
We reviewed consecutive patients with Lenke 1 AIS who underwent STF from 2000 to 2017. The patients were divided into two groups based on the surgical strategy used: low-density (LD) construct without DVR of the LIV (LD group) versus HD construct with DVR of the LIV (HD group). We collected data on the patient’s demographic characteristics, skeletal maturity, operative data, and measured radiological parameters in the preoperative and final follow-up radiographs. The occurrence of adding-on (AO) and coronal decompensation was also determined.
Results
In this study, 72 patients (five males and 67 females) with a mean age of 14.1±2.3 years were included. No significant differences in the demographics, skeletal maturity, and Lenke type distribution were observed between the two groups; however, the follow-up duration was significantly longer in the LD group (64.3±25.7 months vs. 40.7±22.2 months, p<0.001). The HD group had significantly shorter fusion segments (7.1±1.3 vs. 8.5±1.2, p<0.001) and a more proximal LIV level (12.1±0.9 vs. 12.7±1.0, p=0.009). In the radiological measurements, the improvement of LIV+1 rotation (Nash–Moe scale) was significantly larger in the HD group (0.53±0.51 vs. 0.21±0.41, p=0.008). AO and decompensation occurred in 7 (9.7%) and 4 (5.6%) patients in the HD and LD groups, respectively, without any significant difference between the two groups.
Conclusions
In this study, the HD group had a significantly shorter fusion level and a more proximal LIV than the LD group; however, the two groups had similar curve correction and adverse radiological outcome rates.
Introduction
The objective of the surgical treatment of adolescent idiopathic scoliosis (AIS) is to correct three-dimensional deformities and achieve a balanced spine in the coronal and sagittal planes while minimizing the number of fusion segments. Based on the Lenke classification, selective thoracic fusion (STF) is considered in patients with AIS with nonstructural lumbar curves with a bending Cobb angle of <25°C, which can be spontaneously corrected and excluded from the fusion level [1]. Possible adverse outcomes following STF include the progression of unfused lumbar curves, the occurrence of distal adding-on (AO), and decompensation [2,3]. In some studies, the level of the lowest instrumented vertebra (LIV), along with its axial rotation, has been widely discussed as an important factor associated with the aforementioned adverse outcomes [4–8].
Meanwhile, direct vertebral rotation (DVR), a surgical maneuver initially introduced to correct the thoracic hump, can be used at the LIV level to reduce adverse outcomes following STF [3,9,10]. In cases where the direction of the LIV rotation is the same as that of the thoracic apical vertebra (TAV), DVR at the LIV should be performed in the same direction as that of the TAV to prevent AO [11]. In contrast, if the rotations of the TAV and LIV are in the opposite directions, LIV DVR should be performed in the direction opposite to that of the TAV to maximize the spontaneous resolution of the compensatory lumbar curve [12,13]. In the latter case, sufficient and effective DVR of the LIV, which requires a high-density (HD) pedicle screw construct, could reduce fusion segments with a proximally located LIV [9].
Many studies have highlighted the importance of LIV DVR; however, none have examined whether it can allow a proximally located LIV and reduce fusion segments in HD constructs. Therefore, in this preliminary study, we compared the radiological outcomes of two surgical strategies: low-density (LD) construct without DVR of the LIV versus HD construct with DVR of the LIV (Fig. 1).

Illustrative cases of the two surgical strategies. (A) Low-density pedicle screw construct without lowest instrumented vertebra (LIV) direct vertebral rotation (DVR). A 13 year-old-girl with a Lenke type 1B curve whose LIV was one vertebra below the last touched vertebra (LTV) (LTV+1). (B) High-density pedicle screw construct with LIV DVR. A 13-year-old girl with a slightly larger Lenke type 1B curve whose LIV was the LTV. Central sacral vertical lines are shown as white lines.
Materials and Methods
1. Study design and participants
This study was approved by the institutional review board of Seoul National University Hospital (IRB no., 2111-121-1273), and informed consent from individual patients was waived due to the retrospective design of the study. We retrospectively reviewed all consecutive patients with AIS who underwent STF using pedicle screw instrumentation at Seoul National University Hospital between January 2000 and December 2017. In this study, only patients with Lenke type 1 curve who were followed up until 2 years postoperatively and beyond skeletal maturity were included. We excluded those with a curve within which the presumed LIV had the same direction of rotation as that of the TAV on the preoperative radiographs. These patients were excluded because they required a distally located LIV to avoid AO, and the direction and role of the LIV DVR are different from those of their counterparts, as previously described [14]. As a result, we included only patients with a curve within which the presumed LIV had no rotation or rotated in the direction opposite to the TAV, and the suggested direction for the LIV DVR was also the opposite to the direction of the TAV DVR. Patients who underwent thoracoplasty, anterior release, or osteotomy for deformity correction were also excluded from this study.
2. Two surgical strategies
Two surgeons (H.K. and C.K.L.) performed all surgeries under the same principles and techniques, including the material of the rod used (titanium alloy) and its diameter (5.5 mm). However, regarding the implant density (ID) and LIV DVR, two surgical strategies were applied (Fig. 1). First, until 2013, the LD construct without LIV DVR was primarily used (LD group). After inserting the first rod on the concave side, the rod was derotated and fixed at the proximal end. Following the insertion and proximal fixation of the second rod on the convex side, DVR of the TAV was performed in the direction that corrects the thoracic hump, and both rods were fixed at all screws, as described in a previous study [15]. Typically, the stable vertebra (SV) or SV-1 was selected as the LIV, and no LIV DVR was performed in these cases.
From 2013, the second strategy—HD construct with the LIV DVR—was used (HD group). Pedicle screws were inserted into every pedicle included in the fusion level, except for the dysplastic pedicles, in which pedicle screw insertion was impossible. Rod derotation and TAV DVR were performed in the same manner as in the first strategy. However, additional LIV DVR was performed in the direction opposite to the TAV DVR (Fig. 1). The LIV was rotated beyond the neutral rotation to maximize spontaneous lumbar curve correction, particularly in Lenke 1B and 1C patients. In the HD group, the last touched vertebra (LTV), defined as the last vertebra touching the central sacral vertical line (CSVL) [2], or LTV-1 was chosen as the LIV. The selection of a proximally located LIV was possible because of the corrective effect of the LIV DVR. In both strategies, the main intent of LIV selection was to preserve as many mobile segments as many as possible (Fig. 2).
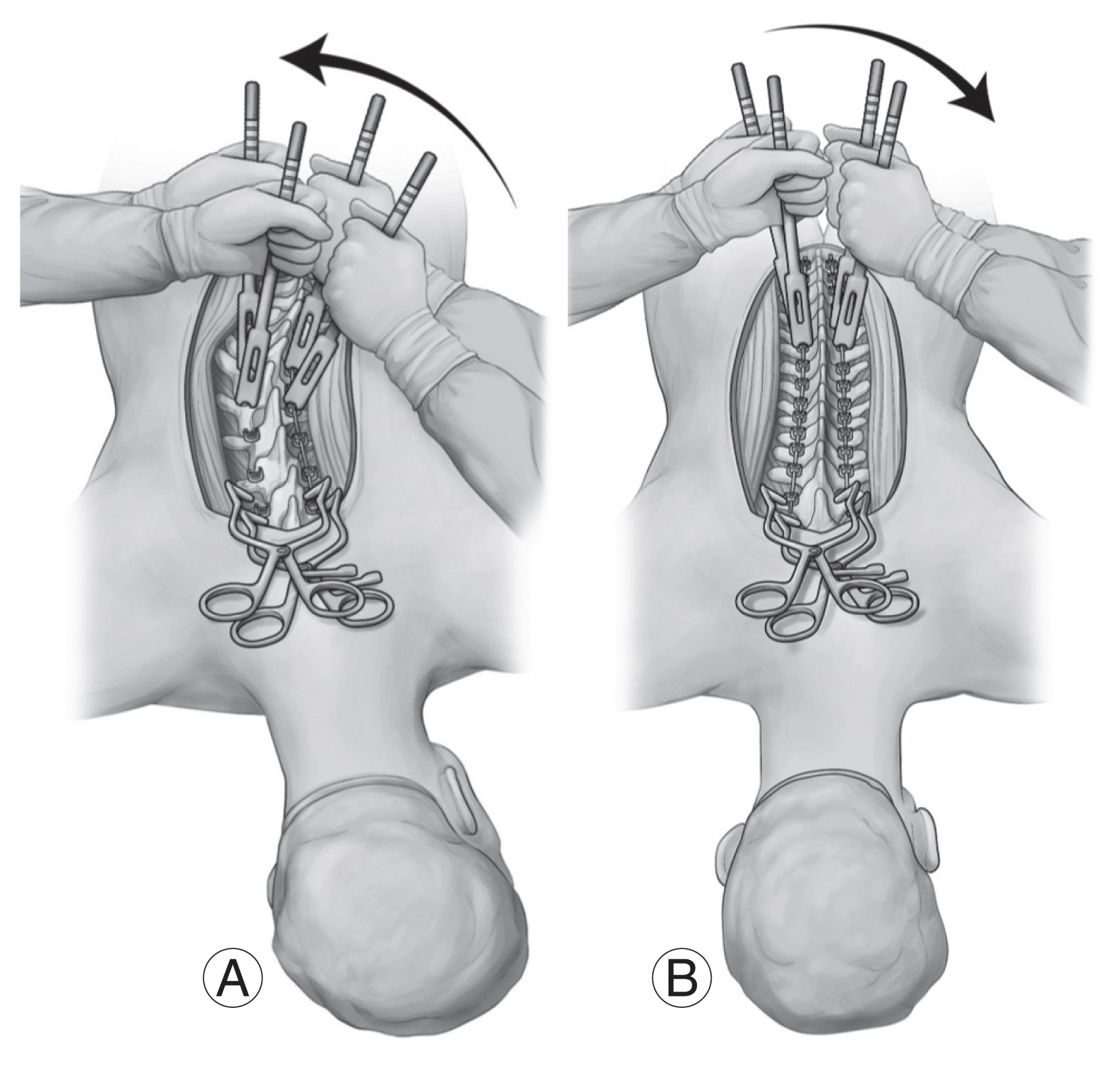
(A) After rod derotation, the pedicle screws at the proximal and distal ends are temporarily but firmly fixed to the rod. Next, direct vertebral rotation of the apical vertebrae is performed in the direction that neutralizes the axial rotation. (B) After apical vertebrae are firmly fixed to the rod, the distal pedicle screws are loosened and rotated in the direction opposite to the thoracic apical vertebrae.
3. Data collection and radiological measurement
We retrospectively collected data on patient demographics, skeletal maturity (Risser grade), and operative data (i.e., the number of fusion segments, pedicle screws, ID, and level of the LIV). The ID was defined as the total number of pedicle screws inserted divided by the fusion levels. Whole-spine anteroposterior radiographs were reviewed preoperatively and during the last follow-up, and the following radiological parameters were measured by one of the authors, who was unaware of the differences between the two surgical strategies. The magnitudes of the main thoracic and compensatory lumbar curves were measured using the Cobb method. The translations of the TAV, lumbar apical vertebra (LAV), and LIV from the CSVL were measured. Coronal balance was assessed by measuring the distance between the C7 plumb line (C7PL) and the CSVL. Additionally, the LIV tilt angle (the angle between the inferior endplate of the LIV and horizontal line) and LIV disk angle (the angle between the inferior endplate of the LIV and the superior endplate of the LIV+1) were also measured [16]. Finally, the rotations of the TAV, LAV, and LIV+1 were assessed using the Nash–Moe classification [17]. For the preoperative radiographs, the parameters of the LIV and LIV+1 were measured in the presumed vertebrae for instrumentation.
The occurrence of distal AO and coronal spinal decompensation were determined based on the final follow-up radiographs. Distal AO was defined as an increase in the number of vertebrae included in the primary curve distally, combined with either an increase of more than 5 mm in the translation of the LIV+1 from the CSVL or an increase of more than 5°C in the LIV disk angle [5]. Coronal decompensation was defined as a C7PL-CSVL distance of >2 cm [4].
4. Statistical analysis
For group comparisons, continuous variables were compared using Student t-test, and categorical variables were compared using the χ2 test. A paired t-test was used to examine the interval changes in the radiological parameters. All statistical analyses were performed using IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA). Statistical significance was set at p<0.05.
Results
From January 2000 to December 2017, 215 patients with Lenke type 1 AIS curves underwent surgical correction at Seoul National University Hospital. Among these patients, 72 patients (five males and 67 females) with a mean age of 14.1±2.3 years who fulfilled the inclusion criteria were included in this study. The comparison of the baseline characteristics and operative data between the LD (n=53) and HD (n=19) groups is summarized in Table 1. The HD group tended to be older with a higher Risser grade than the LD group; however, the differences were not statistically significant. Furthermore, no significant differences in the distribution of the Lenke types and levels of the LTV were observed between the two groups.
Regarding the operative data, the HD group showed significantly shorter fusion segments (7.1±1.3 versus 8.5±1.2, p<0.001) and more proximal LIV level (12.1±0.9 versus 12.7±1.0, p=0.009) than the LD group. In the HD group, 78.9% of patients had LTV as the LIV, whereas, in the LD group, 50.9% of patients had LTV+1 as the LIV (p=0.008). In the HD group, the ID was significantly higher (1.9±0.2 versus 1.0±0.1, p<0.001) and more screws were used (14.9±2.2 versus 9.2±1.3, p<0.001) (Table 1).
We used only the follow-up data of the LD group collected up to postoperative 8 years (96 months) for the radiological assessment, which was the longest follow-up period in the HD group. The truncated follow-up period of the LD group was 64.3±25.7 months, and the mean follow-up period of the HD group was 40.7±22.2 months. No significant differences—both preoperatively and postoperatively—in the following parameters were observed between the two groups: the Cobb angle of the main thoracic and compensatory lumbar curves, the LIV tilt and disk angles, the translations of the TAV and LAV, and the coronal balance (C7PL–CSVL distance) (Table 2).
For the axial vertebral rotation, no significant differences in the TAV and LAV rotations were found between the two groups (Table 3). Although the rotation of the LIV+1 also did not show any difference between the preoperative and postoperative radiographs, the improvement in the LIV+1 rotation (postoperative–preoperative difference) was significantly larger in the HD group (0.53±0.51 versus 0.21±0.41, p=0.008) than in the LD group. Furthermore, a significantly larger proportion of patients in the HD group showed an improvement in the axial rotation of more than 1 grade on the Nash–Moe scale (52.6% versus 20.8%, p=0.009).
Regarding the adverse outcomes, AO occurred in seven patients (9.7%)—six patients in the LD group and one patient in the HD group—of the entire study cohort (n=72); the difference was not statistically significant (p=0.444). The occurrence of AO stratified by the level of the LIV is shown in Table 4. Coronal decompensation occurred in four patients (5.6%) of the entire study cohort; no significant difference in this occurrence was observed between the two groups (p=0.948).
Discussion
The axial rotation of the vertebral body is a key feature of a three-dimensional AIS deformity. DVR can be used to correct scoliosis by rotating the vertebral body in the axial plane. DVR is most commonly performed at the deformity apex to reduce the thoracic or lumbar hump [10]. However, depending on the direction, it can also be used at the LIV in STF to maximize the spontaneous resolution of the compensatory lumbar curve or avoid AO [3,11]. This study was designed to answer the following question: will LIV DVR using an HD pedicle screw construct allow a proximally located LIV and shorter fusion segments without causing more adverse outcomes?
This study compared patients who underwent AIS correction under the two surgical strategies: using an LD construct without LIV DVR (LD group) versus an HD construct with LIV DVR (HD group). The HD group had significantly shorter fusion segments with a more proximally located LIV than the LD group (Table 1). Although the fusion was shorter in the HD group, no statistically significant differences in the thoracic and lumbar curve correction (Cobb angles and translations) and the LIV tilt and disk angles were observed between the two groups (Table 2). Furthermore, no significant increase in the occurrence of adverse surgical outcomes, such as AO and coronal decompensation, was observed in the HD group (Table 4). These comparable results in the HD group, despite the shorter fusion length, could be because of the improvement in the LIV+1 rotation (postoperative–preoperative difference), which was more significant in the HD group (0.53±0.51 versus 0.21±0.41, p=0.008) than in the LD group.
Because of the design of this study, the component that is more responsible for the improved correction of the LIV+1 rotation in the HD group is unclear: the HD construct or LIV DVR. Demura et al. [13] reported that the improvement in axial rotation of the lumbar spine in computed tomography (CT) images correlated with the postoperative thoracic curve magnitude. Additionally, in a study by Kim et al. [9], the rotation of the distal end vertebra significantly improved in patients who underwent DVR at the TAV compared with that in patients who did not. These results indicate that thoracic curve correction itself can improve the axial rotation of the LIV and lumbar spine. Therefore, one should compare cases who underwent LIV DVR with those who did not but with a similar ID to examine the effect of LIV DVR alone on the LIV+1 rotation. This was impossible in this study because effective LIV DVR cannot be performed using LD constructs. Moreover, we performed LIV DVR in all patients with HD constructs to maximize the correction of rotation while attempting to reduce fusion segments. LIV DVR was a rationale for applying HD constructs, which may increase the patient’s cost and the risk of implant-related complications (e.g., screw malposition) in our group.
Regarding the optimal ID in AIS surgery, controversies exist in the literature. Some authors have reported that a higher ID resulted in better coronal [18,19], sagittal [20], and axial corrections [21]. Others have shown no association between the ID and deformity correction [22–24]. In their study, Mac-Thiong et al. [25] reported that the addition of fixation anchors did not significantly improve the main curve correction when the ID reached 70%. Additionally, several studies, including a systemic review by Luo et al. [26], have shown that LD constructs were associated with a reduced operation time, less blood loss, and decreased hospital costs while maintaining similar radiological and clinical outcomes [27,28]. However, there is limited evidence on the association between the ID and fusion level, in which the HD group had a shorter fusion level [29].
In this study, the HD group had a significantly shorter fusion length (7.1±1.3 versus 8.5±1.2, p<0.001) and a more proximally located LIV (12.1±0.9 versus 12.7±1.0, p=0.009), while maintaining similar radiological outcomes (spontaneous lumbar curve correction and occurrence of adverse outcomes). However, note that the HD group had an ID of 1.9, which is higher than what many authors have suggested [30]. Furthermore, the HD group used an average of 5.7 more screws per case, which should have increased the in-hospital cost. Verifying whether the benefit of reducing an average of 1.4 fusion segments using HD constructs combined with LIV DVR justifies the increased cost and risk of complications related to additional pedicle screw placement is beyond the scope of this study.
Regarding the adverse surgical outcomes, the rate of AO was 9.7% (seven of the 72 patients) in this study, which was lower than the AO rates (13.8%–51.1%) following STF reported in previous studies [2,5–7,31,32]. Reports have shown high rates of AO because most studies only examined Lenke type 1A curves, in which distal AO most frequently occurs, and included hybrid constructs (pedicle screw and hooks) with inferior correction powers than all-pedicle screw constructs. In contrast, 65.3% of the patients in this study had Lenke type 1B or 1C curves, and we applied all-pedicle screw constructs to all patients. Furthermore, we excluded patients with a curve, in which the presumed LIV had the same direction of rotation as the TAV in the preoperative radiographs, as they are prone to develop AO after STF. All these factors have resulted in a low AO rate in this study.
In the HD group, only one of the 19 patients (5.3%) had AO. A slightly higher age, greater skeletal maturity, and a significantly shorter follow-up period (40.7±22.2 months versus 64.3±25.7 months, p<0.001) than the LD group may have contributed to the low AO rate in the HD group. However, note that six patients who had AO in the LD group had a similar mean age at operation (14.0±0.7 years) and Risser grade (3.3±1.1) as the entire cohort. As for the LIV, although the LIV level was not significantly associated with the occurrence of AO in this study, it should be emphasized that one of the four patients (25.0%) who had the LTV-1 as the LIV experienced AO, indicating that the LTV-1 is too proximal to be selected as the LIV, even in the case of HD constructs and LIV DVR. Future studies with a larger sample size should be conducted to verify these issues.
Coronal decompensation occurred in four of the 72 patients (5.6%) included in this study. Studies have identified the risk factors of coronal decompensation following STF for Lenke type 1 AIS, which includes lumbar modifier C and a distally placed LIV [33,34]. A similar tendency of decompensation occurring in patients with a distally placed LIV in Lenke type 1B and 1C curves was also observed in this study (Table 4). Therefore, not selecting an LIV too distally beyond the SV is important to avoid coronal decompensation following STF, regardless of the ID, particularly in patients with lumbar modifier C.
This study has several limitations. First, because of the retrospective nature of this study, we cannot rule out selection bias relative to the inclusion and exclusion criteria. Second, the sample size in the HD group was too small to draw statistically significant results. A follow-up study with a larger sample size and a longer follow-up period is necessary. Third, because this was a radiological study, patient-reported outcomes, such as the Scoliosis Research Society-22 questionnaire, were not evaluated. Fourth, we used the Nash–Moe scale to assess the vertebral rotation, which can be less accurate than the measurements in the axial CT images. Fifth, the follow-up periods of the two groups significantly differed, even though we truncated the follow-up period of the HD group. Finally, as previously mentioned, we could not determine the sole effect of LIV DVR, irrespective of the ID in this study design. Nevertheless, the results of this study suggest that HD pedicle screw constructs combined with LIV DVR can reduce fusion segments during STF for AIS without further increasing the occurrence of adverse surgical outcomes compared with LD constructs without LIV DVR.
Conclusions
In this preliminary study, we compared two surgical strategies (LD construct without the LIV DVR versus HD construct with the LIV DVR) in patients with Lenke type 1 AIS who underwent STF. The HD group had a significantly shorter fusion level and more proximally located LIV than the LD group; however, the two groups had similar curve correction and adverse radiological outcome rates. HD constructs combined with LIV DVR can reduce fused segments without further increasing the occurrence of adverse surgical outcomes in patients with AIS undergoing STF.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: HK, SYC, BSC; methodology: HK, SYC, JHK; validation: HK, SM, CKL; formal analysis: SYC, CKL, BSC; investigation: HK, SYC, JHK; resources: SM, CKL; data curation: HK, SM, BSC; writing–original draft preparation: HK, SYC, BSC; writing–review and editing: all authors; visualization: JHK, SM, CKL; and supervision: BSC. All authors have read and agreed to the published version of the manuscript.




