Serotonin Reuptake Inhibitor Increases Pseudarthrosis Rates in Anterior Cervical Discectomy and Fusions
Article information
Abstract
Study Design
Retrospective cohort.
Purpose
To determine (1) the effects of serotonin reuptake inhibitors in pseudarthrosis rates after anterior cervical decompression and fusion (ACDF) and (2) to identify patient-reported outcome measures in patients taking serotonin reuptake inhibitors.
Overview of Literature
Recent literature suggests that selective serotonin reuptake inhibitors (SSRIs) may inhibit fracture healing via downregulation of osteoblast differentiation. Spinal fusion supplementation with osteoblast-rich substances enhances spinal fusion, thus SSRIs may be detrimental.
Methods
Patients with 1-year postoperative dynamic cervical spine radiographs following ACDF were grouped into serotonin reuptake inhibitor prescriptions (SSRI, serotonin-norepinephrine reuptake inhibitor [SNRI], or tricyclic antidepressant [TCA]) and no prescription (atypical antidepressant or no antidepressant). Pseudarthrosis was defined as ≥1 mm interspinous process motion on dynamic radiographs. Logistic regression models were controlled for confounding to analyze pseudarthrosis rates. Alpha was set at p-values of <0.05.
Results
Of the 523 patients who meet the inclusion criteria, 137 (26.2%) were prescribed an SSRI, SNRI, or TCA. Patients with these prescriptions were more likely to have pseudarthrosis (p=0.008) but not a revision surgery due to pseudarthrosis (p=0.219). Additionally, these patients had worse 1-year postoperative mental component summary (MCS)-12 (p=0.015) and Neck Disability Index (NDI) (p=0.006). The multivariate logistic regression analysis identified SSRI/SNRI/TCA use (odds ratio [OR], 1.82; 95% confidence interval [CI], 1.11–2.99; p=0.018) and construct length (OR, 1.91; 95% CI, 1.50–2.44; p<0.001) as pseudarthrosis predictors. A SSRI/SNRI/TCA prescription was a revision surgery predictor due to adjacent segment disease on univariate analysis (OR, 2.51; p=0.035) but not on multivariate logistic regression analysis (OR, 2.24; p=0.10).
Conclusions
Patients taking serotonin reuptake-inhibiting antidepressants are at increased risk of worse postoperative outcome scores, including NDI and MCS-12, likely due to their underlying depression. This may contribute to their greater likelihood of having adjacent segment surgery. Additionally, preoperative use of serotonin reuptake inhibitors in patients undergoing an ACDF is a predictor of radiographic pseudarthrosis but not pseudarthrosis revision.
Introduction
Anterior cervical discectomy and fusion (ACDF) is one of the most common cervical spinal procedures, accounting for approximately 80% of all cervical spinal surgeries [1]. Current estimates expect an increased ACDF prevalence by 13.3% in 2020–2040 [2,3]. The popularity of ACDFs can be attributed to excellent patient satisfaction scores and improvements in both short- and long-term clinical outcomes [3,4].
ACDFs have a favorable complication profile; however, pseudarthrosis is one of the most commonly identified complications with rates ranging from 3%–20% in 1-level procedures to 50% in 4-level procedures [5,6]. Most patients remain asymptomatic, but symptomatic pseudarthrosis or adjacent segment disease (ASD) are two of the leading causes of revision surgery following ACDF, resulting in a combined revision rate of 15% with an average follow-up duration of 31 months [7]. The annual incidence of ASD is low at 2.2%, which leads to clinically symptomatic ASD in 22% of patients at 10-year follow-up [8]. Therefore, identifying the risk factors that contribute to pseudarthrosis or ASD is a critical necessity due to the high surgical volume of ACDF procedures.
Previous literature has suggested a depression diagnosis that leads to worse mental and physical components of patient-reported outcome measures (PROMs) following ACDF [9]. One rationale for the link between depression and inferior postoperative PROMs is a greater complication profile in this population [10,11]. A plausible explanation for this relationship is medication-related. Serotonin reuptake-inhibiting drugs can be prescribed as an alternative method for pain management; however, these drugs are primarily given to patients with depression [12].
Basic science research has identified a potential mechanism where selective serotonin reuptake inhibitors (SSRIs) inhibit osteoblast differentiation leading to reduced mineralization in an animal fracture model [13]. Combined with clinical research that identifies the role of SSRIs in increased bleeding and pseudarthrosis rates in patients with ACDF, this provides a compelling rationale for a link between depression and inferior PROMs [13–15]. Therefore, we hypothesized that patients with serotonin reuptake-inhibiting drug prescriptions (SSRIs, serotonin-norepinephrine reuptake inhibitors [SNRIs], and tricyclic antidepressants [TCAs]) would have increased rates of pseudarthrosis leading to inferior PROMs compared to patients without serotonin reuptake-inhibiting drug prescriptions.
Materials and Methods
1. Inclusion criteria
This study was approved by the Institutional Review Board at Thomas Jefferson University (Control #19D.508) with exempt status from requiring informed consent due to its retrospective design and minimal risk to subjects. Upon obtaining approval, all patients >18 years of age with preoperative and postoperative flexion-extension radiographs who underwent primary 1- to 4-level ACDF at Thomas Jefferson University from 2010 to 2019 were retrospectively identified. Patients who underwent index ACDF for a revision procedure, utilized a combined anterior/posterior approach, with a concomitant cervical corpectomy, or indicated in trauma, infection, or neoplasm settings were excluded.
2. Data extraction
Patient demographics and surgical characteristics were collected through a Structured Query Language search and manual chart review of electronic medical records. Dual-energy X-ray absorptiometry scans were utilized to identify patients with osteoporosis, defined by a T-score of ≤−2.5. Preoperative antidepressant prescriptions were recorded for each patient and classified by the following criteria: SSRI: citalopram, escitalopram, fluoxetine, paroxetine, and sertraline; SNRI: desvenlafaxine, duloxetine, venlafaxine; TCA: amitriptyline, doxepin, and nortriptyline; and atypical antidepressant: bupropion, lurasidone, mirtazapine, quetiapine, trazodone, and ziprasidone. PROMs were retrospectively collected through our institution’s prospectively collected database (OBERD, Columbia, MO, USA) and were included at the preoperative, 3-month postoperative, and 1-year postoperative time points. The extracted PROMs included the Visual Analog Scale for neck pain (VAS neck) and arm pain (VAS arm), the Neck Disability Index (NDI), the modified Japanese Orthopedic Association Scale (mJOA), and the mental and physical component summary scores of the Short Form 12 (SF-12) Health Survey (MCS-12 and PCS-12, respectively). The change in each PROM score (Δ) at the 3-month and 1-year postoperative point was calculated by subtracting the preoperative from the postoperative values. A recovery ratio (RR) was calculated for the 3-month and 1-year postoperative point for each PROM from the following formula: [Δ PROM/(optimal PROM–preoperative PROM)]. Optimal scores for each PROM were defined as VAS neck and VAS arm of 0 points, mJOA of 18 points, and SF-12 MCS/PCS of 100 points.
3. Radiographic evaluation
Postoperative dynamic radiographs were reviewed by a single reviewer through our institution’s Picture Archiving and Communication System (Sectra AB, Linköping, Sweden). The distance (in millimeters) between the superior and inferior spinous process at each ACDF level was measured on postoperative flexion and extension radiographs. Radiographic fusion was defined as <1 mm of interspinous motion between each instrumented level and ≥4 mm of motion at any adjacent unfused level following the guidelines published by the Cervical Spine Research Society Special Project Committee [16]. ASD was defined as any patient with symptomatic postoperative pain and supra-adjacent or infra-adjacent progressive listhesis or degenerative disk disease, which resulted in a revision procedure.
4. Surgical procedure
All surgeons at our institution use a standard Smith-Robinson approach. A combination of sharp and blunt dissection is performed until reaching the longus colli muscle, which is subperiosteally elevated with electrocautery so retractors can be placed posterior to the muscle for appropriate disk space and endplate visualizations. The posterior longitudinal ligament is taken and the pedicles are skeletonized. The cartilaginous endplate is then removed to optimize fusion rates. Machined allograft was used as the interbody spacer in 86% of the cases, but some surgeons alternatively use poly-ether-ether-ketone (PEEK) (5%) or titanium cages (9%) with local autograft, when available, and allograft chips. Following anterior cervical plate and locking screw placement, the wound is irrigated and intraoperative lateral cervical radiographs are taken to confirm instrumentation positioning.
5. Statistical analysis
Descriptive statistics, including mean and standard deviation, were used to record patient demographics, surgical characteristics, and surgical outcomes. Continuous and categorical variables were analyzed using independent t-tests and Pearson’s chi-square tests, or the corresponding non-parametric test, respectively. Multiple logistic regression models were developed to measure the effect of patient demographics, preoperative antidepressant medication usage, and surgical characteristics on the likelihood of radiographic fusion and revision surgery for ASD after the index ACDF. R software ver. 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) was used for all data analysis. Statistical significance was set at p-values of <0.05.
Results
1. Patient demographics
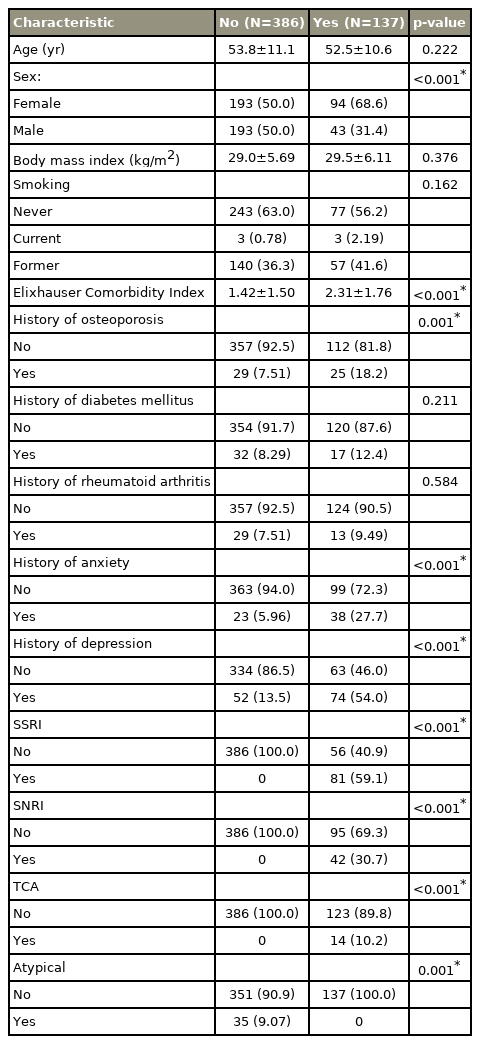
Of the 523 patients who met the inclusion criteria, 137 patients (26.2%) were taking serotonin reuptake-inhibiting antidepressants. Of the 137 patients, 81 (59.1%) were prescribed SSRI, 42 (30.7%) SNRI, and 14 (10.2%) TCA. Patients taking serotonin reuptake-inhibiting antidepressants were significantly more likely females than males (N=94 [68.6%] versus N=43 (31.4%), p<0.001), with a greater Elixhauser Comorbidity Index (2.31±1.76 versus 1.42±1.50, p<0.001), osteoporosis (18.2% versus 7.5%, p=0.001), and anxiety (p<0.001) or depression (p<0.001) diagnosis. The remaining patient demographics were not significantly different (Table 1).
2. Surgical characteristics
A significantly higher proportion of patients were prescribed SSRI, SNRI, or TCA versus those who did not undergo a multilevel ACDF (78.8% versus 67.1%, p=0.045). No significant differences were found in implant composition (p=0.926), length of clinical follow-up (21.4±11.6 versus 21.4±11.5 months, p=0.910), 90-day all cause readmission (2.19% vesus 0.26%, p=0.057), subsidence rates (0.8±1.13 versus 0.8±1.13, p=0.718), or rate of revision surgery due to pseudarthrosis (7.30% versus 4.15%, p=0.219) between the patients with and without SSRI/SNRI/TCA prescriptions. However, a significantly greater pseudarthrosis rate (46.7% versus 33.4%, p=0.008) and rate of revision surgery due to ASD (8.76% versus 3.63%, p=0.032) were found in patients with and without SSRI, SNRI, or TCA prescriptions (Table 2).
3. Patient-reported outcome measures
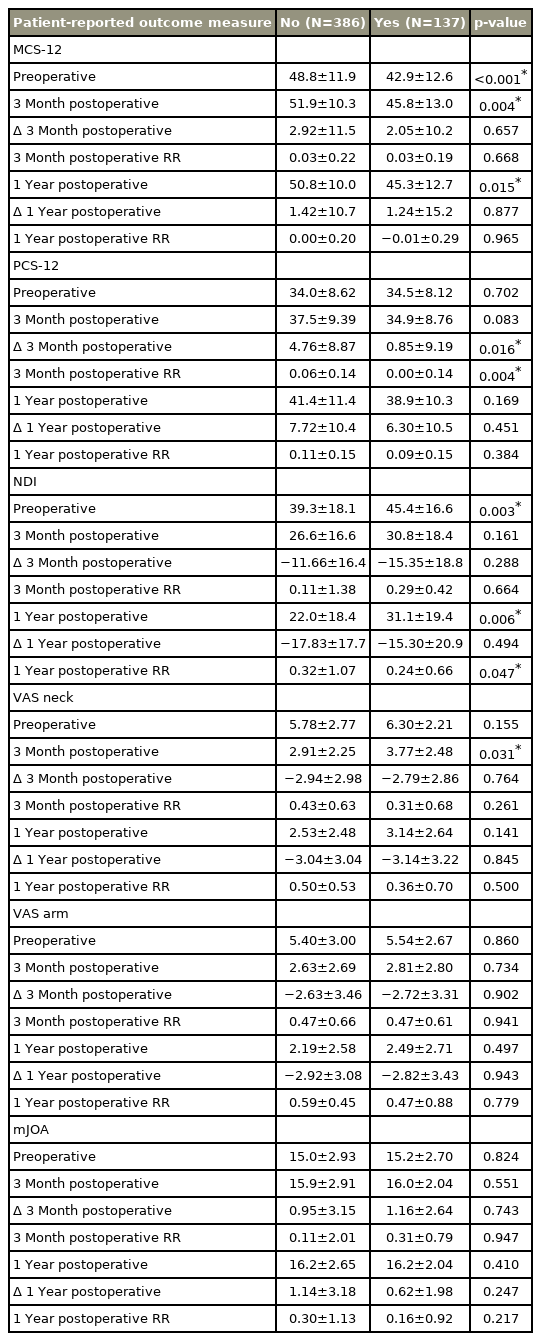
A preoperative prescription for a SSRI, SNRI, or TCA was associated with an inferior preoperative (42.9 versus 48.8, p<0.001), 3-month postoperative (45.8 versus 51.9, p=0.004), and 1-year postoperative MCS-12 (45.3 versus 50.8, p=0.015), but did not significantly affect ∆MCS-12 at 3-months (2.05 versus 2.92, p=0.657) or 1-year (1.24 versus 1.42, p=0.877). The preoperative (34.5 versus 34.0, p=0.702) and 3-month postoperative PCS-12 (34.9 versus 37.5, p=0.083) were not significantly different, the ∆PCS-12 at 3-months (0.85 versus 4.76, p=0.016) and the PCS-12 RR at 3-months (0.00 versus 0.06, p=0.004) did demonstrate a significant decrease in patient improvement with a preoperative SSRI, SNRI, or TCA prescription. These differences did not persist at 1-year for the ΔPCS-12 (6.30 versus 7.72, p=0.451) or PCS-12 RR (0.09 versus 0.11, p=0.384). The preoperative NDI (45.4 versus 39.3, p=0.003), 1-year postoperative NDI (31.1 versus 22.0, p=0.006), and NDI RR at 1-year (0.24 versus 0.32, p=0.047) demonstrated worse outcomes for the SSRI, SNRI, or TCA group. VAS arm and VAS neck analyses revealed a significantly worse outcome only in the 3-month postoperative VAS neck (3.77 versus 2.91, p=0.031) for the SSRI, SNRI, and TCA group (Table 3).
4. Multiple logistic regression analysis
The analyses of radiographic fusion as the dependent variable revealed SSRI/SNRI/TCA use (odd ratio [OR], 1.82; 95% confidence interval [CI], 1.11–2.99; p=0.018) and construct length (OR, 1.91; 95% CI, 1.50–2.44; p<0.001) as radiographic pseudarthrosis predictors. Age (OR, 1.02; 95% CI, 1.00–1.04), male sex (OR, 1.33; 95% CI, 0.90–1.99), body mass index (OR, 0.97; 95% CI, 0.93–1.00), current smoking status (OR, 4.03; 95% CI, 0.70–32.26), osteoporosis (OR, 0.79; 95% CI, 0.41–1.49), and atypical antidepressant prescriptions (OR, 1.44; 95% CI, 0.62–3.26) were not identified as independent pseudarthrosis predictors (Table 4).
The analyses of revision surgery for ASD as the dependent variable revealed that SSRI/SNRI/TCA use (OR, 2.24; 95% CI, 0.84–5.84; p=0.10) is not an independent predictor for increased revision surgery rates for ASD but for increased age (OR, 0.96; 95% CI, 0.92–0.99; p=0.030) did. No other independent variables were revision for ASD predictors (Table 5).
Discussion
ACDF is one of the most successful orthopedic procedures with previous literature suggesting that they outperform total hip and total knee arthroplasty in the physical and mental components of the 36-item Short Form Survey (SF-36) [17]. However, variability in patient-reported outcomes continues to persist between patients with and without depression who undergo ACDF [9]. Identifying the causation of inferior PROMs in this population is imperative, given that an estimated 13.2% of United States adults are prescribed antidepressant medications, making them the third most commonly prescribed drug class [18]. Our study suggests that serotonin reuptake-inhibiting antidepressants are one contributing factor to inferior postoperative patient-reported outcomes in patients undergoing ACDF due to a higher pseudarthrosis rate. However, our data suggest that antidepressant use alone is not the sole cause of inferior PROMs since the RR between our two groups was significantly worse only for NDI at 1-year.
Over the last decade, a growing body of literature has emerged documenting SSRIs’ inhibition of osteoblast differentiation leading to impaired fracture healing [19]. Additionally, SSRI imparts an elevated risk of future fractures [20], which is hypothesized from an increased rate of osteoblast apoptosis leading to approximately 80% reduction in osteoblast viability based on an in vitro model [21]. Osteoblasts are an integral factor in obtaining an osseous spinal fusion, thus serotonin reuptake-inhibiting drugs are one potential causative agent leading to pseudarthrosis [22]. Our study findings support our hypothesis that serotonin reuptake-inhibiting drugs hinder spinal fusion, potentially through osteoblast inhibition; however, this requires confirmation through well-designed translational research, including animal models.
Patient-reported outcomes have become integral in determining patient improvements following surgery. A history of depression is believed to cause worse preoperative and postoperative PROMs in patients undergoing spinal surgery, but most studies have shown similar degrees of improvement following surgery [9,23]. We identified inferior preoperative and postoperative PROMs in patients taking a serotonin reuptake-inhibiting drug compared to those who do not. However, differences in the degree of improvement and RRs revealed significant changes between groups only in the 3-month PCS-12 and 3-month RR for PCS-12, as well as the 1-year NDI and 1-year recovery ratio for NDI, which were worse in the serotonin reuptake-inhibiting group. A previous retrospective study by Jenkins et al. [24] demonstrated a greater magnitude of depression based on the Patient Health Questionnaire-9 correlated with inferior PCS-12 scores at 3 months but not 1 year. We demonstrated similar findings. Serotonin reuptake-inhibiting drugs may result in worse 3-month PCS-12 scores due to delayed construct union; however, this was not confirmed by our data. Additionally, our data does strongly suggest depression alone, and the antidepressant medication is not the major contributing component of worse preoperative and postoperative PROMs based on the minimal differences in the 3-month and 1-year recovery ratios.
In addition to worse preoperative and postoperative PROMs, patients with depression are well established to have an increased complication profile after ACDF procedures due to an elevated incidence of ASD, 90-day readmissions, and revision surgery within 2 years [25]. This results in an estimated increase in healthcare costs by $4,471 over 2 years following ACDFs [25]. As healthcare continues to transition to bundled payments, further research targeted at identifying a concrete link between serotonin reuptake-inhibiting drugs and its contribution to elevated complication rates and escalating healthcare expenditures is critical.
The US Food and Drug Administration approved the first SSRI, fluoxetine, in 1987, and the first atypical antidepressant was approved 2 years later when bupropion was approved in 1989 [26]. Instead of targeting serotonin reuptake, bupropion dually targets norepinephrine and dopamine reuptake, giving it unique antidepressant properties [27]. SRIs were associated with greater rates of revision surgery due to ASD on univariate analysis; however, patients taking atypical antidepressants had similar ASD and pseudarthrosis rates as those who were not prescribed these medications. Therefore, atypical antidepressants are a potentially interesting avenue for future research, as switching antidepressant therapy to an atypical antidepressant before ACDFs may decrease revision surgery rates and improve patient-reported outcomes. Although outside the scope of our study, an elevated risk of bleeding should be noted in patients taking either SSRIs or bupropion due to drug-induced platelet inhibition [28]. Additionally, no formal guidelines exist for SSRI or bupropion cessation before ACDF procedures, due to concerns including depression relapse and discontinuation syndrome [29].
The higher ASD rate observed on univariate analysis deserves further comment. Patients taking SSRI/SNRI/TCA medications were noted to have a higher pseudarthrosis rate, possibly due to the inhibitory effects of these medications on osteoblast function. However, this biological effect is highly unlikely related to an increased ASD incidence. Contrarily, if a new disease at adjacent levels is promoted by “fusion,” then the SSRI/SNRI/TCA group, which has a higher nonunion rate, would be expected to have a lower ASD incidence. Our multivariate linear regression analysis suggests that ASD was not caused by mechanical factors, but rather the result of the way these patients, medicated for depression, may have presented to their surgeons with residual symptoms following their index procedure in short-term follow-up.
Unsurprisingly, our study found that longer construct length was a risk factor for pseudarthrosis, which is consistent with previous literature [30]. A previous retrospective study that compared 1-level versus 2-level ACDFs suggested that the radiographic union of an ACDF construct is half as likely for 2-level ACDFs at 2-year follow-up [30]. Similarly, we report an OR of 0.53 (CI, 0.42–0.68) for the radiographic union of multilevel constructs compared to 1-level ACDFs at approximately 22 months of follow-up.
Our study limitations include the inherent nature of retrospective studies and the reliance on accurate information when performing a chart review. We were able to review the patient’s chart for prescriptions; however, the consumption of patients of the prescribed medication and the medication prescription duration were not determined. Our data was limited to the collection of SSRI/SNRI/TCA use (yes/no), and we believe the benefit of understanding dose-response relationships between serotonin reuptake-inhibiting medications and pseudarthrosis rates. Well-designed prospective trials and animal models may be beneficial in establishing this relationship. Further, we did not evaluate an exhaustive list of antidepressant medications, and certain serotonin reuptake-inhibiting drugs may be more potent at inhibiting spinal fusion or have a greater impact on ASD; thus, higher-powered studies would be required to evaluate the interaction of each antidepressant on spinal fusion. Surgical technique was different between each surgeon, including some surgeons’ preference to incorporate allograft, titanium, or PEEK as the interbody device. Further, 1–4-level fusions were included in our analysis. However, we attempted to account for this heterogeneity through multivariate analysis. The short length of clinical follow-up limited our ability to identify all patients who will develop symptomatic ASD. Each year provides a 2.2% increase in ASD, thus a longer follow-up would provide additional insight into the role of serotonin reuptake-inhibiting agents in ASD [8]. However, the number of patients with 1-year dynamic radiographs limited our cohort size, and to our knowledge, this is the largest number of patients with dynamic cervical spine radiographs stratified into groups based on serotonin reuptake-inhibiting medication prescriptions.
Conclusions
Serotonin reuptake-inhibiting drugs lead to an elevated risk of pseudarthrosis and revision surgery due to ASD in patients undergoing ACDF. Additionally, patients taking these medications have worse preoperative and postoperative PROMs, but this is likely due to their underlying depression, as demonstrated in the similar recovery ratios and degree of improvement after surgery compared to patients without serotonin reuptake-inhibiting antidepressant prescriptions.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: MJL, GRT, JKL; data curation: NDA, GRT, JDP, DMF; formal analysis: NDA, GRT; funding acquisition: none; methodology: MJL; project administration: IDK, BIW, JAR, MFK, JKL, ASH, CKK, ARV, GDS; visualization: MJL; writing–original draft: MJL, NDA; writing–reivew & editing: GRT, BAK, BIW, JAR, MFK, ASH, CKK, ARV, GDS; and final approval of the manuscript: all authors.