Thoracolumbar Injury Classification and Severity Score Is Predictive of Perioperative Adverse Events in Operatively Treated Thoracic and Lumbar Fractures
Article information
Abstract
Study Design
A retrospective cohort study of patients with surgically treated thoracolumbar fractures.
Purpose
This study aimed to describe the incidence of adverse events (AEs) after surgical stabilization of thoracolumbar spine injuries and to identify predictive factors for the occurrence of AEs.
Overview of Literature
Thoracolumbar spine fractures are frequently present in patients with blunt trauma and are associated with significant morbidity. AEs can occur due to the initial spinal injury or secondary to surgical treatment. There is a lack of emphasis in the literature on the AEs that can occur after operative management of thoracolumbar fractures.
Methods
We performed a retrospective review of 199 patients with surgically treated thoracolumbar fractures operated between January 2007 and January 2018. The potential risk factors for the development of AEs as well as the development of common complications were evaluated by univariate analysis, and a multivariate logistic regression analysis was performed to identify independent risk factors predictive of the above.
Results
The overall rate of AEs was 46.7%; 83 patients (41.7%) had nonsurgical AEs, whereas 24 (12.1%) had surgical adverse events. The most common AEs were urinary tract infections in 43 patients (21.6%), and hospital-acquired pneumonia in 21 patients (10.6%). On multivariate logistic regression, a Thoracolumbar Injury Classification and Severity (TLICS) score of 8–10 (odds ratio [OR], 6.39; 95% confidence interval [CI], 2.33–17.51), the presence of polytrauma (OR, 2.64; 95% CI, 1.17–5.99), and undergoing open surgery (OR, 2.31; 95% CI, 1.09–4.88) were significant risk factors for AEs. The absence of neurological deficit was associated with a lower rate of AEs (OR, 0.47; 95% CI, 0.31–0.70).
Conclusions
This study suggests the presence of polytrauma, preoperative American Spinal Injury Association score, and TLICS score are predictive of AEs in patients with surgically treated thoracolumbar fractures. The results might also suggest a role for minimally invasive surgical methods in reducing AEs in these patients.
Introduction
Thoracolumbar spine fractures are present in up to 6.9% of all patients with blunt trauma [1-3]. They encompass a wide variety of injury patterns, from low-energy vertebral compression fractures to high-energy fracture dislocations. They are the cause of significant morbidity, including paralysis, pain, deformity, and loss of function [2]. Post-traumatic complications can occur as a direct result of, or secondary to, their initial injuries, or secondary to their operative treatment [1-3]. There is a lack of emphasis in the literature on the adverse events that can occur after operative management of thoracolumbar fractures, with the most emphasis on the results of operative versus nonoperative management, timing of surgery, and the radiological and quality of life outcomes after operative management. This study aimed to describe the incidence of adverse events after surgical stabilization of thoracolumbar spine injuries and to identify factors predictive of adverse events, both nonoperative and operative.
Materials and Methods
We performed a retrospective review of 199 patients with surgically treated thoracolumbar fractures who were treated between January 2007 and January 2018 at our level 1 trauma center. Exclusion criteria included conservatively treated fractures, pediatric patients younger than 16 years of age, pathological fractures of an infectious or neoplastic origin, and patients with a prior history of spinal surgery. The approving authority was the National Healthcare Group Domain Specific Review Board (DSRB reference no., 2021/00687). The requirement for informed consent was omitted because of the retrospective design of the study.
We collected demographic data in addition to details of the initial trauma and initial injuries sustained. Based on the presence of underlying comorbidities, the Charlson comorbidity index (CCI) was calculated [4]. We collected injury details, such as the mechanism of injury, the Glasgow Coma Score (GCS), the presence of other nonspinal injuries, and the total Injury Severity Scale (ISS). Patients with an ISS of 16 or more and the presence of 2 or more regions of injury were designated as having polytrauma. Neurological impairment at the time of admission and at the time of discharge were graded based on the American Spinal Injury Association (ASIA) score and were recorded in the case notes by the registrar on duty (senior orthopedic trainee with 3 years’ experience) and the spine consultant on duty during that admission [5]. In patients with low GCS or who were unable to cooperate with examination, the first ASIA score when they were conscious and able to cooperate was recorded. The ASIA score was recorded for all patients regardless of injury level.
With respect to the thoracolumbar fracture, the location number and presence of noncontiguous fractures was recorded. Each fracture was classified according to the Association of Osteosynthesis (AO) classification [6], and fracture stability was classified according to the Thoracolumbar Injury Classification and Severity (TLICS) score [7,8]. The TLICS score was calculated by two authors, both of whom are consultant spinal surgeons.
The method of surgical treatment (minimally invasive surgery [MIS] versus open surgery), the surgical approach (posterior, anterior, or combined), the need for decompression, and the number of instrumented levels were also recorded. The choice between conservative and surgical management and the type of surgery performed was dependent on the treating surgeon. In total, there were six spinal surgeons, each with at least 4 years’ experience as independent spinal surgeons. We also recorded intraoperative blood loss, surgical time, need for blood transfusion, and total duration of stay. The main outcome studied was the presence of adverse events within 3 months after surgical stabilization of thoracolumbar fractures. Each patient was followed up for a minimum of 3 months or until death. These adverse events were divided into nonoperative and operative adverse events. An adverse event was defined as one that adversely affected the recovery of the patient and/or required medical treatment or a surgical procedure. A urinary tract infection (UTI) was defined as an infection of the urinary tract with the presence of one or more of the following findings: the presence of fever >38°C; symptoms such as suprapubic tenderness, dysuria, or urinary frequency; cloudy urine; or a positive urine culture. Pneumonia is defined as the presence of a new lung infiltrate on chest imaging, infective symptoms such as fever more than 48 hours after admission, purulent sputum, leukocytosis, and worsening oxygenation. This diagnosis was made by an infectious disease specialist. In National University Hospital, Singapore, patients with hospital-acquired infections are referred to an infectious disease specialist to determine the duration and choice of antibiotic therapy. The diagnosis of a pulmonary contusion is made based on initial computed tomography of the thorax, abdomen, and pelvis, which is the standard investigation performed for all trauma patients at our institution. This diagnosis is made by a radiologist. All adverse events were collected on a weekly basis and were presented at a weekly audit round.
All the statistical analyses were performed using IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). The potential risk factors for the development of adverse events as well as the development of common complications were evaluated by univariate analysis using the Mann-Whitney U test for numerical variables or the chi-square test for categorical variables. Multivariate logistic regression analysis was then performed to identify independent risk factors predictive of the above. Selection was next used to perform model building, removing nonsignificant variables until all the remaining factors were significant predictors of adverse events. The same process was used to determine the independent risk factors of specific adverse events. A p-value of <0.05 was considered significant.
Results
Of the total 199 patients, 158 (79.4%) were male and 41 (20.6%) were female. The mean age was 38 years (range, 20–79 years) and the mean CCI was 1 (range, 0–6). The patients’ most common injury mechanisms were 107 (53.8%) falls from a height, followed by 49 (24.6%) road traffic accidents, and 30 (15.1%) direct traumas. Thirteen patients (6.5%) were injured as a result of suicide attempts; 87 patients (43.7%) had polytrauma; and 12 patients (6.0%) presented with a head injury with GCS of <12. Ten patients (5.3%) presented with spinal shock, and 10 (5.3%) presented with neurogenic shock (Table 1).
The most common location of injury was at the thoracolumbar junction (T11–L2), in 154 patients (77.4%), followed by fractures at L3–L5 in 24 patients (12.1%) and fractures from T1–T10 in 21 patients (10.6%). A total of 59 patients (29.6%) presented with multiple spinal fractures, and 12 (6.0%) presented with noncontiguous spinal fractures. The most common fracture type was AO A3 and A4 burst-type fractures in 124 patients (62.3%), followed by AO B fractures in 52 patients (26.1%) and AO type C fracture dislocations in 23 patients (11.6%). Some 27.1% of patients had a TLICS score of 4 or less, 114 patients (57.3%) had a TLICS score of 5–7, and 31 patients (15.6%) had a TLICS score of 8–10. Seven patients (3.5%) had a score of 3 or less, and 50 (25.1%) had a score of 4. The majority patients (126 [63.3%]) of presented with evidence of neurological injury and had an ASIA score of A–D (Table 1).
In our study, 134 patients (67.3%) have an open procedure and 65 (32.7%) underwent an MIS procedure. The mean intraoperative blood loss was 577 mL (range, 50–4,500 mL), and the mean operative time was 225 minutes (range, 50–750 minutes). The mean duration of surgery for patients undergoing open surgery was 3.9 hours (range, 1.3–12.0 hours), and 3.5 hours (range, 1.2–12.5 hours) for patients undergoing MIS surgery. The mean blood loss in the open surgery group was 843 mL (range, 40–4,500 mL) and 141 mL (range, 20–1,000 mL) in the MIS surgery group. A total of 189 patients (90.5%) were treated with a posterior-only approach, 13 (6.5%) had a combined anterior and posterior approach, and 6 (3.0%) had an anterior-only approach (Table 2).
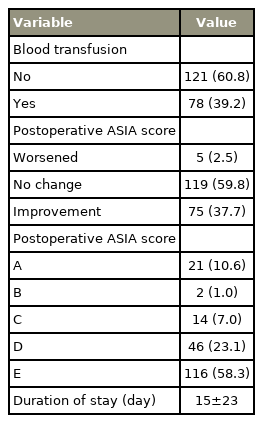
The mean duration of stay was 21 days (range, 5–165 days), and 78 patients (39.2%) required a blood transfusion either intraoperatively or postoperatively. In this study, 75 patients (37.7%) had an improvement in their postoperative ASIA score, and 119 patients (59.8%) maintained their preoperative ASIA score. There were five patients (2.5%) with postoperative worsening of the ASIA score (Table 3).
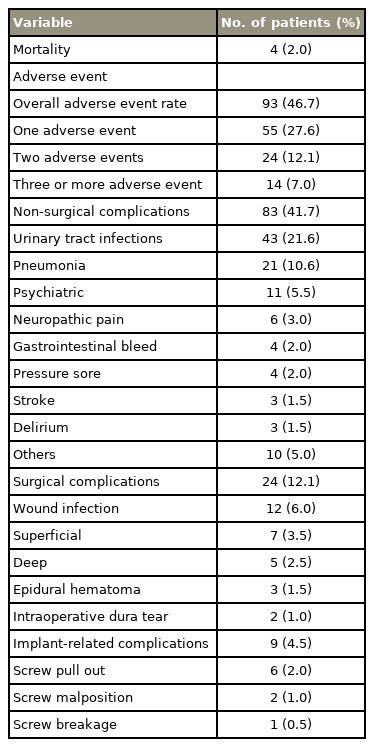
The overall rate of adverse events was 46.7%; 83 patients (41.7%) had nonsurgical adverse events, whereas 24 patients (12.1%) had surgical adverse events. A total of 55 patients (27.6%) had a single event, 24 patients (12.1%) had two events, and 14 patients (7.0%) had three or more adverse events. The most common nonoperative adverse events were nosocomial infections: 43 patients (21.6%) had hospital-acquired UTIs and 21 patients (10.6%) had hospital-acquired pneumonias. The most common surgical adverse events encountered were surgical site infections in 12 patients (6.0%), 7 (3.5%) of which were superficial and successfully treated with antibiotics, whereas 5 (2.5%) had deep infections requiring surgical debridement. Implant-related complications were the next most common, nine patients (4.5%) requiring a revision procedure for pedicle screw pull-out, malposition, or breakage. Other less common adverse events included intraoperative dural tears in two patients (1.0%) and postoperative epidural hematomas in three patients (1.5%), all of which required operative management (Table 4). Psychiatric adverse events included development of acute stress reaction, depression, and post-traumatic stress disorder; delirium refers to an altered mental state due to an underlying medical condition. Intraoperative complications included intraoperative dura tear (2 [1.0%]) and screw malposition (2 [1.0%]). The majority of complications occurred within the first month of treatment, with screw pull-out (4 [2.0%]) and screw breakage (1 [0.5%]) the only complications that occurred after the first month.
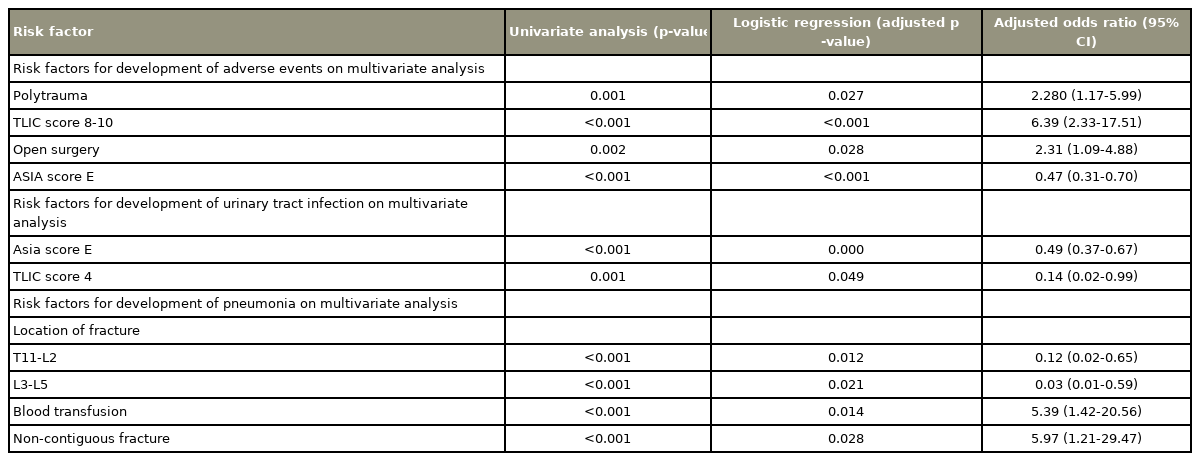
On multivariate logistic regression, a TLICS score of 8–10 (odds ratio [OR], 6.39; 95% confidence interval [CI], 2.33–17.51), the presence of polytrauma (OR, 2.64; 95% CI, 1.17–5.99), and undergoing open surgery compared with MIS (OR, 2.31; 95% CI, 1.09–4.88) were significant risk factors for adverse events occurring. The absence of neurological deficit as evidenced by an ASIA score on admission of E was associated with a lower rate of adverse events (OR, 0.47; 95% CI, 0.31–0.70) (Table 5).
We then performed multivariate logistic regression to identify the independent risk factors for UTIs and pneumonia, which were the two most common adverse events. On logistic regression, the absence of a neurological deficit as evidenced by an ASIA score on admission of E was associated with a significantly lower rate of complications (OR, 0.47; 95% CI, 1.09–4.88), as was a TLICS score of 4 (OR, 0.14; 95% CI, 0.02–0.99). The presence of a spinal fracture in the T10–L2 (OR, 0.12; 95% CI, 0.02–0.65) or L3–L5 region (OR, 0.03; 95% CI, 0.01–0.59) was associated with a lower rate of pneumonia development compared with fractures in the T1–T9 region. The presence of a noncontiguous fracture (OR, 5.97; 95% CI, 1.21–29.47) or blood transfusion (OR, 5.39; 95% CI, 1.42–20.56) were associated with higher rates of postoperative pneumonia (Table 5).
Discussion
Thoracolumbar fractures typically occur secondary to high-energy mechanisms. The presence of multiple injuries and premorbid comorbidities as well as the extensive surgery needed for treatment of these injuries can lead to a high incidence of adverse events. These adverse events include nosocomial infections, progression of neurological deficits, respiratory failure, deep vein thrombosis, pulmonary embolus, myocardial infarction, and cerebral vascular accidents [1-3].
The morbidity associated with major spinal surgery is unclear and might be under-reported. In a systematic review by Dekutoski et al. [9], the complication rate for thoracic spine surgery was 7%–18%, and the complication rate for lumbar spine surgery was 4%–14%. However, Street et al. [10] reported a morbidity rate of 73.5% in a study of 942 consecutive patients undergoing complex spinal surgery. This difference was attributed to increased accuracy in reporting adverse events due to dedicated weekly multidisciplinary rounds and a formal tool for recording adverse events in patients undergoing complex spinal surgery.
In a systematic review by Ghobrial et al. [11], the incidence of all adverse events in patients who underwent surgery for thoracic or lumbar fractures was 32.6%, with a significantly higher incidence of infections (pneumonia, UTI, wound infection, and sepsis) in operative patients compared with nonoperative patients. Dimar et al. [3] reported a 79% incidence of complications (minor 30%, major 49%) in patients undergoing stabilization for fractures of the thoracic and lumbar spine. This study was a multicenter review of 230 patients. In their study, UTI (11%), followed by wound infection (5.5%) and pulmonary complications (5%), were the most commonly encountered complications. In a study of Dimar et al. [3], the severity of neurologic injury, the number of comorbidities, and the use of high-dose steroids significantly increased the risk of a major complication after surgical stabilization of thoracolumbar spine fractures. Glennie et al. [12] reported an adverse event rate of 56% in 276 operatively treated patients. The most common adverse events were UTIs (19.7%), neuropathic pain (12.3%), pneumonias (11.8%), delirium (10.5%), and ileus (6.2%); the presence of neurological injuries was also a significant risk factor for the occurrence of adverse events. Operatively treated patients had a significantly higher rate of complications compared with nonoperatively treated patients (56% versus 13%).
We had an overall adverse event rate of 46.5%, which was lower than that of Dimar et al. [3] and Glennie et al. [12] and higher than that reported by Ghobrial et al. [11]. We had a similar profile of adverse events, with nosocomial UTIs (21.6%) and pneumonia (10.6%) being the most commonly reported adverse events.
In our study, the absence of neurological injury as evidenced by a preoperative ASIA score of E was associated with a lower rate of adverse events. A poorer preoperative ASIA score had previously been shown by Whitmore et al. [13] to be associated with an increased likelihood of a major complication in patients undergoing major spinal surgery. Our findings were similar to that of Dimar et al. [3], who also reported a significant correlation between neurological injury and development of adverse events postsurgery. They also reported the use of high-dose steroids and the CCI as significant predictors of adverse events [3]. The use of high-dose steroids was not a risk factor for adverse events, given that we do not practice the use of high-dose steroids in our institution. The demographics of our patient population, largely young males of working age with no comorbidities, could be the reason why the CCI was not a significant risk factor for postoperative adverse events. Very few of our patients had any comorbidities, the most common being diabetes mellitus (10 [5.0%]) and ischemic heart disease (8 [4.0%]), and these were not found to be significant risk factors.
In our study, a higher TLICS score was associated with a higher rate of adverse events. The TLICS classification is based on the morphology of the fractured vertebrae, the neurological status of the patient, and the integrity of the important posterior ligamentous complex [6-8]. At present, there is no clear indication in the literature of increased rates of adverse events in patients with higher TLICS scores; however, we believe that due to the higher rates of spinal cord injury and higher-energy mechanisms of injury, there might be more unstable fracture morphologies and neurological injury in the patients with higher TLICS scores. In a systematic review by Khorasanizadeh et al. [14], recovery from spinal cord injury had a significant association with initial injury mechanism and severity. The presence of a high TLICS score could be a surrogate marker of a severe initial injury with a high-energy mechanism. Polytrauma patients were found to have significantly higher rates of adverse events; a high ISS is a known predictor of complications after thoracolumbar spine fractures [15], which could be due to the increased severity of the initial mechanism of injury.
Minimally invasive spine surgery in spinal trauma, in the form of percutaneous pedicle screws, has become increasingly popular [16]; in thoracolumbar fractures it is associated with lower infection rates, less intraoperative blood loss, and shorter operative time and hospital stay [17-19]. The reduced blood loss and soft tissue trauma in minimally invasive spine surgery could explain the lower adverse event rate in our patients. In our study, MIS patients had an adverse event rate of 30.7% versus 54.1% in the open surgery patients, which is consistent with the increased role and indication for minimally invasive methods in spinal trauma surgery.
In the two largest studies of postoperative adverse events after surgical treatment of thoracolumbar fractures, UTIs have consistently been the most common postoperative adverse events [3,12]. Similar to Glennie et al. [12], we found the ASIA score to be predictive for development of a UTI. Age was not a significant predictive factor due to the demographics of our patient population. A TLICS score of 4 or less was predictive of a lower rate of UTIs. We postulate that a lower TLICS score could be indicative of a less severe mechanism of injury and an intact neurological status, thus reducing the risk of UTI due to a neurogenic bladder and prolonged catheterization.
Pneumonia is also a common adverse event in postoperative patients with thoracolumbar fractures. We found that the presence of a noncontiguous fracture and a higher thoracic fracture was associated with significantly higher rates of pneumonia. The presence of a higher thoracic fracture and/or a noncontiguous fracture could lead to paralysis of the intercostal muscles and thoracic cage, leading to decreased forced vital capacity and an increased risk of hospital-acquired pneumonia [20,21]. Increased blood transfusion is associated with an increased risk of infection [22], which could explain the significant association with pneumonia in our patients.
This study has several limitations. First, it is retrospective in nature, thus there could have been variations in practice at the start and the end of the series and between the surgeons treating the patients. Although major adverse events might have been recorded, minor adverse events might not have been recorded, despite data being collected on a weekly basis and presented at a weekly audit round. The future use of valid and sensitive methods for recording adverse events in patients, such as the Spine Adverse Events Severity System [23], might improve our ability to more accurately record adverse events. The variables predictive of an adverse event, the TLICS score and ASIA score, might be co-linear, although we have analyzed both factors separately in our logistic regression models. In both cases, the ASIA score and TLICS score were found to be significant predictors of adverse events and UTIs. The other components within the TLICS score, morphology of fracture and presence of PLC injury, indirectly demonstrate the severity of the initial injury, which could be predictive of adverse events. The TLICS score is a commonly used score in thoracolumbar spinal trauma, and a possible association between the TLICS score and adverse events might be a useful way for spinal surgeons to counsel patients in their care. The generalizability of our results, which occurred in a level 1 trauma center, might also be limited.
Conclusions
In our cohort of patients, there was an overall adverse event rate of 46.7%, with UTIs (21.6%) being the most common complication. This study suggests that severity of neurological injury and initial injury as measured by the presence of polytrauma, preoperative ASIA score, and TLICS score are predictive of adverse events in patients with operatively treated thoracolumbar fractures. It might also demonstrate the role of MIS methods in reducing adverse events in these patients. We described independent risk factors for the development of UTIs and pneumonia, which were the most common adverse events in our cohort of patients. There is a need for further, larger, prospective studies in multiple centers to identify, predict, and minimize complications in this group of vulnerable patients.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Literature review: Gabriel Liu, Jiong Hao Tan, Jun Cheong Kong, Yong Hao Joel Tan, Nishant Kumar; data collection: Jiong Hao Tan, Jun Cheong Kong, Yong Hao Joel Tan, Nishant Kumar; data analysis: Gabriel Liu, Jiong Hao Tan, Jun Cheong Kong, Yong Hao Joel Tan, Nishant Kumar, Shen Liang, Seah Jing Sheng Shawn, Chiu Shi Ting, Lau Leok Lim, Hey Hwee Weng Dennis, Naresh Kumar, Joseph Thambiah, Hee-Kit Wong; and preparation of manuscript and review of manuscript: Gabriel Liu, Jiong Hao Tan, Jun Cheong Kong, Shen Liang, Seah Jing Sheng Shawn, Chiu Shi Ting, Lau Leok Lim, Hey Hwee Weng Dennis, Naresh Kumar, Joseph Thambiah, Hee-Kit Wong.