Comparative Analysis of 30-Day Readmission, Reoperation, and Morbidity between Posterior Cervical Decompression and Fusion Performed in Inpatient and Outpatient Settings
Article information
Abstract
Study Design
A retrospective cohort study.
Purpose
To compare 30-day readmission, reoperation, and morbidity for patients undergoing posterior cervical decompression and fusion (PCDF) in inpatient vs. outpatient settings.
Overview of Literature
PCDF has recently been increasingly performed in outpatient settings, often utilizing minimally invasive techniques. However, literature evaluating short-term outcomes for PCDF is scarce. Moreover, no currently large-scale database studies have compared short-term outcomes between PCDF performed in the inpatient and outpatient settings.
Methods
Patients who underwent PCDF from 2005 to 2018 were identified using the National Surgical Quality Improvement Program database. Regression analysis was utilized to compare primary outcomes between surgical settings and evaluate for predictors thereof.
Results
We identified 8,912 patients. Unadjusted analysis revealed that outpatients had lower readmission (4.7% vs. 8.8%, p=0.020), reoperation (1.7% vs. 3.8%, p=0.038), and morbidity (4.5% vs. 11.2%, p<0.001) rates. After adjusting for baseline differences, readmission, reoperation, and morbidity no longer statistically differed between surgical settings. Outpatients had lower operative time (126 minutes vs. 179 minutes) and levels fused (1.8 vs. 2.2) (p<0.001). Multivariate analysis revealed that age (p=0.008; odds ratio [OR], 1.012), weight loss (p=0.045; OR, 2.444), and increased creatinine (p<0.001; OR, 2.233) independently predicted readmission. The American Society of Anesthesiologists (ASA) classification of ≥3 predicted reoperation (p=0.028; OR, 1.406). Rehabilitation discharge (p<0.001; OR, 1.412), ASA-class of ≥3 (p=0.008; OR, 1.296), decreased hematocrit (p<0.001; OR, 1.700), and operative time (p<0.001; OR, 1.005) predicted morbidity.
Conclusions
The 30-day outcomes were statistically similar between surgical settings, indicating that PCDF can be safely performed as an outpatient procedure. Surrogates for poor health predicted negative outcomes. These results are particularly important as we continue to shift spinal surgery to outpatient centers. This importance has been highlighted by the need to unburden inpatient sites, particularly during public health emergencies, such as the coronavirus disease 2019 pandemic.
Introduction
Posterior cervical decompression and fusion (PCDF) is an effective surgical technique used to treat various cervical spine abnormalities. The addition of posterior cervical fusion to laminectomy has become increasingly utilized in treating myelopathy and radiculopathy [1].
Spinal surgery, in general, has been increasingly performed in the outpatient setting. PCDF has followed this pattern, with recently increased procedures performed in the outpatient settings, often utilizing minimally invasive techniques [2]. Outpatient spinal surgery has been associated with benefits of greater efficiency and lower overall costs [3]. Improvements in these aspects are necessary for the demands of an aging population and a reforming health care payment and delivery landscape. However, short-term outcomes-research evaluating the safety of this trend is limited, particularly regarding PCDF.
Outcomes for PCDF have shown clinically significant improvement along with high fusion rates and low revision rates and adverse events [4,5]. However, data that directly evaluate short-term outcomes for PCDF are scarce. Moreover, no currently large-scale database studies have compared short-term outcomes between PCDF performed in the inpatient and outpatient settings. Therefore, this study aimed to compare inpatient and outpatient PCDF based on 30-day readmission, reoperation, and morbidity. The study findings provide insight into the safety of performing PCDF in the outpatient setting.
Materials and Methods
1. Study design and population
This retrospective analysis included patient data from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database from 2005 to 2018. This project is exempt from the Institutional Review Board as this database is de-identified, without direct patient involvement.
Patients aged ≥18 years, who underwent elective single-level PCDF, were identified and included based on the Current Procedural Terminology (CPT) code 22600, in conjunction with a cervical decompression code (63045, 63001, 63015, or 22210). We evaluated multilevel fusion using CPT 22614. Patients were excluded if they had CPT codes for anterior, thoracic, and/or lumbar procedures; deformity, revision, nonelective, or spinal tumor surgery; if they were admitted from non-home settings; discharged anywhere other than home or rehabilitation; or had emergency surgery, preoperative systemic inflammatory response syndrome or sepsis, disseminated cancer, or decompression without posterior cervical fusion.
2. Outcomes and variables
The NSQIP database provides data on patients treated as inpatient or outpatient as defined by the NSQIP Participant Use Data File [6]. Patients were categorized into either inpatients or outpatients based on the provided variable.
Primary outcomes were 30-day readmission, reoperation, and morbidity. Readmission includes any inpatient stay at the same or another hospital related to the surgical procedure [6]. The NSQIP database did not collect readmission data until 2011. Reoperation and morbidity outcomes were collected from the start of the dataset in 2005. Reoperation includes all major surgical procedures requiring unplanned operating room returns [6]. Morbidity includes infectious, pulmonary, cardiac, renal, neurological, hematologic, and thromboembolic complications reported in the dataset [6,7]. Primary outcomes, as well as specific complications, were compared between inpatient and outpatient PCDF.
Predictors of primary outcomes were analyzed amongst the entire cohort. Variables evaluated as potential predictors included patient demographic, comorbidity, preoperative lab values, and procedural factors (Table 1). Variables with <80% of available data were excluded from the multivariate analysis to avoid distorted results [7].
3. Statistical analysis
Analyses were completed using the IBM SPSS ver. 28.0 (IBM Corp., Armonk, NY, USA). Demographic, comorbidity, laboratory, and procedural factors were individually analyzed for baseline differences between inpatients and outpatients using the Student t-test for continuous and chi-square or Fisher’s exact test for categorical variables. Additionally, the above factors were individually analyzed for association with the primary outcomes using univariate logistic regression. Potential predictor variables from the univariate analyses that were significant (p<0.05) [8], as well as surgical setting, were then evaluated for significance (p<0.05) as independent predictors and control variables in a series of multivariate logistic regression analyses of the primary outcomes.
Results
We identified 8,912 patients (8,559 inpatient) who underwent PCDF. Baseline group differences and unadjusted primary outcomes are provided in Table 1. The inpatient group was significantly older (62 versus 55 years, p<0.001); more likely to be functionally dependent (4.5% versus 1.1%, p=0.002) and discharged to rehabilitation (25.2% versus 7.4%, p<0.001); more likely to have hypertension (58.9% versus 47.6%, p<0.001), an ASA-class of ≥3 (63.8% versus 47.9%), and decreased hematocrit (18.5% versus 9.9%, p<0.001); and less likely to be obese (45.7% versus 52.1%, p=0.018) and smoke (24.7% versus 32.9%, p=0.001). Inpatients also had greater operative time (179 minutes versus 126 minutes) and levels fused (2.2 levels versus 1.8 levels) (p<0.001).
1. Primary outcomes
Unadjusted analysis revealed that outpatients had significantly lower rates of readmission (4.7% versus 8.8%, p=0.020), reoperation (1.7% versus 3.8%, p=0.038), and morbidity (4.5% versus 11.2%, p<0.001) compared to inpatients (Table 1). Inpatient PCDF was associated with urinary tract infection (UTI) (1.6% versus 0%, p=0.018) and transfusion (4.4% versus 0.3%, p<0.001) (Table 2).
After adjusting for significant baseline differences and primary outcome predictors, the multivariate analysis revealed that readmission (p=0.236; odds ratio [OR], 1.436), reoperation (p=0.524; OR, 1.317), and morbidity (p=0.716; OR, 1.108) no longer statistically differed between surgical setting (Tables 3–5). Additionally, UTI and stroke no longer statistically differed between surgical settings (Table 2).
2. Predictor analysis
Readmissions occurred in 620 patients (8.6%). The multivariate analysis revealed age (p=0.008; OR, 1.012), unexpected weight loss (p=0.045; OR, 2.444), and increased creatinine (p<0.001; OR, 2.233) as independent readmission predictors (Table 3).
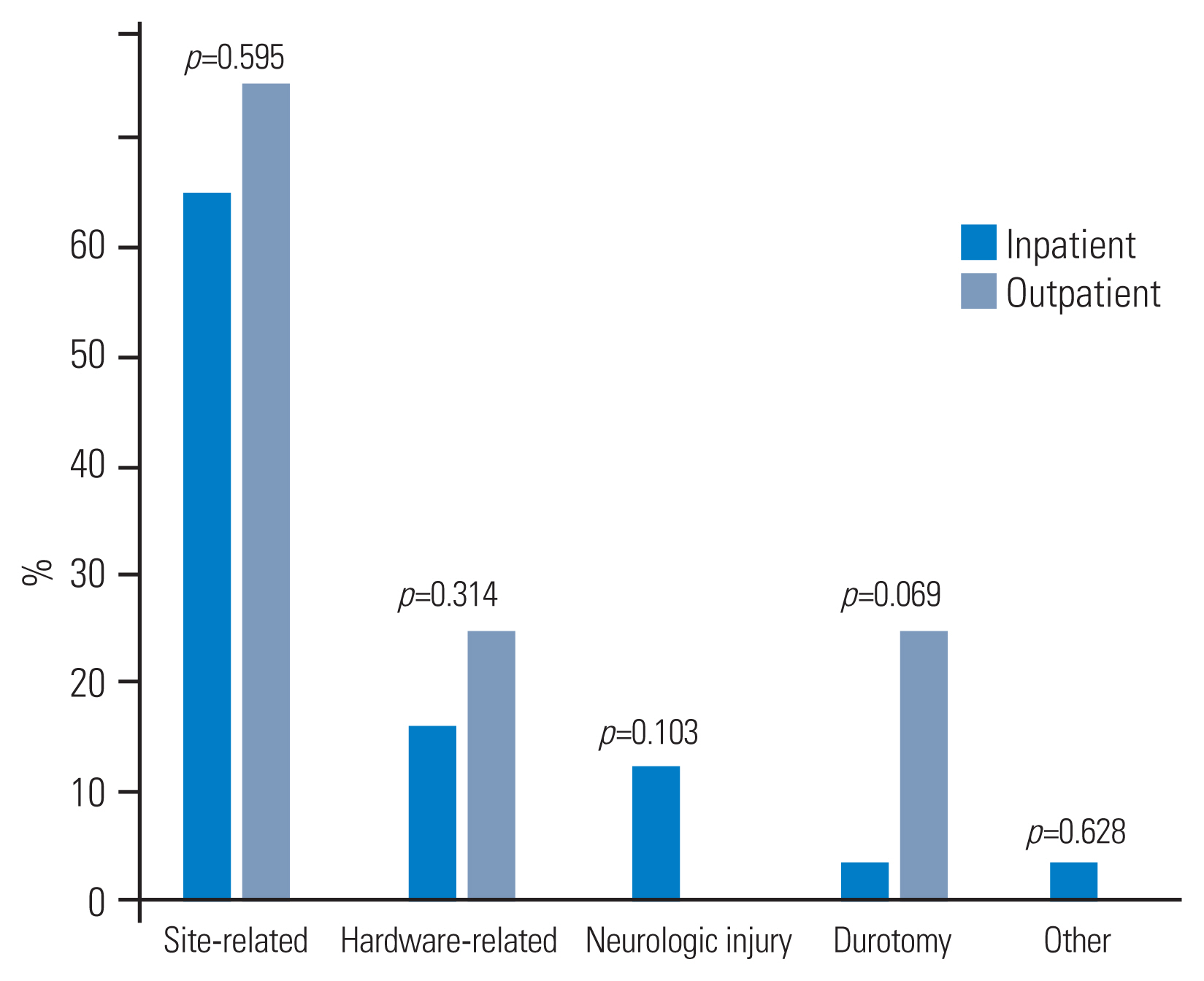
Reoperations occurred in 335 patients (3.8%). ASA-class of ≥3 (p=0.028; OR, 1.406) and prior open wound (p=0.040; OR, 2.557) predicted reoperation on multivariate analysis (Table 4). Reoperations most occurred due to site-related complications (65.2%), followed by hardware-related complications (16.3%). No statistically significant differences were found in the reasons for reoperation between inpatient and outpatient settings (Fig. 1).
Morbidity occurred in 972 patients (10.9%). Discharge to rehabilitation (p<0.001; OR, 1.412), ASA-class of ≥3 (p=0.008; OR, 1.296), decreased hematocrit (p<0.001; OR, 1.700), and operative time (p<0.001; OR, 1.005) predicted morbidity on multivariate analysis (Table 5).
Discussion
1. Comparison of setting: primary outcomes
An increasing trend toward performing spine surgery was found in the outpatient setting, but literature evaluating outpatient PCDF is limited. In the present study, 30-day outcomes were statistically similar between inpatients and outpatients, indicating that PCDF can safely be performed in the outpatient setting.
The outcomes observed in the present study are consistent with current literature on outpatient spinal procedures [9,10]. Segal et al. [8] demonstrated that rates of readmission, reoperation, and complication were statistically similar between inpatient and outpatient cervical disc replacement. Bovonratwet et al. [9] showed that rates of bleeding events requiring transfusion for posterior lumbar fusion were significantly lower in the outpatient setting, without significant differences between inpatient and outpatient readmission or reoperation rates. Khanna et al. [11] demonstrated a significantly lower overall complication rate for anterior cervical discectomy and fusion in the outpatient setting compared with the inpatient setting, without significant differences in readmission and mortality rates. Low complication rates for outpatient discectomy have been well-described [10,12]. Inpatient and outpatient outcomes did not statistically differ despite significant variability in resources available among outpatient facilities, such as equipment availability, laboratory draw access, and specialty physician support. This may indicate that features intrinsic to outpatient surgery foster a safe and efficient operative environment [13]. This is evidenced by reduced operative time, lower cost, and statistically similar complication and readmission rates.
Moreover, the outcomes presented in this study are consistent with current literature that evaluates PCDF. Long-term PCDF studies have demonstrated reoperation rates ranging from 4% to 27% [14,15]. Our early reoperation rate of 3.8% for the entire cohort is in-line with these findings. Complication and readmission profiles of PCDF have been incompletely evaluated thus far. Current literature on PCDF provides varying data on complication rates; however, most studies demonstrate postoperative complication rates ranging from 15% to 25% [5,16,17]. Commonly reported complications or adverse events included axial pain, temporary neurologic deficit, and wound infection [5]. The PCDF literature provides scant data on readmission rates. Snyder et al. reported 30-day readmission rates following PCDF of 10% for non-home discharges and 6% for home discharges [18]. Cole et al. [19] reported a 30-day readmission rate of 9.9% for the posterior approach to multilevel degenerative cervical disease. Despite inadequate extensive data, these findings are consistent with our overall 30-day readmission rate of 8.6%.
2. Predictor variables
Few studies have reported on predictors of poor early outcomes in PCDF. Snyder et al. [18] found that dependent functional status, diabetes, ASA-class of >2, older age, and female gender were significant predictors of non-home discharge, severe post-discharge adverse events, and unplanned readmission following PCDF. Tetreault et al. [20] found that a longer operation duration was predictive of perioperative complications. Similarly, our study found that older age independently predicted readmission, and ASA-class of ≥3 and longer operative time predicted morbidity on multivariate analysis. However, we did not obtain similar findings for dependent functional status, diabetes, and female gender. Several other studies have found operative time to predict complications and morbidity in spinal surgery [21,22]. The suggested benefit of reducing operative time further supports the shifting trend towards outpatient spinal surgery.
Baseline health status is often considered in deciding on inpatient or outpatient surgery for patients. Analysis revealed that this was evident in our present study, as patients in the inpatient cohort were more likely older and have medical comorbidities. Notably, outpatients had significantly greater rates of obesity and smoking, further suggesting that they were overall healthier by being selected for outpatient surgery, despite having these negative health attributes. These discrepancies were addressed by comparing readmission, reoperation, and morbidity before and after baseline difference adjustments. Before adjustment, the outpatient cohort had significantly lower readmission, reoperation, and morbidity rates. After adjustment, no statistically significant difference was found between the surgical settings in any of the measured variables.
3. Procedural factors
Operative time was longer in the inpatient group. Similar findings were observed in the comparison of inpatient to outpatient cervical disc replacement [8]. On average, inpatient spinal surgery requires approximately 30 minutes more operative time than outpatient [23]. Our study showed that outpatient PCDF was 53 minutes faster on average. Some of this difference in operation time may be attributed to the performance of more complex cases in inpatient settings; however, the statistically similar reoperation, readmission, and morbidity rates, even after adjusting for baseline differences between cohorts, support the idea that outpatient surgery provides similar efficacy as evidenced by the increased number of performed levels.
4. Limitations
The NSQIP database provides access to a large number of nationally represented patients from multiple institutions and highly relevant variables, allowing for generalizability and the development of meaningful predictive models [24]. Trained reviewers collect data for the database while adhering to stringent variable definitions, rendering it more reliable than other large-scale administrative databases [25].
Limitations exist with the NSQIP database, which uses hospital billing data to capture inpatient and outpatient status, and thus may not accurately reflect the length of stay [9]. Consequently, some researchers have treated patients with a zero-day length of stay as an outpatient, and greater than zero as an inpatient [9,10]. However, this method can introduce a potential bias by creating modified inpatient and outpatient groups, with fewer and more number of healthier patients, respectively. Additionally, determining that an unexpected negative intraoperative event would have resulted in an intended outpatient case to require inpatient admission is impossible; however, the utilization of billing data to determine inpatient-versus-outpatient status would suggest that the vast majority of any outpatient-converted-to-inpatient patient stay would have been appropriately coded as an inpatient. Therefore, we used the inpatient versus outpatient variable provided by the NSQIP dataset as-is, as has been previously done [8,10]. The detailed indications for outpatient surgery are not provided; however, various patient-related factors that are surrogates for outpatient selection criteria were controlled for in the analysis. Additionally, the database does not account for the evolution of spinal implants, technology, and techniques that have occurred over the period (i.e., facet fusion devices, navigation, robotics, etc.). Furthermore, a disproportionately greater number of cases are performed in inpatient settings compared to those in outpatient settings, which may potentially provide a temporal bias based on recent improvements in surgical technique, technology, and ambulatory surgery centers. Finally, posterior cervical decompression has many different types, such as total laminectomy, hemilaminectomy, laminotomy, or foraminotomy, which are not differentiated in the analysis. However, every included patient in the study underwent fusion, which would more strongly influence the overall morbidity and invasiveness than the utilized decompression method. Therefore, the decompression method is likely less influential given that every patient underwent fusion.
Conclusions
This study compared 30-day outcomes between inpatient and outpatient PCDF. Rates of readmission, reoperation, and morbidity remained statistically similar between inpatient and outpatients after accounting for potential patient confounders through multivariate logistic regression. These findings suggest that PCDF can be safely performed in the outpatient setting.
Notes
Conflict of Interest
David Essig receives consulting fees for Stryker and DePuy. Jeff Silber receives teaching fees for Stryker. For all remaining authors, no potential conflict of interest relevant to this article was reported.
Author Contributions
Study conception: Junho Song, Austin David Katz, David Essig; data analysis: Junho Song, Austin David Katz, Alan Job; manuscript writing: Junho Song, Austin David Katz, Dean Perfetti, Matthew Morris; manuscript revisions: all authors; supervision: Sohrab Virk, Jeff Silber, David Essig; administrative support: Sohrab Virk, Jeff Silber; and final approval of the manuscript: all authors.