Type I Arnold Chiari Malformation with Syringomyelia and Scoliosis: Radiological Correlations between Tonsillar Descent, Syrinx Morphology and Curve Characteristics: A Retrospective Study
Article information
Abstract
Study Design
Retrospective cohort.
Purpose
The current study was planned to evaluate deformity characteristics, assess relationship between morphology of syrinx/ Arnold Chiari malformation (ACM) and deformity, analyze effect of posterior fossa decompression (PFD), and evaluate outcome.
Overview of Literature: Scoliosis in ACM-I and syringomyelia (SM) is uncommon, and deformity characteristics differ from those seen in idiopathic scoliosis.
Methods
Data regarding patients, who underwent PFD for ACM-I presenting with SM and scoliosis between January 2009 and December 2018, were retrospectively collected. Only patients with 2-year follow-up were included. Sagittal/coronal deformity and sagittal spinopelvic parameters were examined. Symmetry and extent of tonsillar descent, as well as morphology (configuration/variation) and extent of syrinx were determined.
Results
A total of 42 patients (20 females; age: 14.2±5.8 years) were included; 35 patients (83.3%) had atypical curves. Mean preoperative coronal Cobb was 57.7°±20.9°; and 12 (28.6%) had significant coronal imbalance. Tonsillar descent was classified as grade 1, 2, and 3 in 16 (38.1%), 11 (26.2%), and 15 (35.7%) patients; 35 patients (83.3%) had asymmetric tonsillar descent; 17 (40.4%), 3 (7.1%), 16 (38.1%), and 6 (14.4%) had circumscribed, moniliform, dilated, and slender syrinx patterns; and 9 (21.4%), 12 (28.6%), and 21 (50%) of syrinx were right-sided, left-sided, and centric. There was no significant relationship between side of tonsillar dominance (p=0.31), grade of descent (p=0.30), and convexity of deformity. There was significant association between side of syrinx and convexity of scoliosis (p=0.01). PFD was performed in all, and deformity correction was performed in 23 patients. In curves ≤40°, PFD alone could stabilize scoliosis progression (p=0.02). There was significant reduction in syrinx/cord ratio following PFD (p<0.001).
Conclusions
ACM-I+SM patients had atypical curve patterns in 83% of cases, and the side of syrinx deviation correlates with scoliosis convexity. Syrinx shrinks significantly following PFD. PFD may not stabilize scoliosis in curves >40°.
Introduction
Chiari identified herniated cerebellar tonsils on postmortem more than a century ago [1]. With the development of high-resolution magnetic resonance imaging (MRI) in the last decade, such tonsillar ectopias (Chiari Malformation, CM) have become more common and acknowledged as an important cause of syringomyelia (SM) [2]. Both these pathologies (CM and SM) have been independently recognized as risk factors for scoliosis [3,4]. While scoliosis has been reported in 25% to 85% of patients with Chiari Malformation type I (CM-I) and SM; the incidence of CM-I and SM in scoliosis patients ranges between 4% and 58% [3–5].
The exact pathogeneses underlying the association between these conditions are still poorly understood [6]. The malfunction of the central nervous system, damage to anterior horn cells, and changes in the dynamics of cerebrospinal fluid flow as a result of tonsillar herniation are all thought to play a role in the formation or propagation of syrinx, and subsequent neurogenic changes in paraspinal musculature possibly lead to the spinal deformity [7,8]. Although deformity patterns associated with SM and CM are different from the deformity characteristics observed in adolescent idiopathic scoliosis patients, the typical curve morphology is not well-documented hitherto [9]. The role of posterior fossa decompression (PFD) on the progression of the syrinx, deformity magnitude, and outcome in patients presenting with a combination of CM-I, SM, and scoliosis are still largely unclear [10,11]. As a result, the current study was designed to evaluate our experience with patients who underwent PFD after presenting with CM-I, SM, and scoliosis. The overall pattern of scoliosis (and its correlation with syrinx morphology and CM-I), its progression, morphological patterns of the syrinx, the effect of PFD on syrinx size and curve magnitude, corrective scoliotic surgeries or other non-surgical interventions undergone; and thus, the overall outcome in such scenarios were all examined.
Materials and Methods
1. Patient and study design
Data on patients who had PFD for Arnold Chiari malformation (ACM)-I presenting with SM and scoliosis at Ganga Medical Center and Hospital between January 2009 and December 2018 were retrospectively gathered with the agreement of Ganga Medical Center and Hospital (IRB application no., 2020/03/14) review board. Only patients who agreed to participate in the trial and had complete clinico-radiological data with a minimum follow-up of 2 years were included. Alternative etiologies for spinal abnormalities were ruled out. Informed consent was obtained from all patients.
From the hospital records, demographic details, clinical history, and examination findings were recorded. Detailed neurological examination findings (motor [including superficial and deep reflexes], sensory and autonomic assessment) of all patients were also recorded. All patients underwent routine radiological evaluation including plain radiographs (whole spine anteroposterior [AP] and lateral), computed tomography (whenever necessary), and whole spine MRI. All radiological images were retrieved from the hospital picture archiving and communication system. The preoperative radiographs were evaluated for the type of deformity, level of apex, curve magnitude (Cobb angle), sagittal spinopelvic parameters, and pelvic obliquity. The left-sided curves, long “C” curves, high thoracic curves, short and acute deformities, and those with apical hyper-kyphosis were classified as atypical deformities [12].
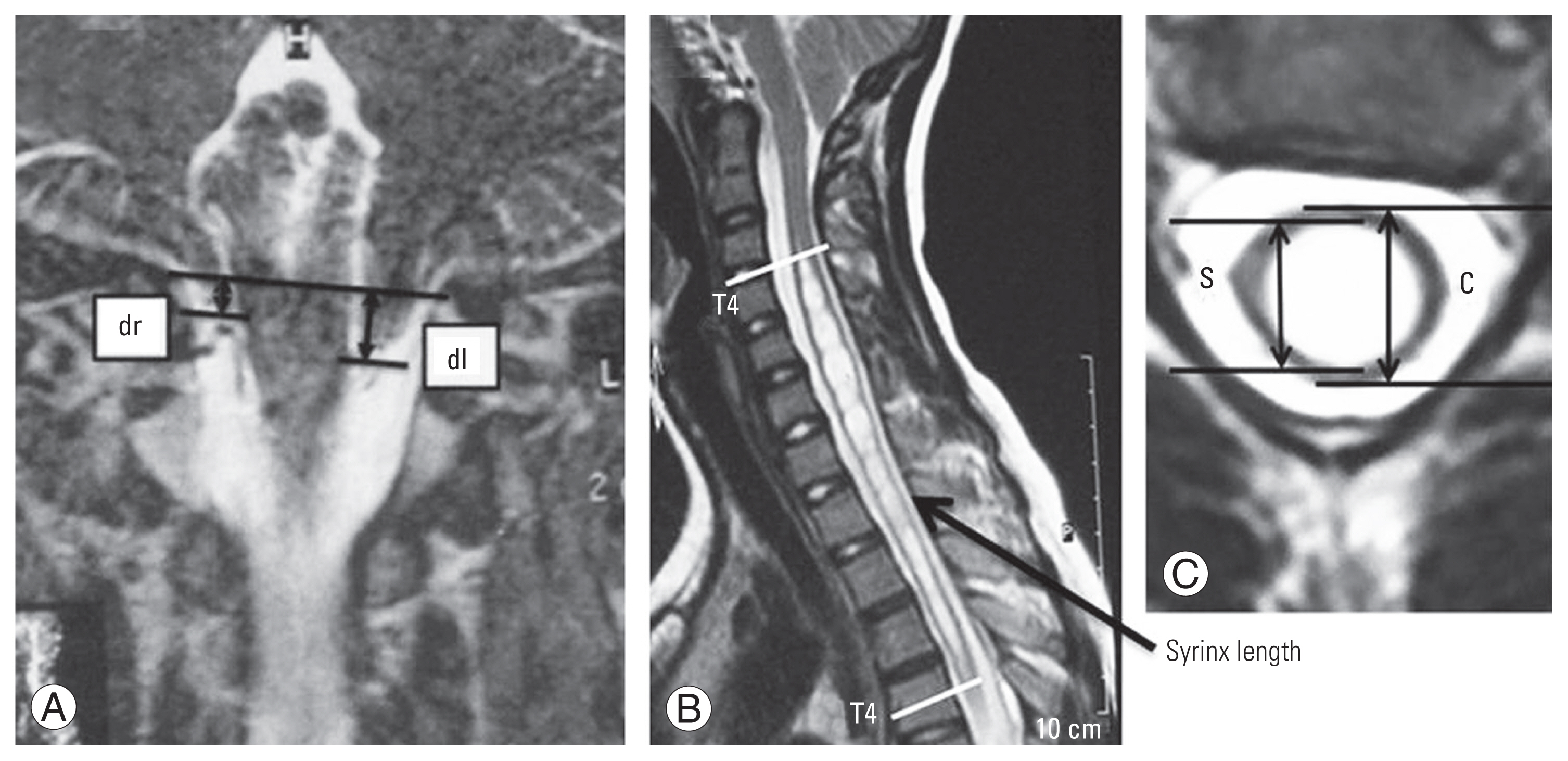
The symmetry, size, and extent of tonsillar descent, as well as the morphology and extent of the syrinx, were assessed on preoperative MRI (axial, sagittal, and coronal sections). The extent of tonsillar descent was divided into three categories: grade I, where the tonsil dropped beyond the foramen magnum but did not reach the C1 arch; grade II, where the tonsil reached the C1 arch; and grade III, where the tonsil dropped beyond the C1 arch [1]. The symmetry of tonsillar ectopia was assessed using coronal images at the base of the brain. The ratio of descent on the right and left sides were quantified, and a ratio ≥1.10 or ≤0.90 was defined as asymmetrical (Fig. 1A) [1].
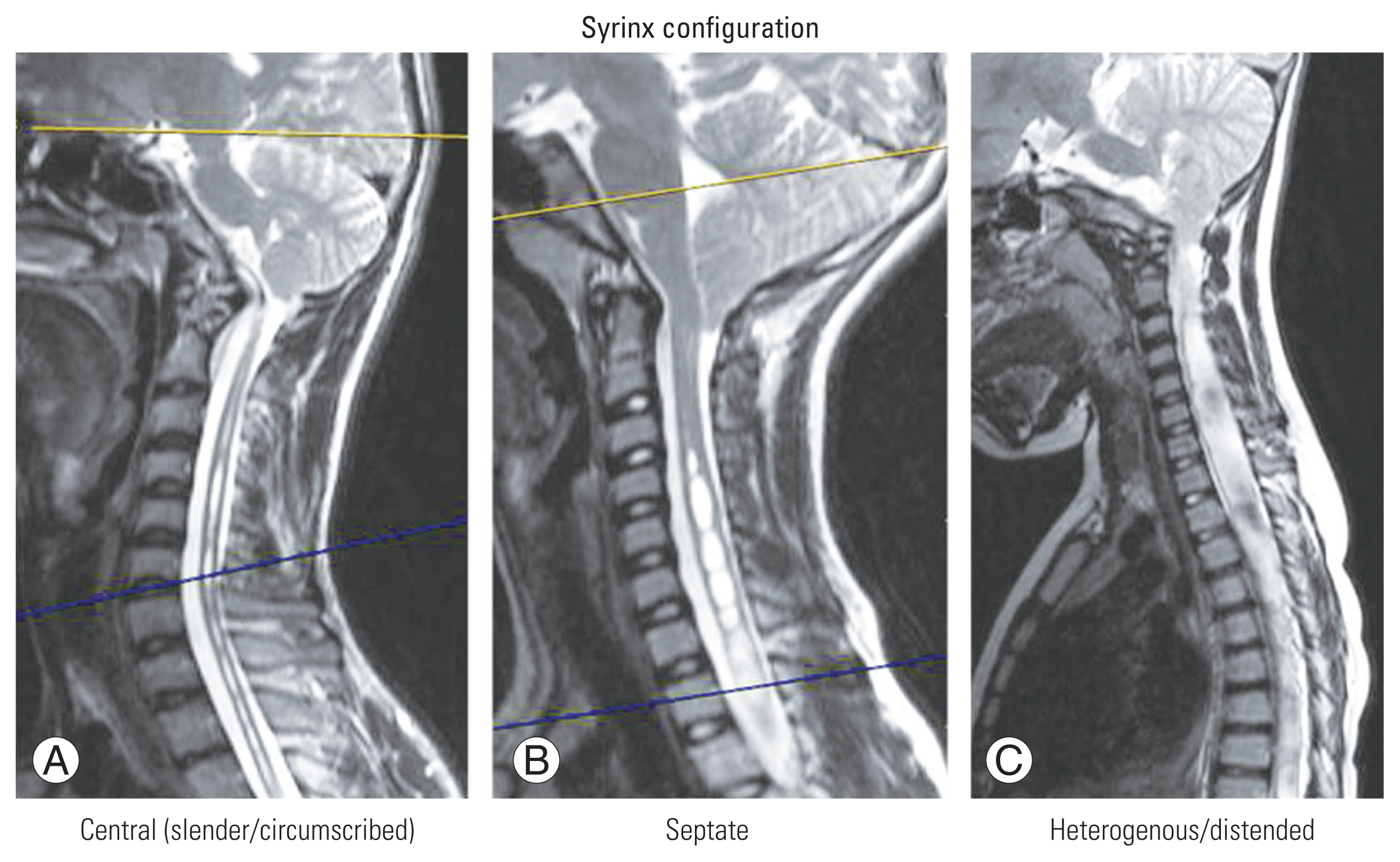
On T2-weighted axial and sagittal MRI, the maximal syrinx/cord (S/C) ratio and length of syrinx were measured respectively (Fig. 1B). On T2-weighted axial MRI, maximal S/C ratio was determined by the ratio between maximal AP diameter of the syrinx and AP diameter of the spinal cord at the same level. On T2-weighted sagittal MRI, the length of syrinx was defined as the length of vertebral segments spanned by syrinx. The configuration of syrinx was categorized into four types, namely distended, moniliform, slender, and circumscribed (Fig. 2) [7]. Based on the assumption that the syrinx is a single straight tube, the side of syrinx deviation was determined by the location of the syrinx relative to the spinal cord at the upper or lower ends of the syrinx on axial images, as described by Yeom et al. [8] (Fig. 3). A syrinx with a deviation ≥1.10 or ≤0.90 was defined as eccentric. All radiological images were initially reported by a specialist radiologist and measurements were obtained by one of the authors (S.S. and N.R.). All radiological details and measurements were further ratified by a senior author (S.R. and A.P.S.).

(A–C) Deviated rate of syrinx location=(right-side distance at the upper end+right-side distance at the lower end)/(left-side distance at the upper end+left-side distance at the lower end).
The current study only included patients who underwent PFD. All patients were followed up on at 6, 12 weeks, and 6 months after their PFD. All patients had whole spine plain radiographs taken at each postoperative visit, and a whole spine MRI was taken at the end of 6 months. All adverse events during immediate postoperative and other follow-up time points were recorded. While patients with a curve magnitude ≥50° were considered for surgical deformity correction; additional non-surgical interventions like bracing were considered for skeletally immature (Risser 0, 1, or 2) patients with an interim curve progression ≥5°. Additional shunt procedures for syrinx were performed for those who had a persistent or worsening syrinx, which was causing deterioration in neurological status. At each postoperative visit, all of the aforementioned clinico-radiological parameters were evaluated. At each preoperative and postoperative visit, a detailed comparison of the deformity characteristics (on plain radiographs) and the morphology of syrinx and tonsillar herniation (on MRI) was made and statistically analyzed.
2. Statistical analysis
The statistical analysis was performed using IBM SPSS software for Windows ver. 24.0 (IBM Corp., Armonk, NY, USA). Curve parameters, syrinx morphology, and tonsillar descent were among the clinical, demographic, and radiological parameters analyzed. The chi-square and analysis of variance test were used for categorical values between two or three groups. An independent t-test was performed to compare the statistical significance of the association for continuous data. Results were expressed as the mean±standard deviation, with a p-value of <0.05 considered statistically significant.
Results
The study included 42 patients in total. The patients’ average age was 14.2±5.8 years, and there were 20 female patients (six of whom were premenarchal) (Table 1). Sixteen patients (38.1%) had an abnormal superficial abdominal reflex (SAR; absent on the right, left, and bilaterally in three, eight, and five patients, respectively). The rest of the neurological examinations were all normal in all of the patients.
1. Preoperative deformity characteristics
In this series, 35 patients (83.3%) had atypical curves (Table 2). Of these patients, 24 had a left-sided deformity, 13 had apical hyperkyphosis, six had long “C” curves, three had high thoracic or cervicothoracic curves, and one had short acute scoliosis. The apex of major scoliotic curvature was found in 6 (14.3%), 29 (69%), and 7 (16.7%) patients, respectively, at the proximal thoracic (T1–T6), main thoracic (T6–T7 disk to T11), and thoracolumbar or lumbar (T11–12 disk to L5) levels. Only one major structural curve was found in 32 (76.2%) of the patients, while double-major curves were found in 10 (23.8%) of the patients. Risser grading was used to grade skeletal maturity, and grades 0 (open tri-radiate in 10 patients), 1, 2, 3, 4, and 5 were found in 18 (42.9%), 3 (7.1%), 4 (9.5%), 2 (4.8%), 4 (9.5%), and 11 (26.2%) of the patients, respectively.
The coronal plane deformity (Cobb angle) had a mean magnitude of 57.7°±20.9° before surgery. There were 1 (2.3%), 8 (19%), 12 (28.6%), 13 (31%), and 8 (19.1%) patients with apical vertebral rotations of grades 0, 1, 2, 3, and 4, according to Moes’ classification. Twelve patients (28.6%) had significant coronal imbalance (≤1.9 cm in one, 2–4.9 cm in height, and ≥5 cm in three). Four patients (9.5%) had a significant (≥5 cm) sagittal imbalance (three positives and one negative). Seven patients (16.7%) had significant pelvic obliquity (≤1.9 cm in five patients, 2–4.9 cm in one patient and ≥5 cm in one patient). The mean preoperative thoracic kyphosis (TK), lumbar lordosis (LL), thoracolumbar kyphosis (TLK), pelvic incidence (PI), and sacral slope (SS) were 46.3°±18.4°, 58.3°±13.1°, 6.8°±8.6°, 44.5°±10.1°, and 36.4°±11.1°, respectively.
2. Morphology of tonsillar descent and features of the syrinx
In 16 (38.1%), 11 (26.2%), and 15 (35.7%) patients, the descent of cerebellar tonsils was graded as grade 1, 2, or 3 (Table 3). An asymmetric tonsillar descent was found in the majority of our patients (35 patients, 29 with right-sided dominant descent, and six with left-sided dominant descent). On coronal MRI, the tonsils had a mean maximum descent of 13.6±4.1 cm (the mean descents on the right and left halves of the cerebellar tonsils on coronal sections were 13.2±4.3 cm and 10.6±3.2 cm, respectively).
Seventeen (40.4%), 3 (7.1%), 16 (38.1%), and 6 (14.4%) patients presented with circumscribed, moniliform, dilated, and slender patterns of the syrinx. Nine (21.4%), 12 (28.6%) and 21 (50%) of syrinx were right-sided, left-sided, or centric in location. The mean preoperative length and diameter of syrinx were 12.5±4.9 mm and 8.4±4.7 mm, respectively; while the mean S/C ratio was 0.7±0.2.
3. Comparison between atypical and typical curves
Patients with typical and atypical curves had similar clinico-radiological characteristics, such as sex distribution (p=0.86), magnitude of preoperative coronal (Cobb angle) deformity (“atypical” 58° versus “typical” 48.5°, p=0.68), apical rotation (Moe’s grades, p=0.27), grade of tonsillar herniation (p=0.82), and asymmetry of tonsil.
4. Relationship between abdominal reflex and tonsillar or syrinx morphology
There was no statistically significant relationship between the status of abdominal reflex and the symmetry of syrinx deviation (right/left or centric) (p=0.29) or side of dominant tonsillar descent (p=0.79).
5. Association between syrinx and tonsillar morphology and curve characteristics
There was no statistically significant relationship between deformity pattern (high thoracic, double or single major, long thoracic, or typical) and major curve side (convexity to right/left) (p=0.39). We found no statistically significant link between the side of tonsillar descent and the side of syrinx deviation (p=0.30). There was no statistically significant relationship between the side of tonsillar dominance (p=0.31), the extent of tonsillar descent (grades 1, 2, and 3; p=0.30), and major curve convexity. There was, however, a statistically significant relationship between the side of syrinx deviation (right, left, or centric) and the side of major curvature (right or left) (p=0.01). In other words, scoliosis convexity tended to correlate with the dominant side of the syrinx.
6. Posterior fossa decompression and its effect on curve progression and syrinx morphology
All patients in this series underwent PFD. One of the patients had an incidental dural leak, two had wound dehiscence (which required re-suturing), and one had a superficial wound infection (which necessitated debridement). There were no major neurological complications. Following PFD, skeletally immature children (Risser 0, 1, or 2) with Cobb ≥25° or interim curve progression ≥5° underwent bracing. Plain radiographs obtained at each postoperative visit were used to assess the deformity progression serially. At 6 months after PFD, all patients underwent MRI to evaluate syrinx morphology and progression.
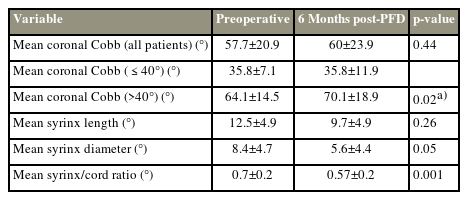
The overall mean coronal Cobb angle at 6-months post-PFD was 60°±23.9° (Table 4). In curves with magnitude ≤40°, there was significantly better stabilization of scoliosis, as compared with curves of larger magnitude (p=0.02). Although patients younger than 10 years of age showed a trend toward greater curve deformity stabilization when compared to older patients, the difference was not statistically significant (possibly due to a smaller number of younger patients; p=0.49). The curve stabilization after PFD did not significantly differ between atypical and typical curves (p=0.38). The extent of preoperative tonsillar descent (grades 1, 2, or 3) or size of the syrinx (S/C ratio ≥0.7 versus <0.7) did not significantly affect the degree of stabilization of deformity after PFD (extent of tonsillar descent: p=0.13; syrinx size: p=0.26).
Overall, there was a significant reduction in syrinx size following PFD (at 6-month follow-up). Although mean syrinx length (9.7°±4.9°) and diameter (5.6°±4.4°) were numerically smaller than the preoperative status (mean syrinx length [12.5°±4.9°] and diameter [8.4°±4.7°]), the differences were not statistically significant (p>0.05). There was a statistically significant reduction in the S/C ratio post-PFD, as compared with preoperative status (pre-PFD 0.76 versus post-PFD 0.53, p<0.001). Only one patient with persistently large syrinx required syringe-subarachnoid shunt (SSAS) at 3 months post-PFD, following which she recuperated well.
7. Curve progression and outcome after surgical deformity correction
At 6 months post-PFD, 26 patients had a curve of magnitude ≥50° (Table 5). Twenty-three of them had their deformities corrected surgically. At our institution, all deformity correction procedures were performed no sooner than 6 months after PFD as a standard procedure. One of the patients underwent selective thoracic fusion (T4–L1); and all others underwent longer segment fusions (seven patients: T4–L4; seven patients: T4–L3; three patients: T2–L3; two patients: T2–L4; two patients: T3–L3; one patient: T3–L3). Four patients with severe deformities received 6 weeks of halo-gravity traction before surgery. All surgeries were performed through posterior-only approaches. There were no neurological side effects. Two patients had minor wound dehiscence (which required re-suturing) and two had significant ileus following surgery. At the final follow-up at 2 years post-deformity correction, mean coronal deformity improved from 57.7°±20.9° to 32.6°±12.3° (p=0.001). There was no statistically significant difference in the final deformity correction achieved between atypical and typical curves (“atypical” 14.2° versus “typical” 18.3°, p=0.39).
Discussion
It is well-acknowledged that a subset of children with “presumed idiopathic scoliosis” may have an underlying abnormality of the neural axis [13]. The most common such anomalies include ACM-I and SM, which are primarily diagnosed on MRI [1,13]. Although factors like age, sex, and certain clinical findings (e.g., stigmata of spinal dysraphism, abnormal SAR, etc.) may indicate the possibility of underlying neuraxial abnormalities, a few radiographic guidelines have also been put forth to help clinicians in suspecting such neural axis disorders in scoliotic children with normal clinical examination [4]. The identification of “atypical curves” assumes a major significance in this context, as it has been well-demonstrated that such curve patterns have a higher frequency of association with abnormal neural axis [1,13,14].
ACM-I is a congenital hindbrain disorder that results from abnormal development of para-axial mesoderm [15]. It is defined as a caudal migration of cerebellar tonsils ≥5 mm below the foramen magnum [16]. ACM can result in the development of spinal syrinx, and syrinx can lead to scoliosis as a result of asymmetrical insult to the spinal cord secondary to an expanding cyst [14]. ACM has been associated with scoliosis even in the absence of syrinx [13]. This phenomenon has been explained by the truncal imbalance due to asymmetrical compression of the cervicomedullary junction by asymmetrically herniated cerebellar tonsils [16,17]. Researchers have also reported scoliotic curves in patients with idiopathic SM, in the absence of ACM [14]. The current study was designed to evaluate our experience with patients who underwent PFD after being diagnosed with ACM-I, SM, or scoliosis.
In our series, one-third of the patients (14 patients) were 16 years or older, which is the typical (and relatively late) pattern of presentation in developing countries. SAR was abnormal in about 38% of the people. The side of abnormal SAR, on the other hand, did not correspond to the side of tonsillar descent or syrinx. Fujimori et al. [18] had previously reported a strong association between abnormal SAR and SM. They concluded that abnormal SAR had sensitivity, specificity, positive predictive value, and negative predictive value for SM in a patient with presumed idiopathic scoliosis of 89%, 95%, 80%, and 98%, respectively. None of the patients in our series had any signs of major sensorimotor, lower cranial nerve, or evidence of medullary dysfunction.
Atypical scoliotic curve patterns were found in about 83% of our patients. Atypical patterns included left-sided convexity and apical hyperkyphosis. A double major curve pattern appeared in 23.8% of cases. Zhu et al. [1] observed that the thoracic spine in patients with scoliosis tended to be convex on the dominant side of an asymmetrically-displaced tonsil as well as the deviated side of an eccentrically-located syrinx. In their series, 66.7% had asymmetric tonsillar descent and 74.4% had an eccentrically-located syrinx. In our study, we could observe that the convexity of scoliosis was more commonly located on the same side as an eccentrically-located syrinx [1,4,14]. We were unable to find a statistically significant relationship between the side of tonsillar descent and the side of scoliosis. In our study, 83.3% of patients had asymmetrically descended cerebellar tonsils, and 50% had an eccentric syrinx. These findings support the role of spinal cord dysfunction in the pathogenesis of SM-associated scoliosis. Sun et al. [15] also reported that the position of cerebellar tonsils in a cohort of 206 children with “presumed idiopathic scoliosis” did not significantly differ with different curve patterns or severity, although there was a higher incidence of tonsillar ectopia in children with atypical curves or double thoracic curves.
Fujimori et al. [18], in their study, had observed that patients with SM requiring surgery had a mean preoperative Cobb angle of 78° (range, 56°–105°) and mean curve flexibility of 58% (range, 50%–78%). They concluded that SM presented with more severe and rigid curves, in comparison with idiopathic deformities. Of the patients, 33% had a severe deformity of magnitude >70° and 76.2% had significant apical vertebral rotation (Moe’s grade ≥2). Zhu et al. [12] observed that sagittal spinopelvic parameters (including TK, LL, PT, and SS) in patients with ACM and scoliosis were significantly different from those with idiopathic scoliosis. While the PT was significantly lower in these patients, TK was relatively higher. We could also observe a higher prevalence of apical thoracic or TL hyperkyphosis (31%) in our patients.
Previous studies have reported good results following bracing in patients with scoliosis secondary to ACM-I, although the outcome has not been as successful in those with associated SM [19]. Sha et al. [19,20] reported that bracing after PFD was effective in preventing curve progression in 62% to 64% of patients with ACM. This result was significantly better than those who were only observed (where the curve stabilized in only 30% of patients). After PFD, all patients who were eligible for bracing (Risser 0, 1, 2; curve magnitude between 25° and 50°; interim progression of the curve by at least 5°) were advised to wear an additional brace.
Yeom et al. [8] observed that early diagnosis and decompression of syrinx in scoliosis before 10 years of age was crucial in decreasing the curve size and limiting scoliosis progression. A previous study by Brockmeyer et al. [21] also revealed an excellent outcome after PFD in ACM-I patients younger than 10 years, where the surgery could halt scoliosis progression in 91% of situations. We found no significant difference in curve stabilization after PFD in younger children (as compared to children >10 years) in our study. This observation could, however, be because our cohort had a smaller number of younger children. Although our observations suggest that PFD can potentially stabilize deformities of less than 40°, its role in stabilizing deformities of larger magnitudes is unclear and needs to be investigated further. Many previous studies have made the same observation [1,4,8,10,14].
In all patients who present with a combination of ACM-I, SM, and scoliosis at our institution, we prefer to perform PFD first. Additional shunt procedures are performed in patients whose syrinx size is persistently large or whose neurological status is deteriorating. There was no neurological deterioration in this series of patients after PFD. One patient, however, had a persistently large syrinx that necessitated an SSAS procedure three months after PFD. All deformity correction surgeries are performed no sooner than 6 months after PFD as a standard procedure at our institution. We had no neurological complications with this approach in the current series.
We could observe a significant reduction in the size of the syrinx (as revealed by a significantly reduced S/C ratio) after PFD. Even based on the evidence in the literature, a significant proportion of patients with ACM-I have a substantial reduction in syrinx size with PFD alone [11]. Zhu et al. [6] recommended that neurosurgical procedures are necessary for patients presenting with syringomyelia when the S/C ratio is greater than 0.7 (in large syrinx). In this series, 23 patients underwent definitive deformity correction surgery. While the literature has suggested a good outcome in these patients even with selective thoracic fusion [9], only one patient was amenable to a selective fusion procedure. All patients had a satisfactory outcome with the achievement of adequate fusion at the end of 2-year follow-up.
We did not include a control group of people with idiopathic scoliosis in our study to compare curve characteristics and morphology. In our study, we observed all of the inherent flaws of a retrospective trial. Alternative management strategies such as definitive fusion without prior PFD, single-staged PFD and deformity correction, or regular shunt procedures for the syrinx were not compared. The follow-up MRI was obtained at 6 months after PFD, despite the fact that only patients with at least 2 years of clinical follow-up were included in this retrospective study. Nonetheless, we were able to see excellent results from our management team. This is one of the largest studies heretofore published, which not only discuss the characteristics of deformities in these rare scenarios but also elaborates upon the outcome following PFD and deformity correction.
Conclusions
A majority of patients with ACM-I and SM present with atypical curve patterns. In our cohort, the side of syrinx deviation correlated significantly with the convexity of scoliosis. PFD, followed by surgical deformity correction is a safe approach in such scenarios with low neurological risk. PFD reduces the size of the syrinx by a significant amount. PFD may not play a significant role in the stabilization of scoliosis in curves with magnitudes >40°.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
VVK, SS, NR, and SH collected the data and prepared the manuscript. APS, RMK, and SR reviewed the manuscript, analyzed the data and supervised the preparation of manuscript. All authors read and approved the final manuscript.
Funding
We received funding from the Ganga Orthopedic Research and Educational Fund (GOREF).