Unilateral Cervical Facet Fractures: Relevance of Acute Disc Injury in Conservative Treatment Failure
Article information
Abstract
Study Design
Case-control study.
Purpose
Analyze association between imaging factors related to the failure of conservative treatment in isolated subaxial cervical facet fractures.
Overview of Literature
Facet fracture (F1, F2, and F3 AOSpine) may be stable or unstable depending on clinical and imaging variables, which are not well established. As a result, differences in fracture management lead to differences in surgical or conservative indications, and there is no evidence to predict conservative treatment failure.
Methods
Patients were categorized into two groups: six patients (16.2%) with conservative treatment failure (defined as the appearance of neurological symptoms, listhesis >3.5 mm, kyphotic deformation >11°, and/or non-union), and 31 patients (83.7%) with successful conservative management (defined as complete consolidation confirmed by computed tomography [CT] at the 6-month follow-up). All participants were fitted with rigid collars of the Miami type, and standardized follow-up was performed until consolidation or failure. CT and magnetic resonance imaging (MRI) was used to examine imaging characteristics. Sagittal balance parameters were assessed using CT, and signs of acute disc injury, prevertebral edema, facet synovitis, and interspinous hyperintense signal were assessed using MRI.
Results
Thirty-seven patients were diagnosed with unilateral cervical facet fractures between 2009 and 2020. In this sample, acute disc injury had a significative association to failure of conservative treatment in F2 and F3 AOSpine facet fractures, 100% of the failure group presented with traumatic disc injury compared to 9.7% of the successful group, for the other variables: prevertebral edema, 83.7% vs. 41.9%; facet synovitis, 100% vs. 77.4%; and interspinous hyperintensity, 71.4% vs. 38.7%, respectively. With conservative management, all F1 fractures healed successfully. Conservative treatment failed in 20% of F2 fractures and 50% of F3 fractures, respectively. In terms of cervical sagittal balance parameters, there were no significant differences between groups.
Conclusions
Conservative management was successful in all F1 fractures. In F2 and F3 types, there was a significant association between acute disc injury and conservative treatment failure.
Introduction
Isolated, non-displaced, or minimally displaced facet fractures (F1, F2, or F3 based on the AOSpine classification) [1] account for <5% of all cervical spine fractures [2]. Fractures may be stable or unstable in the same pattern of bone injury, depending on other clinical and imaging variables. However, these variables are not well established [3], making it difficult to understand and reach a consensus in the management of these injuries. Multiple studies and classifications have been developed in an attempt to understand the biomechanical behavior of these lesions and standardize treatment, such as the subaxial cervical spine injury classification score, which sent the AOSpine classification to its bases [1]. Furthermore, fracture management differences lead to variations in surgical or conservative treatment indications for F2 and F3 fractures. Currently, there are no publications with a high level of evidence that can reliably predict conservative treatment failure [4].
The present study aimed to analyze imaging factors associated with the failure of conservative treatment, in isolated fractures of the lateral mass that could be determinants in the decision of surgical treatment.
Materials and Methods
1. Participants
Case-control studies were conducted on patients with F1, F2, and F3 fractures based on the AOSpine classification.
Between 2009 and 2020, a total of 47 patients were treated in a level one trauma center. Following approval from local institutional ethics committee (CEC HT-24/2020), informed consent was obtained from all individual participants included in the study. To ensure the protection of each patient’s identity, the registry was also compiled by nonsequential coding. Ten patients were excluded as they presented one or more of the following criteria: injury at more than one level, emergency surgery due to neurological compromise, radiological instability according to the White-Panjabi criteria (kyphotic deformation >11° and listhesis >3.5 mm) [5], incomplete registration, or less than 6 months of follow-up.
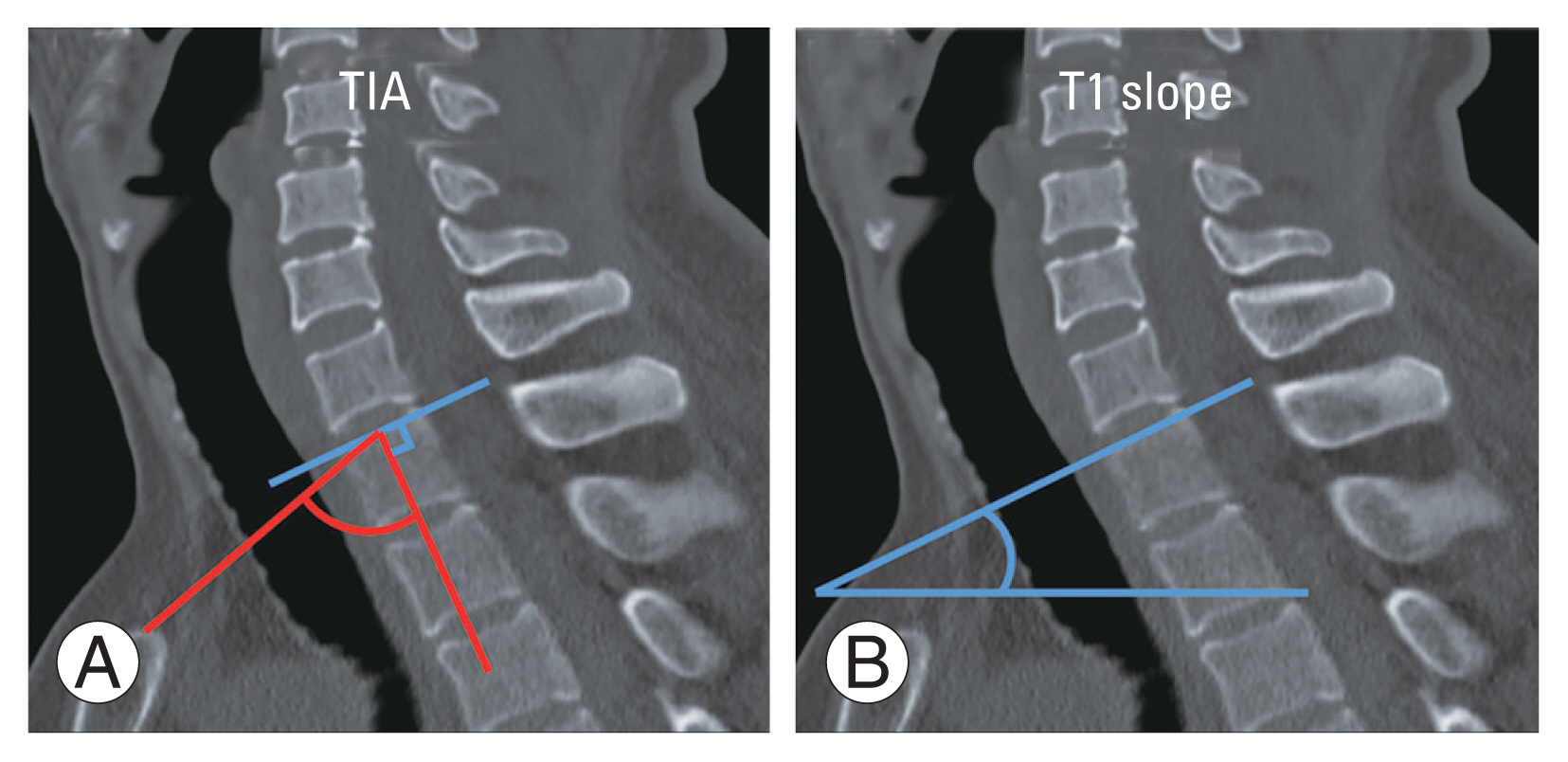
There were 37 people in total, with a median age of 41 years (range, 21–71 years), 91.8% of whom were men and 8.1 percent of whom were women. Car accidents (62.1%) were the most common cause of injury, followed by falls from a great height (37.8%) (Table 1).
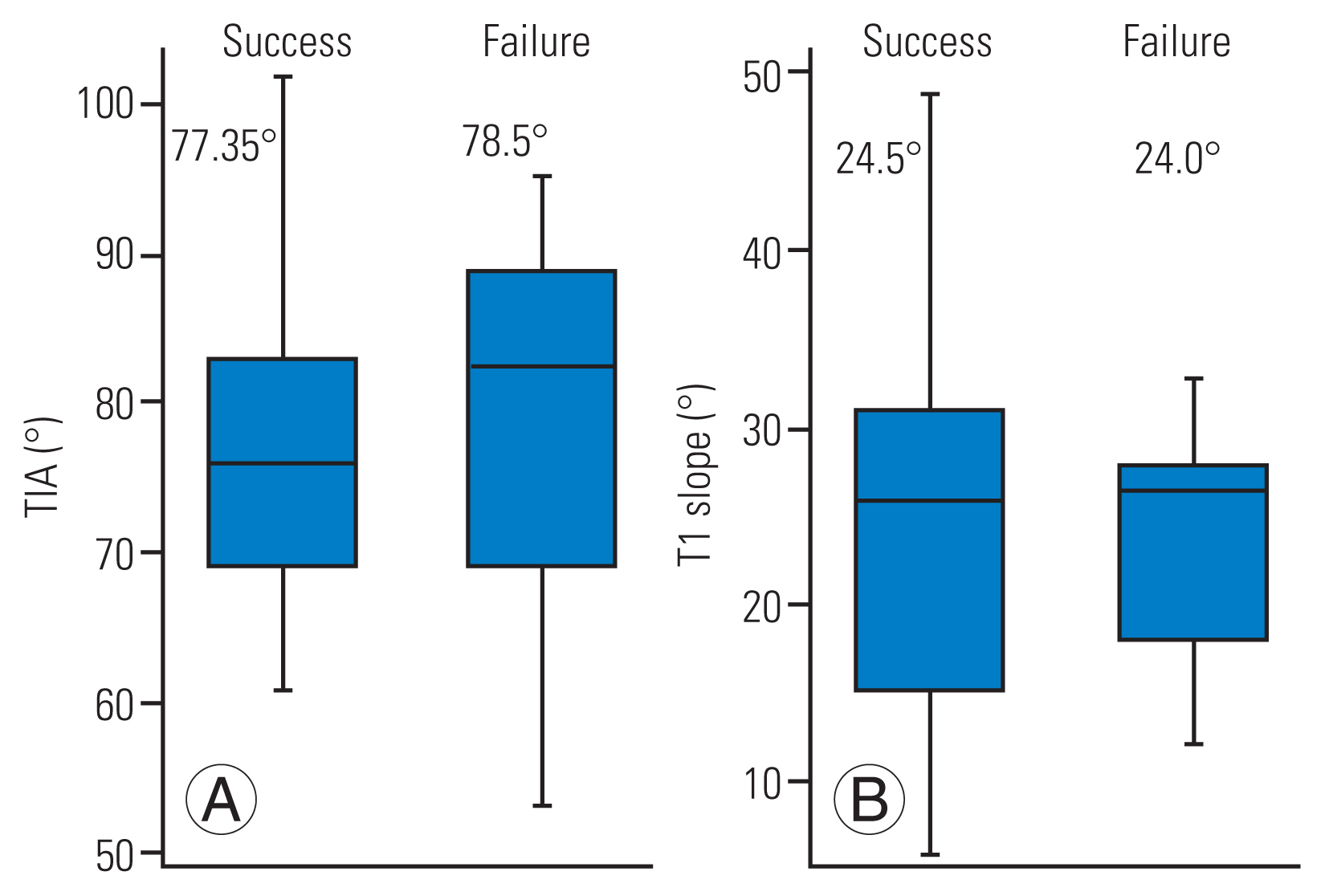
Demographic characteristics and mechanism of injury in the failure and successful groups who underwent conservative treatment
All patients received conservative treatment with a cervical collar (Miami-J). Of the 37 eligible patients, six patients were classified as “cases” as they presented with conservative treatment failure (Table 2, Fig. 1). This failure was defined as the onset of neurological symptoms, development or progression of listhesis >3.5 mm, bisegmental angulation >11° or non-union. In contrast, the 31 patients who evolved successfully (complete consolidation confirmed by computed tomography [CT] at the 6-month follow-up) were classified as “controls.” Depending on availability at the time of patient admission, all patients underwent CT scanning (Diamond Select Brilliance CT 16 channels; Philips, Amsterdam, The Netherlands) and magnetic resonance imaging (MRI; Phillips Ingenia 1.5 or 3.0 Tesla).

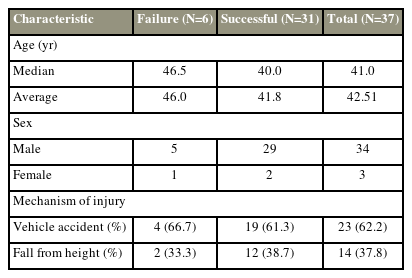
Images case # 1. (A, B) Computed tomography: sagittal and axial view of case #1, C6 A0 F2 left N0 AOSpine, and (C) magnetic resonance imaging of C6–C7 acute disc injury.
The AOSpine classification of fractures and the level of injury were designated as variables to be evaluated.
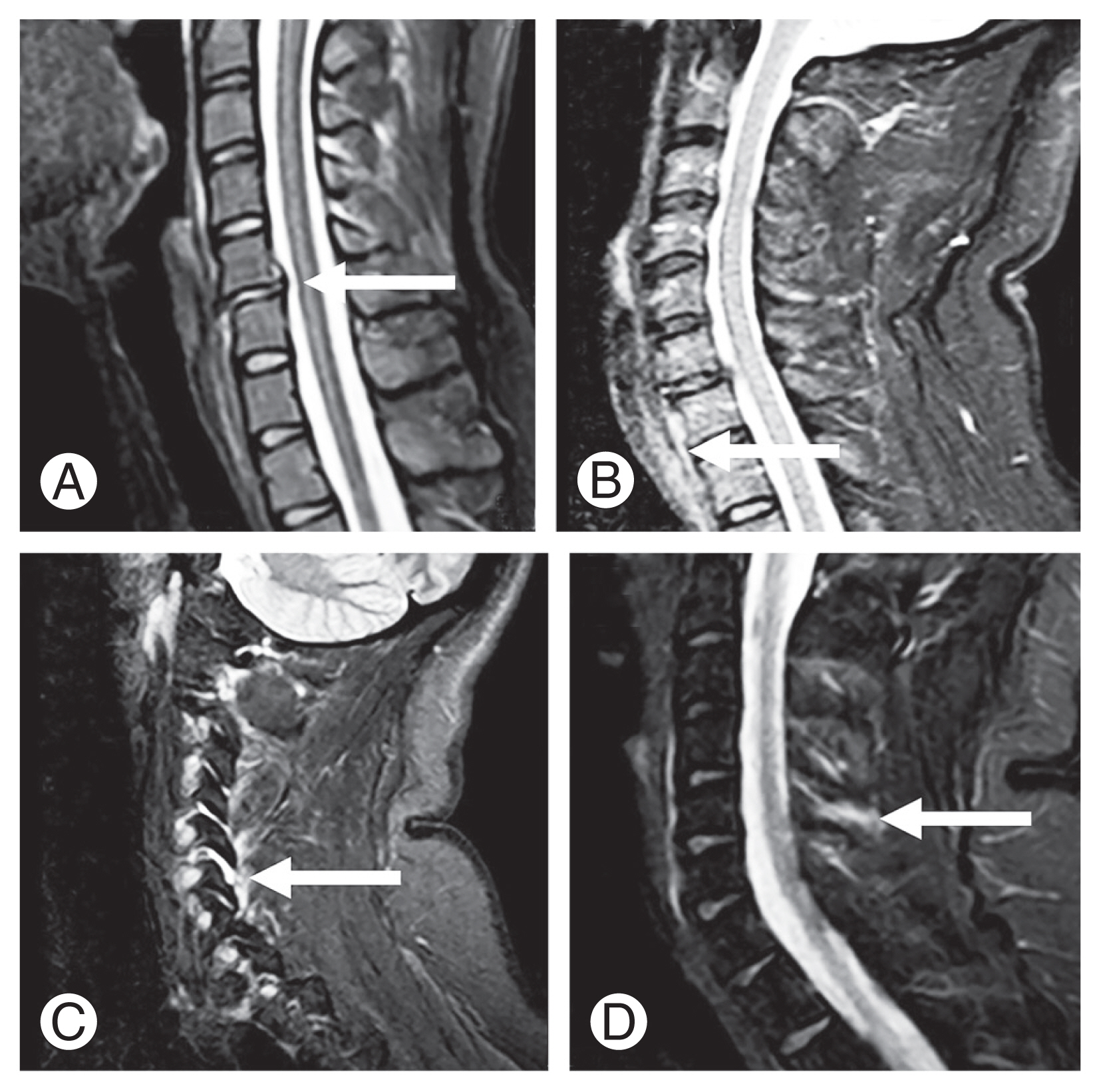
The following MRI findings were examined: signs of acute disc injury in the affected segment (defined as the presence of a hyperintense image of the fibrous ring and/or signs of acute herniation in fat suppression sequences STIR [short inversion time inversion recovery], SPAIR [spectral adiabatic inversion recovery], or fat-saturation), the presence of prevertebral edema, facet synovitis of the injured segment, and signal alteration in the interspinous space (Fig. 2). Furthermore, the following cervical sagittal balance parameters were evaluated on radiographs or CT (according to availability): thoracic inlet angle (TIA) and T1 slope (Fig. 3) [6].
Magnetic resonance imaging findings of the cervical spine (represented by the white arrow). (A) Acute disc injury at C5–C6. (B) Prevertebral edema at C7–T1. (C) Facet synovitis at C5–C6. (D) Interspinous hyperintensity at C4–C5 in the fat suppression sequence SPAIR (spectral adiabatic inversion recovery).
(A) Thoracic inlet angle (TIA) refers to the angle between the line drawn from the proximal edge of the sternum perpendicular to the center of the upper endplate of T1 and the horizontal. The normal is between 17.5° and 30°, with an average of 23° [17]. (B) T1 slope refers to the angle formed between the upper platform T1 and the horizontal line. The normal is between 63° to 81°, with an average of 72° [18].
2. Statistical analysis
For categorical variables, Fisher’s exact test was used to estimate the values between patients with success and conservative treatment failure. For continuous variables, Student t-test was used, with the significance level set at 0.05.
The imaging studies were evaluated using the Agfa Xero Viewer ver. 8.1.2 (2017) software (Agfa HealthCare, Mortsel, Belgium). Statistical analysis was performed using Stata ver. 12.0 (Stata Corp., College Station, TX, USA; license: 936-11859-953). Moreover, graphs were created using GraphPad Prism software ver. 9.0 (GraphPad Software, San Diego, CA, USA).
Results
1. Injury morphology
All F1 fractures evolved without conservative treatment failure. Among patients with F2 and F3 fracture types, 20% and 50% presented with failure, respectively. The differences between the three types of fractures were significant (chi-square test, p=0.016). On analyzing the frequency of conservative treatment failure to the lesion level (Table 3), no significant associations were detected.
2. Analysis of magnetic resonance imaging findings
Acute disc injury was significantly associated with conservative treatment failure (100% compared to 9.67% in the successful treatment group [Fisher’s exact test, p<0.01]). Furthermore, prevertebral edema was more common in the treatment failure group (83.3%) than in the successfully conservatively managed group (41.9%), but this was not statistically significant (Fisher’s exact test, p=0.09). Facet synovitis and interspinous hyperintensity were not associated with conservative treatment failure. Multivariate analysis confirmed that acute disc injury showed a significant association with conservative treatment failure (Fig. 4).

Magnetic resonance imaging findings expressed as percentages per group: success group (black) and failure group (gray). Statistical calculation of Fisher’s exact test. Disc injury: difference=0.90, z=4.72 (*p<0.01); prevertebral edema: difference=0.41, z=1.36 (p=0.09); facet synovitis: difference=0.22, z=1.29 (p=0.19); interspinous hyperintensity: difference=0.27, z=1.27 (p=0.20).
3. Cervical sagittal balance
In the failure group and successful group, the mean TIA was 78.5° and 77.35° (two-sample t-test, p=0.81), while the T1 slope was 24.0° and 24.5° (two-sample t-test, p=0.90), respectively. Thus, no significant associations were found (Fig. 5).
Discussion
The management of facet fractures remains controversial [6–8]. The classification and management algorithms for these injuries are based on studies with a limited number of patients and a low level of evidence [9–11]. Spector et al. [12] published a review of 24 cases using CT for imaging evaluation. They showed that the most relevant risk factor for conservative treatment failure was an articular mass fragment with a height of >1 cm and/or a >40% involvement. It is important to note that the study of Spector et al. [12] provides scientific support for the AOSpine facet classification, based on a total of 24 cases with low statistical significance, in a methodologically very correct work but with the statistical limitation of one low prevalence pathology. So, this was adopted as the criterion for differentiating F1 from F2 fractures in the AOSpine classification [1].
Currently, there is a scarcity of literature evaluating the usefulness of MRI in the decision-making for the treatment of these injuries. Halliday et al. [13] proposed that three of four ligament structures had been injured: the joint capsule, anterior longitudinal ligament, posterior longitudinal ligament, and interspinous ligament. This was linked to segment instability, allowing conservative treatment failure to be predicted [13]. Furthermore, Ha et al. [14] reported that in a sample of 27 patients, 41% had acute disc injury; however, they did not identify this as a determinant of instability. Caravaggi et al. [15] performed a biomechanical study and found a significant relationship between disc injury and instability associated with a mass fracture. In particular, under physiological loading conditions, instability was not always observed in injuries with at least 40% compromised articular mass but no associated disc injury [15].
In our experience, the disc is an indicator of the stability of the subaxial spine. In contrast, the posterior ligamentous complex in the cervical spine has lesser biomechanical relevance than that in the thoracolumbar spine. In our study, all surgical patients had a traumatic disc injury, whereas interspinous hyperintensity and facet synovitis were not directly associated with conservative treatment failure.
Given the importance of the disc, we consider that it is necessary to evaluate this structure and its relation to instability in isolated fracture of the lateral mass. As a result, MRI plays a critical role in defining its damage. This is especially true for F2 and F3 fractures, as none of the F1 fractures presented with a conservative treatment failure.
Finally, the current literature is segmented with optimal treatments for facet fractures. The success rates of conservative treatment highly vary from 20% to 80% [16]. Nevertheless, there is a high degree of consensus among spine surgeons regarding the diagnostic value of MRI. According to a survey conducted by the AOSpine Latin America Trauma Study Group, 53.5%, 76%, and 89.1% of the 229 surgeons polled requested MRI for F1, F2, and F3 fractures, respectively [17]. As a result, our findings imply that for injuries classified as unstable (F2 and F3) [18–21], conservative management is possible, as long as the MRI study confirms the absence of lesions of structures associated with failure, such as disc and prevertebral edema. Thus, F2 and F3 fractures are not unstable due to their morphology. In our study, 80% of F2 and 50% of F3 fractures were successfully managed conservatively.
In consideration of the low sample size of the group of cases (n=6), we estimated sample size through power analysis, with a significance of 0.05, statistical power, and effect size of 80%, the number of cases corresponds to 25, which due to the low prevalence of this pathology would require 33 years of case records, a number that is probably difficult to achieve for a monocentric study, but which can lay the foundations for a multicenter study that allows for greater statistical support to the findings of the same.
The strengths of this study are as follows. All patients underwent an imaging study with CT and MRI on admission. The surgical indication was standardized according to the team consensus. This study was backed up by scientific evidence, and we looked at factors that hadn’t previously been considered in determining prognosis in these lesions. The retrospective design and small sample size of this study are two of its limitations. Given the low prevalence of these types of lesions, our findings call for a prospective longitudinal multicenter study with a larger sample size.
Conclusions
In summary, all patients with F1 fractures evolved satisfactorily with conservative treatment, with or without an associated disc injury. In contrast, when comparing patients with F2 and F3 fractures to those with other evaluated structures, the association of disc injury with conservative treatment failure was significant. As a result, systematic use of MRI should be considered as a diagnostic tool from the start of treatment (particularly when F2 and F3 fractures are present) to define surgical treatment options; however, additional multicentric studies are needed to back up these findings.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.