Clinical and Radiographic Comparisons among Minimally Invasive Lumbar Interbody Fusion: A Comparison with Three-Way Matching
Article information
Abstract
Study Design
Retrospective cohort study.
Purpose
To compare clinical and radiographic outcomes among minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF), extreme lateral lumbar interbody fusion (XLIF), and oblique lateral lumbar interbody fusion (OLIF) techniques.
Overview of Literature
To date, there are many reports comparing outcomes between MIS-TLIF and XLIF, MIS-TLIF and OLIF, or XLIF and OLIF procedures. However, there are no previous studies comparing clinical and radiographic outcomes among all these three techniques.
Methods
Data from patients who underwent minimally invasive (MI) fusion surgery for lumbar degenerative diseases at L4–L5 level was analyzed. Thirty patients each from MIS-TLIF, XLIF, and OLIF groups were recruited for propensity score matching. Visual Analog Scale (VAS) of the back and legs and Oswestry Disability Index (ODI) were evaluated preoperatively and at 1, 3, and 6 months and 1 year postoperatively. Radiographic outcomes were also compared. The fusion rate was evaluated at 1 year after surgeries.
Results
The clinical outcomes were significantly improved in all groups. The disk height was significantly restored in all groups postoperatively, which was significantly more improved in XLIF and OLIF than MIS-TLIF group (p<0.001). The axial canal area was significantly increased more in MIS-TLIF versus XLIF and OLIF (p<0.001). The correction of lumbar lordotic angle and segmental sagittal angle were similar among these techniques. OLIF and XLIF groups showed less blood loss and shorter hospital stays than MIS-TLIF group (p<0.001). There was no significant difference in fusion rate among all groups.
Conclusions
MIS-TLIF, XLIF, and OLIF facilitated safe and effective MI procedures for treating lumbar degenerative diseases. XLIF and OLIF can achieve clinical outcomes equivalent to MIS-TLIF by indirect decompression. XLIF and OLIF showed less blood loss, shorter hospital stays, and better disk and foraminal height restorations. In single-level L4–5, the restoration of sagittal alignment was similar between these three techniques.
Introduction
Lumbar interbody fusion has been popularized for surgical treatment in patients with chronic back pain with or without radiculopathy [1]. Open approaches such as posterior lumbar interbody fusion and transforaminal lumbar interbody fusion (TLIF) reportedly have high success rates. However, these techniques have some disadvantages, such as more postoperative pain, more blood loss, and prolonged length of hospital stays. Minimally invasive (MI) lumbar interbody fusion has been also provided good clinical outcomes with fewer complications. Its advantages include less blood loss, shorter operative times, less postoperative pain, and shorter length of hospital stays than conventional open procedures. Moreover, MI techniques are also popular in obese and elderly patients with multiple medical comorbidities [2–6].
In this study, we focused on three common MI techniques: minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF), extreme lateral lumbar interbody fusion (XLIF), and oblique lateral lumbar interbody fusion (OLIF). The MIS-TLIF delivers direct decompression of spinal canal via unilateral access to the spinal canal and intervertebral foraminal space. The XLIF involves accessing the targeted disk space via a lateral retroperitoneal, transpsoas corridor, and provides indirect decompression of spinal canal. Lastly, OLIF also provides indirect decompression effect but involves accessing the disk space via a corridor between great vessels and psoas muscle (Fig. 1) [1,5]. The outcomes of these MI techniques are favorable [4,5,7,8].
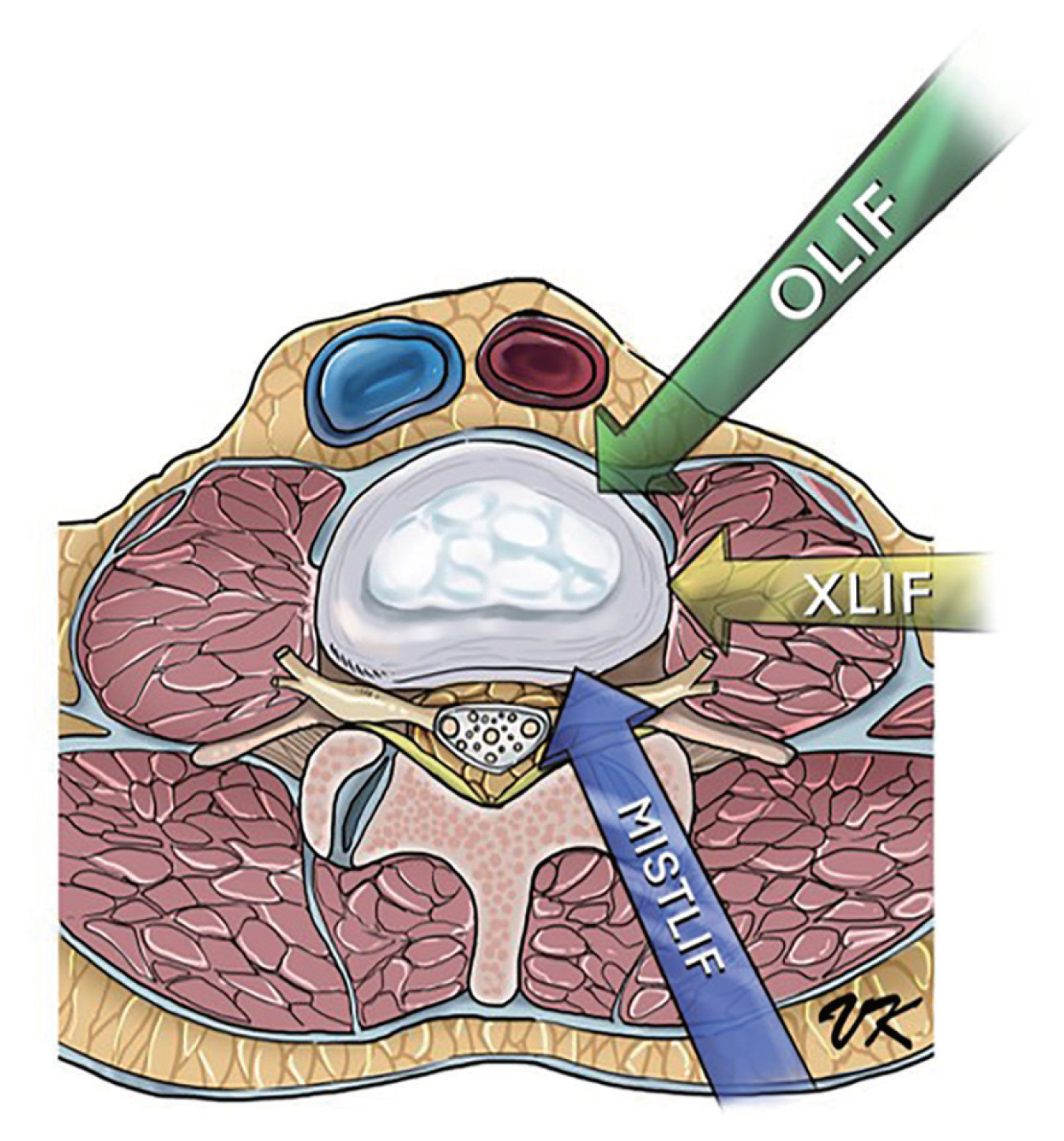
Schematic drawing of different techniques of minimally invasive lumbar interbody fusion. MIS-TLIF, minimally invasive transforaminal lumbar interbody fusion; XLIF, extreme lateral lumbar interbody fusion; OLIF, oblique lateral lumbar interbody fusion.
To date, there are many reports comparing clinical or radiographic outcomes among these MI lumbar fusion surgeries. Some of these studies compared the outcomes between MIS-TLIF and XLIF [9,10], MIS-TLIF and OLIF [11], or XLIF and OLIF procedures [12,13]. However, there are no previous studies comparing clinical and radiographic outcomes among all these three techniques. Hence, this study aimed to compare clinical and radiological outcomes between MIS-TLIF, XLIF, and OLIF to help improve clinical practice guidelines on spinal surgery.
Materials and Methods
This retrospective study comparatively analyzed patients’ data collected from July 2016 to July 2019 from a single institution. This study was approved by the Institutional Review Board (IRB) of the Faculty of Medicine, Chulalongkorn University (IRB no., 478/62). Informed consent was obtained from all individual participants included in the study. All patients with lumbar degenerative diseases were treated by senior spinal surgeons who have performed more than 100 cases of each procedure.
1. Sample size calculation
The sample size of this study was calculated by using the formula: n/group=2(Zα/2+Zβ)2σ2/(μ1−μ2)2.
We applied type I error α=0.05, type II error β=0.20, and power of test=80% in this formula. The other variables were applied from a study of Lin et al. [11]. The canal diameter change in postoperative OLIF surgery was μ=50.66 square millimeters (mm2). The canal diameter change in postoperative surgery of MIS-TLIF was μ2=54.62 mm2, standard deviation=46.25 mm2. We calculated the population size equal to each group of operations in 30 cases.
2. Population
Altogether, 363 patients who underwent the operation were analyzed (MIS-TLIF=135, XLIF=126, and OLIF=102 cases). We used propensity score comparison for three-way matching, with 30 patients in each group, using the inverse probability of treatment weighting statistics of preoperative demographic data and preoperative clinical and radiographic outcomes for preventing selection bias [14]. Finally, 90 patients were included. The inclusion criteria were patients who underwent single-level MIS-TLIF, XLIF, or OLIF procedure at the L4–5 level for degenerative spine diseases, including low-grade spondylolisthesis, and lumbar spinal stenosis, where conservative management had failed to improve his/her symptoms. All patients were completely treated and had a minimum of 12 months of follow-up. Exclusion criteria were the presence of traumas, tumor, infection, previous lumbar spine surgery, severe spinal stenosis with cauda equina syndrome, and poor quality of imaging and follow-up information. Patients who underwent MIS-TLIF with over-the-top decompression on the contralateral side were excluded. Patients who underwent direct posterior decompression in XLIF and OLIF groups were also excluded. The patients in MIS-TLIF, XLIF, and OLIF groups were matched according to demographic data and preoperative clinical and radiographic parameters.
3. Surgical techniques
1) MIS-TLIF [7]
This procedure was performed by one author (W.S.) of this study. The patient was operated in prone position. The procedures included hemi-laminectomy, medial facetectomy, and ligamentum flavum removal on the approach side, discectomy, and endplate preparation. Then, the interbody cage (CAPSTONE; Medtronic, Minneapolis, MN, USA) filled with an autogenous local bone graft was inserted into the prepared disk space. Finally, supplement posterior instrumentation was placed percutaneously in standard fashion.
2) XLIF [12,15]
The XLIF procedure was performed by the author (W.Y.). Neurophysiological monitoring was applied to all patients to avoid lumbar plexus injuries during psoas muscle splitting. Patient was positioned in right lateral decubitus with the iliac crest placed on table break. The surgical approach was performed step by step to access the retroperitoneal space. The psoas muscle was identified and split. Then, a self-retaining retractor was applied. Discectomy and endplate preparation were performed. The proper-sized cage (Cohere; NuVasive Inc., San Diego, CA, USA) filled with demineralized bone matrix (DBM, ATTRAX; NuVasive Inc., San Diego, CA, USA) was inserted into the operated disk space. Lastly, the lateral plate was then fixed to the L4 and L5 vertebral bodies. The patient was subsequently turned into prone position after completion of the lateral procedure. Posterior instrumentation was performed percutaneously in this position.
3) OLIF [12]
This technique was performed by the author (W.L.). The patient was placed in the right lateral decubitus position. The surgical approach was performed to reach the retroperitoneal corridor between the psoas muscle and great vessels. The self-retaining retractor was placed upon the operated disk level after sequential dilators were applied. Thorough discectomy and endplate preparation were performed using the orthogonal maneuver. The appropriate-sized cage (CLYDESDALE; Medtronic) filled with DBM (GRAFTON; Medtronic) was inserted orthogonally into the operated disk space. Percutaneous posterior instrumentation was placed in prone position after completion of the lateral procedure.
4. Clinical evaluation
Functional outcomes regarding Visual Analog Scale (VAS) score and the Oswestry Disability Index (ODI) for low back pain were evaluated preoperatively and at 1, 3, and 6 months and 1 year postoperatively.
5. Radiographic evaluation
All patients obtained plain radiographs preoperatively and postoperatively. The anterior disk height (ADH), posterior disk height (PDH), foraminal height (FH), segmental sagittal angle (SSA), and lumbar lordotic angle (LLA) were measured (Figs. 2, 3). The ADH was defined as distance between anterior margin of inferior endplate of the L4 vertebra and anterior margin of superior endplate of the L5 vertebra on lateral radiograph. The PDH was measured as distance between posterior margin of inferior endplate of the L4 vertebra and posterior margin of superior endplate of the L5 vertebra on lateral radiograph. The FH was measured as the longest length between inferior edge of the L4 pedicle and superior edge of L5 pedicle on lateral radiograph. The SSA was assessed using an angle between inferior margin of L5 vertebral body and superior margin of L4 vertebral body. The LLA was defined as an angle between inferior margin of T12 vertebral body and superior margin of S1 vertebral body.
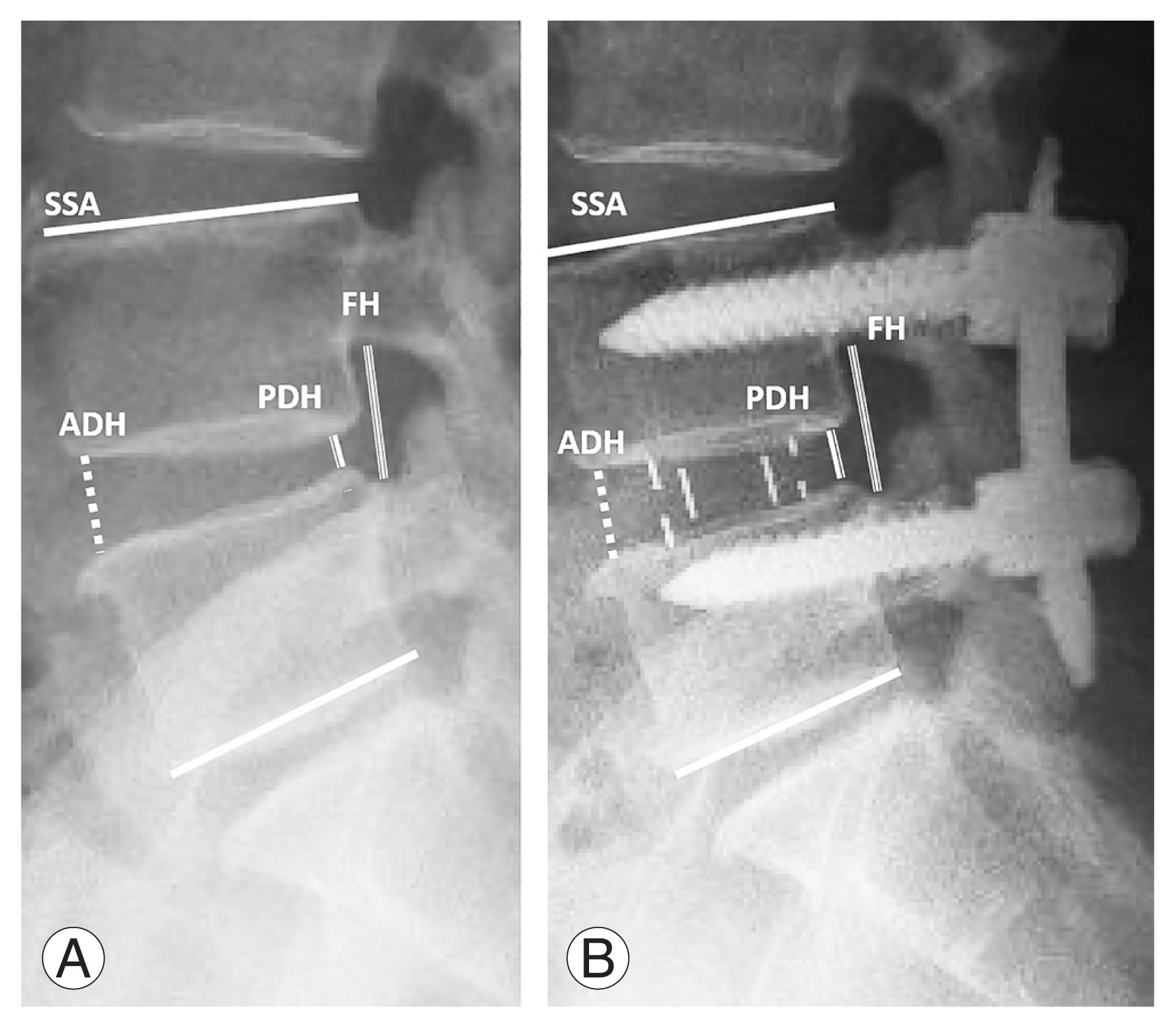
Anterior disc height (ADH), posterior disc height (PDH), foraminal height (FH), and segmental sagittal angle (SSA) were measured on lateral standing plain radiographs preoperatively (A) and postoperatively (B).

(A, B) Lumbar lordotic angle (LLA) was measured on lateral standing plain radiographs preoperatively and postoperatively.
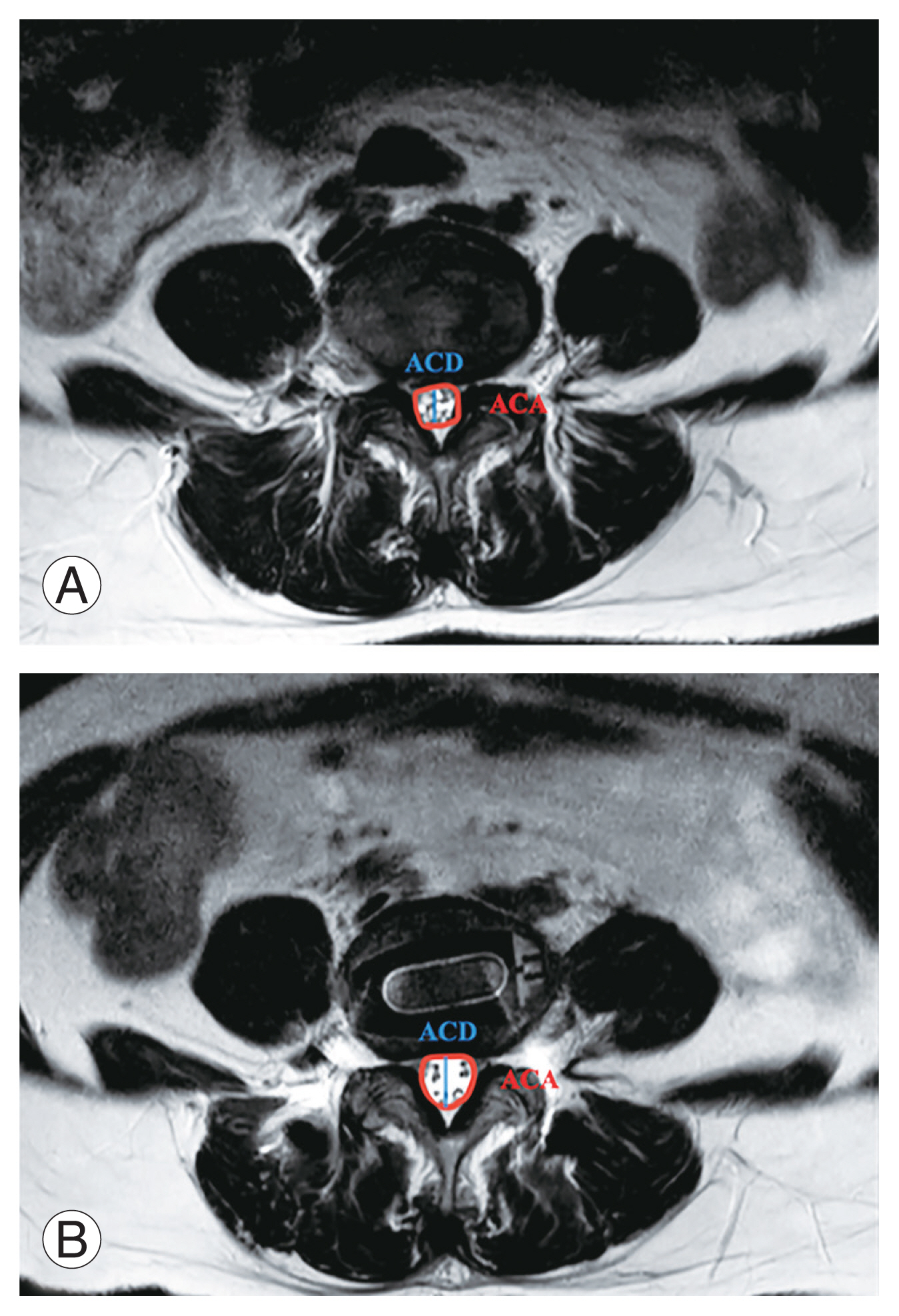
Magnetic resonance images (MRI) with a 1.5-Tesla unit (Aera, Siemens Medical Solutions; Erlangen, Bavaria, Germany) was obtained preoperatively and at 3 months postoperatively in all patients. The axial canal area (ACA) and axial canal diameter (ACD) were measured (Fig. 4). The ACA was the area of thecal sac measured at facet joint level on axial cut T2-weighted MRI. The ACD was measured as the length between posterior surface of the annulus and anterior surface of the ligamentum flavum. The radiographic parameters were evaluated on digital radiographic images presented on a picture archiving and communication system. The resolution of the radiographic caliper was 0.1 mm. Fusion was evaluated using the Bridwell fusion grading system on computer tomography (CT) scan. Grades 1 and 2 were defined as fused spinal construct. Cage subsidence was also assessed on CT scan and defined as adjacent endplate breaches >2 mm [16]. Each parameter was measured twice by two spine surgeons.
6. Statistical analyses
The statistical analyses were performed by IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). The change between the preoperative and postoperative clinical outcomes in VAS (leg), VAS (back), and ODI was analyzed by using repeated analysis of variance (ANOVA) and subgroup analysis by the Bonferroni test. The change between preoperative and postoperative radiographic values in ADH, PDH, FH, SSA, LLA, ACA, and ACD was analyzed by using ANOVA and subgroup analysis by the Bonferroni test. Intraobserver and interobserver reliabilities were evaluated using the Cronbach α. A p-value of <0.05 was used in all outcomes. A biostatistician performed the data analysis.
Results
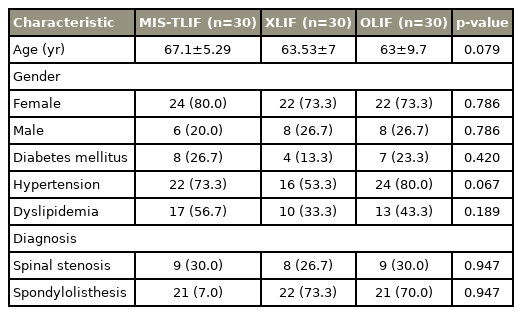
A total of 90 patients were included in this study. Thirty patients per group underwent MIS-TLIF, XLIF, and OLIF. Demographic data was shown in Table 1. The mean age of patients in MIS-TLIF, XLIF, and OLIF groups were 67.1±5.29, 63.53±7, and 63±9.7 years, respectively (p<0.079). There were no statistically significant differences among all groups in terms of underlying disease, baseline demographic data, preoperative clinical parameters, and radiographic parameters.
The perioperative comparison between all groups was shown in Table 2. There was a significant difference in blood loss between groups. Based on subgroup analysis, there was significantly less blood loss during OLIF than during MIS-TLIF and significantly less blood loss during XLIF than during MIS-TLIF.
Regarding the perioperative time, there was no statistical significance between each procedure. There was a significant difference regarding length of hospital stays (p<0.01). Based on subgroup analysis, there was a significantly shorter hospital stay during XLIF (3.6±0.62 days) versus MIS-TLIF (4.33±0.61 days) and a shorter hospital stay during OLIF (3.7±0.53 days) versus MIS-TLIF (4.33±0.61 days) (Table 2).
Concerning to complications, one patient in OLIF group developed deep vein thrombosis, and two patients had transient thigh pain in XLIF group.
1. Clinical evaluation
There was no significant difference between baseline preoperative clinical parameters (VAS scores of back and leg, ODI score) among MIS-TLIF, XLIF, and OLIF groups. The VAS score of back of all techniques showed significant improvement in any postoperative time point (1, 3, and 6 months and 1 year) compared with preoperative score of each procedure. There was no statistically significant difference between these groups (Table 3). The VAS score of the leg of all procedures was significantly decreased from preoperative period to any postoperative time point (1, 3, and 6 months and 1 year) of each technique. There was no statistically significant difference between the three groups (Table 3). The ODI score of all the procedures showed significant improvement in any postoperative period (1, 3, and 6 months and 1 year) compared with preoperative score of each technique. Subgroup analysis showed that the score of MIS-TLIF group significantly improved compared to XLIF group at 1-year postoperative time point (Table 3).
2. Radiological outcomes
There was no significant difference in baseline preoperative radiographic parameters among MIS-TLIF, XLIF, and OLIF. The ADH, PDH, FH, FA, SSA, LLA, ACA, and ACD were significantly improved postoperatively after all the procedures (Table 4). The interobserver agreement was at an almost-perfect level (kappa=0.81).
The ADH was significantly restored in all three groups, where MIS-TLIF, XLIF, and OLIF approaches yielded increases of 18.35%, 51.10%, and 45.61%, respectively. Subgroup analysis showed that the ADH significantly increased in XLIF and OLIF more than in MIS-TLIF (p<0.001).
The PDH was also significantly restored in all groups, where MIS-TLIF, XLIF, and OLIF yielded increases of 19.21%, 50.68%, and 42.45%, respectively. Subgroup analysis showed that the PDH significantly increased in XLIF and OLIF more than in MIS-TLIF (p<0.001).
The FH was significantly improved in all groups. Based on the subgroup analysis, XLIF significantly restored FH compared to MIS-TLIF (p<0.001). Likewise, OLIF significantly improved FH versus MIS-TLIF (p<0.001). XLIF and OLIF yielded increases of 22.75% and 29.47%, respectively. Nevertheless, no significant difference was seen in XLIF and OLIF groups (p=0.058).
Based on the subgroup analysis, there were no significant differences regarding the correction of SSA among all groups. Similarly, there were no significant differences regarding the restoration of LLA among all techniques based on subgroup analysis.
We found that ACA was significantly increased from preoperative to postoperative time point in MIS-TLIF by 211%, XLIF by 78.79%, and OLIF by 82.93%. Based on the subgroup analysis, the canal area was significantly increased more in MIS-TLIF than in XLIF (p<0.001) and OLIF (p<0.001) groups. No significant difference was seen between XLIF and OLIF groups.
The ACD was significantly restored from preoperative to postoperative period in MIS-TLIF, XLIF, and OLIF groups. Subgroup analysis demonstrated that the diameter significantly increased more in MIS-TLIF group than in XLIF and OLIF groups.
The fusion rate was not significantly different at 1-year evaluation. The MIS-TLIF group demonstrated fusion in 28/30 (93.3%), and XLIF and OLIF groups resulted in fusion in 29/30 (96.7%).
There was no statistically significant difference in subsidence rate at 1-year follow-up. Cage subsidence occurred in 43.33% (13/30), 43.33% (13/30), and 50% (15/30) of patients in MIS-TLIF, XLIF, and OLIF groups, respectively.
Discussion
MI lumbar interbody fusion has gained popularity in the treatment of degenerative lumbar spine diseases due to favorable results with less collateral damage to paraspinal muscles and ligaments. MIS-TLIF, XLIF, and OLIF are currently considered as promising treatment options. As with open TLIF surgery, the MIS-TLIF can directly decompress neural element with reported better short-term outcomes following the surgery including less bleeding, postoperative pain, hospitalization, and complications [17–19]. Lateral lumbar interbody fusion (LLIF), including OLIF and XLIF, provides indirect decompression to neural elements by ligamentotaxis and also corrects deformity in sagittal and coronal planes [12,20]. Many studies demonstrated significant improvement of clinical and radiographic outcomes following LLIF [8,12,21]. Although several studies indicated that MIS-TLIF, XLIF, and OLIF provided good results, only a few studies have focused on comparison of the outcomes following these various MI spinal surgery techniques. In addition, none of the reports compared clinical and radiographic outcomes among these three procedures [9–13]. To the best of our knowledge, our study was the first to evaluate clinical and radiographic outcomes among these three procedures.
Regarding clinical outcomes, we discovered that all three groups were significantly improved in the outcomes at all studied time points compared with preoperative period, as evidenced by better VAS score of back and leg and ODI in this study. These findings were consistent with many previous reports [2,5,22]. In addition, we found that clinical outcomes of all the procedures were not significant differences at any postoperative period except ODI score at 1 year after surgery, which showed that the score of MIS-TLIF group was better than XLIF group. However, the score in these two groups improved more than 90% from preoperative baseline, which represented excellent outcomes. Concerning to outcomes of the LLIF procedures, Li et al. [23] found different results. They reported that VAS and ODI scores of OLIF group were better than XLIF group, which might be due to complications related to psoas muscle injury in the XLIF group.
The radiographic outcomes regarding ADH, PDH, FH, ACA, and ACD were significantly improved in all the three techniques. The restorations of ADH, PDH, and FH were significantly more favorable in both OLIF and XLIF than in MIS-TLIF in this study, which were in accordance with previous studies [11,24]. This is because surgeon can insert larger and higher size of cage into disc space in XLIF and OLIF groups. Subgroup analysis demonstrated that improvement of disc height after XLIF and OLIF was comparable. These findings were consistent with a study reported by Li et al. [23].
In contrast, the ACA and ACD were significantly improved better in MIS-TLIF than the other two groups. This is due to the effect of direct decompression from MIS-TLIF, which directly removed ipsilateral posterior bony elements and ligamentum flavum to decompress and expand the spinal canal. In contract with MIS-TLIF, XLIF, and OLIF procedures achieve indirect decompression of the spinal canal by implantation of interbody cage, which resulted in unbuckling of ligamentum flavum, stretching of ligaments, and increasing disc height. These results were similar to a randomized controlled trial reported by Isaacs et al. [10]. However, despite lesser axial canal dimensions achieved from indirect decompression in XLIF and OLIF, the clinical improvement was favorable and comparable to direct decompression effect from MIS-TLIF. This is due to the disc and FH restorations from a larger and higher size of cage that maximized the ligamentotaxis effect and subsequently indirectly decompressed the spinal canal.
Our study demonstrated an improvement of overall lumbar lordosis postoperatively in all groups. Nevertheless, there was no statistically significant difference in LLA and SSA among all groups, which was contrary to a previous study [24] that reported better correction of SSA in XLIF than MIS-TLIF. The lesser degree of sagittal alignment correction obtained in this study could be explained by us performing only a single-level fusion procedure. In addition, the cage characteristic played an important role in creating lumbar lordosis. In this study, there was application of neither the hyperlordotic cage in LLIF nor the banana-shaped cage in MIS-TLIF that could achieve more lordosis when located anteriorly.
The transient anterior thigh pain following XLIF procedure in this study (6.6%) was lower than previously reported in the systematic review by Gammal et al. [25], which ranged from 9.3% to 43.0%. As expected, the operative blood loss and length of hospital stay were lower in LLIF than in MIS-TLIF possibly because LLIF does not require dissection through paraspinal muscle and also avoids injury to epidural venous plexus or bone bleeding from the direct decompression procedure. These findings were consistent with the prospective study by Sembrano et al. [9].
This study has some limitations. This study was a retrospective, nonrandomized single-center study. We did not include preoperative MRI data for the propensity score matching that might cause selection bias. Moreover, this study included only L4–5 lumbar fusion. The clinical results, radiographic outcomes, and complications may differ when other spinal levels or multilevel were operated. Further studies with prospective, longer follow-up periods, and larger patient cohorts are warranted.
Conclusions
MIS-TLIF, XLIF, and OLIF are safe and effective MI procedures for treating lumbar degenerative diseases. XLIF and OLIF can achieve clinical outcomes equivalent to MIS-TLIF. XLIF and OLIF showed less blood loss, shorter hospital stays, and superior improvement in restoring DH and FH than MIS-TLIF. In single-level L4–5, the restoration of sagittal alignment was similar between these three techniques.
Acknowledgments
The authors thank Thanachaporn Kittipibul, MD., Mrs. Dollapas Punpanich and Chulalongkorn University Spine Team for their support of this study.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Wicharn Yingsakmongkol: conceptualization, resources; Khanathip Jitpakdee: data collection; Panapol Varakornpipat: data collection, writing (original draft); Chitapoom Choentrakool: data analysis; Teerachat Tanasansomboon: writing (review and editing); Worawat Limthongkul: supervision, resources; Weerasak Singhatanadgige: methodology, resources; Vit Kotheeranurak: writing (review and editing), supervision.